Bcl-2 and Bcl-xL: Masters of Cell Survival from Apoptosis Mechanisms to Targeted Cancer Therapy
This article provides a comprehensive analysis of the Bcl-2 protein family, focusing on the pivotal roles of Bcl-2 and Bcl-xL as key regulators of the intrinsic apoptosis pathway.
Bcl-2 and Bcl-xL: Masters of Cell Survival from Apoptosis Mechanisms to Targeted Cancer Therapy
Abstract
This article provides a comprehensive analysis of the Bcl-2 protein family, focusing on the pivotal roles of Bcl-2 and Bcl-xL as key regulators of the intrinsic apoptosis pathway. Tailored for researchers and drug development professionals, it explores the foundational biology governing these anti-apoptotic proteins, examines the development and application of BH3-mimetic therapeutics like venetoclax, and addresses challenges such as treatment resistance and toxicity. The content further synthesizes validation data from clinical trials and compares the therapeutic landscapes of targeting different Bcl-2 family members, offering a holistic view of their potential in precision oncology and other therapeutic areas.
The Fundamental Biology of Bcl-2 and Bcl-xL: Guardians Against Programmed Cell Death
The discovery of B-cell lymphoma 2 (Bcl-2) represents a paradigm shift in cancer biology, establishing that oncogenes can promote tumorigenesis by inhibiting cell death rather than stimulating proliferation. This review chronicles the seminal journey from the initial identification of the t(14;18) chromosomal translocation in follicular lymphoma to the elucidation of Bcl-2's fundamental role as an anti-apoptotic regulator. We examine the key experimental methodologies that defined Bcl-2 function, detail the structural basis of its mechanism within the Bcl-2 protein family, and contextualize these findings within the broader field of apoptosis research. The development and clinical application of Bcl-2 inhibitors are discussed as the direct therapeutic culmination of this foundational research, highlighting the critical pathway from basic biological discovery to targeted cancer therapy.
Prior to the discovery of Bcl-2, the canonical function of oncogenes was understood primarily through their capacity to drive cellular proliferation. The identification of the Bcl-2 oncogene in the context of follicular lymphoma revealed a fundamentally different oncogenic mechanism: the blockade of programmed cell death (apoptosis). This discovery established that tumors could arise not only through accelerated cell division but also through failed cell elimination, reshaping the conceptual framework of cancer pathogenesis and opening new avenues for therapeutic intervention [1] [2]. This review traces the pivotal discoveries that linked a specific chromosomal translocation to the aberrant regulation of a fundamental cellular process, ultimately positioning Bcl-2 and its relatives, including Bcl-xL, as central regulators of cell survival and promising therapeutic targets.
The Initial Discovery: Chromosomal Translocations in Lymphoma
The foundational discovery of Bcl-2 emerged from cytogenetic studies of B-cell malignancies. In 1984, researchers identified a frequent chromosomal abnormality in follicular lymphoma cells: a balanced, reciprocal translocation between chromosomes 14 and 18, denoted as t(14;18)(q32;q21) [1] [2]. This translocation was subsequently found in a significant proportion of diffuse large B-cell lymphoma (DLBCL) and chronic lymphocytic leukemia (CLL) cases [2].
Molecular Consequences of t(14;18)
At the molecular level, the t(14;18) translocation juxtaposes the BCL2 gene from chromosome 18 with the immunoglobulin heavy chain (IGH) locus on chromosome 14 [3] [2]. This genetic repositioning places the BCL2 coding sequence under the control of the potent IGH enhancer region, leading to its constitutive and deregulated overexpression in B-cells [3]. This gene fusion product is detectable on cytogenetics or karyotype analysis of affected cells and serves as a diagnostic marker [4].
Table 1: Key Chromosomal Translocations in Hematologic Malignancies
| Disease | Chromosomal Abnormality | Affected Gene(s) | Molecular Consequence |
|---|---|---|---|
| Follicular Lymphoma | t(14;18)(q32;q21) | BCL2 and IGH | BCL2 overexpression via IGH enhancer |
| Chronic Myelogenous Leukemia (CML) | t(9;22)(q34;q11) | BCR and ABL | Generation of BCR-ABL fusion oncogene |
| Acute Promyelocytic Leukemia (APL) | t(15;17)(q21;q21) | PML and RARA | Generation of PML-RARA fusion oncogene |
| B-cell Acute Lymphoblastic Leukemia (ALL) | t(1;19)(q23;p13) | E2A and PBX1 | Generation of E2A-PBX1 fusion oncogene |
Unlike other known oncogenes that accelerated cell division, initial observations indicated that BCL2 overexpression did not directly promote proliferation. Instead, it conferred a remarkable survival advantage to lymphocytes by extending their lifespan, suggesting a novel mechanism of oncogenesis centered on the inhibition of a normal cell death program [1].
Establishing the Anti-Apoptotic Function: Key Experimental Evidence
The hypothesis that Bcl-2 functioned by inhibiting cell death was confirmed through a series of critical experiments in the late 1980s and early 1990s. These studies transitioned Bcl-2 from a genetic aberration associated with cancer to a fundamental regulator of a core biological process.
Critical Experimental Workflows and Findings
The following diagram illustrates the logical flow and conclusions of the key experiments that established Bcl-2's anti-apoptotic function.
Diagram 1: Experimental Workflow Establishing Bcl-2 Function. This flowchart summarizes the sequence of key experiments that defined Bcl-2 as an inhibitor of apoptosis, culminating in a paradigm shift in oncology.
In Vitro Cytokine Deprivation Models
A pivotal experiment involved interleukin-3 (IL-3)–dependent hematopoietic cell lines. When deprived of IL-3, control cells rapidly died. In contrast, cells engineered to overexpress Bcl-2 did not proliferate but entered a quiescent state and remained viable for extended periods. The critical finding was that upon reintroduction of IL-3, these cells resumed proliferation, demonstrating that Bcl-2 had not induced a transformed state but had prevented death, allowing for survival until growth signals were restored [1].
Transgenic Mouse Models
Mice genetically engineered to overexpress Bcl-2 in B-lymphocytes displayed a dramatic accumulation of these cells due to extended survival rather than increased division. When these Bcl-2 transgenic mice were crossed with mice expressing the MYC oncogene (a known driver of proliferation), they rapidly developed aggressive lymphomas [1]. This synergy powerfully demonstrated that oncogenic collaboration could occur between a pro-proliferation signal (MYC) and an anti-death signal (Bcl-2).
Discovery of Bcl-2 Family Members and the Dimerization Model
The discovery of BAX, a protein that co-immunoprecipitated with Bcl-2, was a breakthrough [1]. It was the first identified homolog and had a function antagonistic to Bcl-2. This led to the proposal of a heterodimerization model, where the balance between death antagonists (like Bcl-2) and death agonists (like Bax) determined cellular fate [2]. This model was further supported by structural studies revealing a hydrophobic groove on anti-apoptotic proteins as the main protein-protein interaction site for binding the BH3 domain of pro-apoptotic partners [2].
Table 2: Summary of Key Functional Experiments on Bcl-2
| Experimental System | Key Observation | Interpretation |
|---|---|---|
| IL-3 Dependent Cell Lines | Bcl-2 expression allowed survival after growth factor withdrawal. | Bcl-2 prevents cell death but does not drive proliferation. |
| Bcl-2 Transgenic Mice | Accumulation of B-cells; enhanced survival of lymphocytes in vitro. | Bcl-2 inhibits physiological cell death pathways in vivo. |
| Bcl-2/MYC Double Transgenic Mice | Rapid onset of aggressive B-cell lymphoma. | Bcl-2 collaborates with a pro-proliferative oncogene. |
| Yeast Two-Hybrid / Co-IP | Identification of Bax binding to Bcl-2. | Bcl-2 functions through protein-protein interactions with homologs. |
The Scientist's Toolkit: Key Research Reagents and Models
Table 3: Essential Reagents and Models for Bcl-2 Family Research
| Reagent/Model | Description | Primary Function in Research |
|---|---|---|
| ABT-737 | Small-molecule BH3-mimetic inhibitor of Bcl-2, Bcl-xL, and Bcl-w. | Tool compound for validating Bcl-2 family dependence in cancer models. |
| Venus/mCherry Fluorescent Protein Fusions | N-terminal tags for Bcl-2 family proteins (e.g., Venus-Bcl-2, mCherry-Bim). | Visualizing protein localization and interactions in live cells via microscopy. |
| BH3 Peptides | Synthetic peptides corresponding to BH3 domains of pro-apoptotic proteins. | Profiling dependencies on anti-apoptotic proteins in mitochondrial assays. |
| Bcl-2 Transgenic Mice | Mice overexpressing Bcl-2 in specific lineages (e.g., B-cells). | Studying the impact of suppressed apoptosis on development and tumorigenesis. |
| BAX/BAK Double Knockout Mice | Mice lacking key pro-apoptotic effector proteins. | Defining the essential gateway to intrinsic apoptosis. |
| Navitoclax (ABT-263) | Orally available analog of ABT-737; inhibits Bcl-2, Bcl-xL, Bcl-w. | Preclinical and clinical proof-of-concept for BH3-mimetic therapy. |
The Bcl-2 Protein Family: Regulators of Mitochondrial Apoptosis
The initial discovery of Bcl-2 and Bax paved the way for identifying an entire family of regulatory proteins. The Bcl-2 family is now known to comprise approximately 20 members in humans, which can be divided into three functional subgroups based on their structure and function [2]:
- Anti-apoptotic proteins (e.g., Bcl-2, Bcl-xL, Mcl-1, Bcl-w), which contain four BH domains (BH1-BH4) and suppress cell death.
- Pro-apoptotic effector proteins (e.g., Bax, Bak, Bok), which contain multiple BH domains and are responsible for mitochondrial outer membrane permeabilization (MOMP).
- BH3-only proteins (e.g., Bim, Bid, Puma, Bad, Noxa), which are sensors of cellular stress and initiate apoptosis by engaging the other two groups.
The Molecular Mechanism of Apoptotic Control
The primary function of the Bcl-2 family is to regulate the intrinsic (mitochondrial) pathway of apoptosis. Under normal conditions, anti-apoptotic proteins like Bcl-2 and Bcl-xL bind and sequester pro-apoptotic BH3-only proteins and the activated forms of Bax/Bak, thereby preserving mitochondrial integrity [1]. In response to cellular damage or stress (e.g., DNA damage, growth factor withdrawal), the expression or activity of BH3-only proteins is elevated. These proteins then neutralize the anti-apoptotic members, freeing Bax and Bak to oligomerize and form pores in the mitochondrial outer membrane, a process known as mitochondrial outer membrane permeabilization (MOMP) [5] [1]. MOMP leads to the release of cytochrome c and other factors into the cytosol, triggering caspase activation and orderly cell dismantling [2].
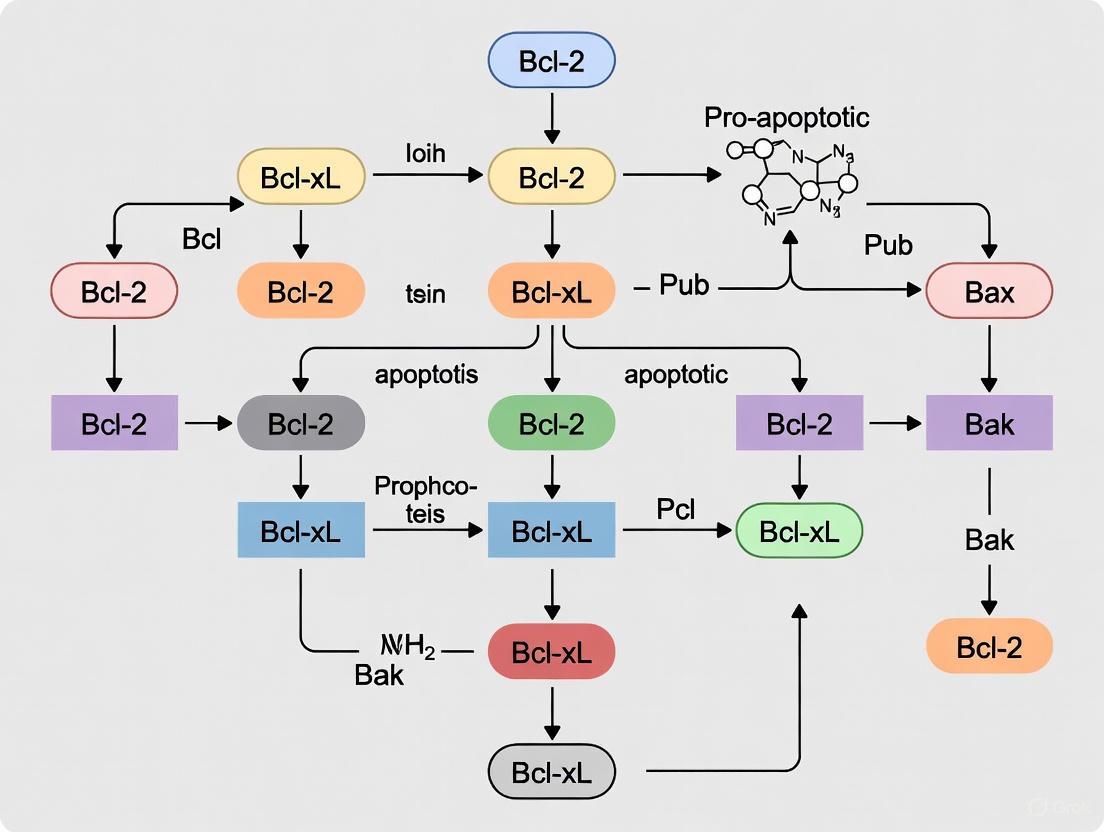
The following diagram illustrates the core regulatory network of the Bcl-2 protein family and the commitment to apoptosis.
Diagram 2: Bcl-2 Family Regulation of Intrinsic Apoptosis. Cellular stress activates BH3-only proteins, which inhibit anti-apoptotic members and/or directly activate Bax/Bak. This leads to MOMP, cytochrome c release, and caspase-dependent apoptosis.
From Mechanism to Therapy: The Development of BH3-Mimetics
The elucidation of Bcl-2's role in cancer and the structural understanding of its hydrophobic groove enabled the rational design of a new class of drugs: BH3-mimetics. These small molecules are designed to mimic the function of native BH3-only proteins by binding to the hydrophobic groove of anti-apoptotic proteins, thereby displacing pro-apoptotic partners and triggering apoptosis in cancer cells [2].
The Clinical Translation Timeline
The development of BH3-mimetics marks a direct therapeutic application of the foundational research on Bcl-2.
- ABT-737 (2005): The first potent and specific small-molecule inhibitor of Bcl-2, Bcl-xL, and Bcl-w, developed using NMR-based screening and structure-based design [2].
- Navitoclax (ABT-263): An orally available derivative of ABT-737 that entered clinical trials. It showed promise but caused dose-limiting thrombocytopenia due to on-target inhibition of Bcl-xL, which is critical for platelet survival [3] [2].
- Venetoclax (ABT-199): A highly selective Bcl-2 inhibitor engineered to spare Bcl-xL. This selectivity avoided the thrombocytopenia associated with navitoclax [3]. Venetoclax received FDA approval in 2016 for the treatment of CLL with 17p deletion, becoming the first FDA-approved Bcl-2 inhibitor and validating Bcl-2 as a cancer drug target [3] [2].
The journey of Bcl-2 from a chromosomal translocation in a B-cell lymphoma to a central regulator of apoptosis and a validated drug target exemplifies the power of basic biological research to transform clinical practice. The initial discovery that Bcl-2 inhibited cell death established a new oncogenic paradigm and spurred decades of research into the Bcl-2 protein family. The rigorous experimental characterization of its function, interactions, and structure provided the essential blueprint for targeted therapeutic development. The successful clinical application of venetoclax and the ongoing development of inhibitors targeting other anti-apoptotic family members like Bcl-xL and Mcl-1 stand as a testament to the profound impact of understanding the fundamental historical context and mechanistic biology of the Bcl-2 family.
The B-cell lymphoma 2 (BCL-2) protein family represents a critical class of regulators that determine cellular fate through the intrinsic apoptotic pathway. The founding member, BCL-2, was first identified in 1984 as the gene involved in the t(14;18) chromosomal translocation found in most follicular lymphomas [6]. This discovery revealed the first oncogene that promotes cancer by inhibiting programmed cell death rather than stimulating proliferation [6]. Subsequent research has identified approximately 20 proteins in the human BCL-2 family, which are characterized by the presence of BCL-2 homology (BH) domains and classified into three functional groups: anti-apoptotic, pro-apoptotic effector, and BH3-only proteins [6] [7]. The structural intricacies of these proteins, particularly their BH domains and the hydrophobic groove they form, constitute the fundamental mechanism through which BCL-2 and BCL-XL inhibit mitochondrial apoptosis, making them compelling targets for therapeutic intervention in cancer and other diseases [6] [8].
Structural Organization of BCL-2 Family Proteins
The BCL-2 Homology (BH) Domains
BCL-2 family proteins are defined by the presence of up to four conserved α-helical motifs known as BCL-2 homology (BH) domains. These structural elements facilitate the protein-protein interactions that govern apoptotic regulation [7] [8]. The BH domains serve distinct functions:
BH4 Domain: Located at the N-terminus, this domain is primarily found in anti-apoptotic members and is crucial for their survival function. Deletion of BH4 can convert BCL-2 from anti-apoptotic to pro-apoptotic [7] [9]. The BH4 domain also interacts with effector molecules outside the BCL-2 family to participate in angiogenesis, autophagy, and other pathways [7].
BH3 Domain: An amphipathic α-helix that serves as the primary interaction motif for both pro- and anti-apoptotic family members. This domain is essential for the pro-apoptotic function of BH3-only proteins and for dimer formation [6] [10].
BH1 and BH2 Domains: These domains, along with BH3, form the characteristic hydrophobic surface groove that binds to BH3 domains of partner proteins [6] [8].
The multi-domain anti-apoptotic proteins (BCL-2, BCL-XL, MCL-1, BCL-W, BFL-1, BCL-B) typically contain all four BH domains, while the pro-apoptotic effectors (BAX, BAK, BOK) possess BH1-3 domains but lack BH4 [6] [7]. BH3-only proteins (BID, BIM, BAD, PUMA, NOXA, etc.) share sequence homology only within the BH3 region [6].
Table 1: BCL-2 Family Protein Classification and Domain Architecture
| Subfamily | Representative Members | BH Domains Present | Transmembrane Domain | Primary Function |
|---|---|---|---|---|
| Anti-apoptotic | BCL-2, BCL-XL, MCL-1, BCL-W | BH1, BH2, BH3, BH4 | Yes [8] | Inhibit mitochondrial outer membrane permeabilization (MOMP) |
| Pro-apoptotic Effectors | BAX, BAK, BOK | BH1, BH2, BH3 | Yes (BAX translocates upon activation) [10] | Execute MOMP through oligomerization |
| BH3-only | BID, BIM, BAD, PUMA, NOXA | BH3 only | Some members (e.g., BID) [8] | Initiate apoptosis by inhibiting anti-apoptotic proteins or directly activating effectors |
The Hydrophobic Groove: Architecture and Function
The three-dimensional structure of multi-domain BCL-2 family members features a characteristic fold consisting of eight α-helices (α1-α8) arranged around two central hydrophobic helices (α5 and α6) [8]. The BH1, BH2, and BH3 domains collectively form a pronounced hydrophobic groove on the protein surface, which serves as the primary interaction site for BH3 domain binding [6] [8].
This groove contains four hydrophobic pockets (P1-P4) that accommodate the hydrophobic residues of the BH3 α-helix from binding partners [6]. The groove is structurally conserved across anti-apoptotic family members, though sequence variations confer binding specificity for different BH3-only proteins [6]. In the inactive state of pro-apoptotic BAX, its C-terminal transmembrane domain (α9-helix) is folded into this hydrophobic groove, preventing its activation [11].
Molecular Mechanism of Apoptosis Inhibition
Regulation of Mitochondrial Outer Membrane Permeabilization (MOMP)
The hydrophobic groove of anti-apoptotic BCL-2 proteins is the structural basis for their function as apoptosis inhibitors. These proteins localize to the outer mitochondrial membrane (OMM) via their C-terminal transmembrane domains, where they regulate mitochondrial outer membrane permeabilization (MOMP) [6] [10]. MOMP represents the "point of no return" in intrinsic apoptosis, leading to cytochrome c release and caspase activation [10].
BCL-2 and BCL-XL prevent MOMP by sequestering pro-apoptotic family members through groove-BH3 interactions in two primary mechanisms:
Neutralization of BH3-only proteins: Anti-apoptotic proteins bind and neutralize the activator BH3-only proteins (e.g., BIM, BID), preventing them from activating BAX and BAK [6] [10].
Direct inhibition of BAX and BAK: BCL-2 and BCL-XL can directly bind to the activated forms of BAX and BAK, preventing their oligomerization and pore formation [10] [12].
The binding specificity varies among family members; for example, BCL-XL shows high affinity for BIM and BAD BH3 domains, while MCL-1 preferentially binds NOXA and BIM [6].
BH3:Groove Interactions in Apoptotic Regulation
The interaction between the hydrophobic groove of multi-domain BCL-2 proteins and the BH3 α-helix of binding partners is the fundamental regulatory mechanism in apoptosis control. Structural studies reveal that this interaction involves the burial of hydrophobic residues from the BH3 helix into the pockets of the groove, complemented by electrostatic interactions at the helix termini [10] [8].
A key mechanistic insight involves the role of these interactions in BAX/BAK activation. During apoptosis, activator BH3-only proteins (like BIM or tBID) bind to BAX/BAK, triggering a conformational change that includes exposure of their BH3 domain [10]. This exposed BH3 domain can then bind to the hydrophobic groove of another BAX/BAK molecule, forming a symmetric homodimer through BH3:groove interactions that nucleate further oligomerization into the apoptotic pore complex [10].
BCL-2 and BCL-XL counteract this process by capturing the BH3 domains of activator proteins or activated BAX/BAK before they can engage in pro-apoptotic oligomerization [10].
Diagram 1: Intrinsic Apoptosis Regulation. Cellular stress activates BH3-only proteins that either neutralize anti-apoptotic proteins or directly activate BAX/BAK to induce MOMP [6] [10].
Therapeutic Targeting of the Hydrophobic Groove
BH3-Mimetics: Mechanism and Clinical Applications
The structural understanding of BH3:groove interactions has enabled the development of BH3-mimetics - small molecules that occupy the hydrophobic groove of anti-apoptotic BCL-2 proteins, displacing pro-apoptotic partners and reactivating apoptosis in cancer cells [6].
Venetoclax (ABT-199) represents the first successful BH3-mimetic, specifically designed to target BCL-2 with high affinity while sparing BCL-XL to avoid platelet toxicity [6]. It was developed through structure-based design following the discovery of earlier inhibitors like ABT-737 and navitoclax (ABT-263) [6]. Venetoclax has received FDA and EMA approval for treating chronic lymphocytic leukemia (CLL) and acute myeloid leukemia (AML) [6] [7].
Following venetoclax's success, several chemically similar BCL-2 inhibitors such as sonrotoclax and lisaftoclax are undergoing clinical evaluation, both as monotherapies and in combination regimens [6].
Quantitative Binding Affinities of BH3-Mimetics
Table 2: Experimentally Determined Binding Affinities for BCL-2 Family Interactions and Inhibitors
| Ligand/Target | BCL-2 Family Member | Affinity (Kd or IC50) | Experimental Method | Biological/Therapeutic Significance |
|---|---|---|---|---|
| Venetoclax | BCL-2 | <1 nM [6] | NMR-based screening, parallel synthesis, structure-based design [6] | Selective BCL-2 inhibition; approved for CLL and AML |
| ABT-737 | BCL-XL | Nanomolar range [6] | NMR-based screening, parallel synthesis [6] | Prototypic BH3-mimetic; tool compound for research |
| Navitoclax | BCL-2/BCL-XL/BCL-w | Nanomolar affinity [6] | Modification of ABT-737 for oral availability [6] | Clinical development limited by thrombocytopenia |
| KSHV BCL-2 | BAK1 BH3 | Nanomolar affinity [8] | Binding assays | Viral mimicry of human BCL-2; independent anti-death activity |
| KSHV BCL-2 | BAX BH3 | 980 nM [8] | Binding assays | Viral immune evasion mechanism |
Challenges and Novel Approaches in BH3-Mimetic Development
Despite the success of BCL-2-specific inhibitors, targeting other anti-apoptotic family members has proven challenging. BCL-XL inhibition causes dose-limiting thrombocytopenia due to BCL-XL's essential role in platelet survival, while MCL-1 inhibition has been associated with cardiac toxicity [6].
Novel strategies are emerging to overcome these limitations:
PROTACs (Proteolysis Targeting Chimeras): Designed to achieve tumor-specific degradation of BCL-XL or MCL-1, potentially reducing on-target toxicities [6].
Antibody-Drug Conjugates (ADCs): Enable selective delivery of BCL-XL or MCL-1 inhibitors to tumor cells [6].
Computational Peptide Design: In silico approaches are being used to develop cyclic peptides that target the hydrophobic groove of BAX, inhibiting its pro-apoptotic function [11].
Diagram 2: Therapeutic Development Pipeline. Structure-based drug design has progressed from initial screening to approved BH3-mimetics, with novel approaches now emerging [6] [11].
Experimental Methodologies for Studying BH Domains and Groove Interactions
Structural Biology Techniques
Nuclear Magnetic Resonance (NMR) Spectroscopy: NMR-based screening was instrumental in the development of ABT-737, the progenitor of venetoclax. This technique identified fragments that bind proximally in the hydrophobic groove, which were then linked to create high-affinity inhibitors [6].
X-ray Crystallography: Has provided high-resolution structures of BCL-XL, BCL-2, and other family members, revealing the detailed architecture of the hydrophobic groove and its interaction with BH3 peptides [6] [8]. These structures show the precise arrangement of the eight-helix bundle and the four hydrophobic pockets (P1-P4) that accommodate BH3 residues [6].
Computational Design and Molecular Dynamics
Recent advances employ molecular dynamics (MD) simulations to study the stability of BCL-2 protein complexes and design novel inhibitors:
Rational Peptide Design: Starting from crystal structures of protein complexes, peptides are designed to bind specific sites on BCL-2 family proteins, then optimized through single-point mutations [11].
Binding Free Energy Calculations: MD simulations estimate binding affinities of designed peptides, prioritizing candidates for experimental testing [11].
Digital Twin Development: Integration of computational and experimental data to simulate effects of peptide-based drugs on targets like BAX [11].
For BAX inhibition studies, computational approaches have designed cyclic peptides that bind to either the canonical hydrophobic groove (BH1 domain) or the outside of the BH3 domain (α2-helix), restricting flexibility of the α1-α2 loop and modulating the "trigger button" site associated with toxicity [11].
Binding Assays and Functional Measurements
Surface Plasmon Resonance (SPR) and Isothermal Titration Calorimetry (ITC): Quantify binding affinities between BH3 peptides and anti-apoptotic proteins, providing the quantitative data essential for drug development [6] [8].
Cytochrome c Release Assays: Functional measurements of MOMP in isolated mitochondria or cell-based systems validate the physiological relevance of BH3:groove interactions [6] [10].
BH3 Profiling: Measures mitochondrial sensitivity to synthetic BH3 peptides as a functional readout of BCL-2 family dependence in cancer cells [6].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Studying BH3:Groove Interactions
| Reagent/Tool | Category | Function/Application | Example Specific Reagents |
|---|---|---|---|
| Recombinant BCL-2 Family Proteins | Protein Tools | Structural studies, in vitro binding assays | BCL-2, BCL-XL, MCL-1, BAX, BAK [6] [11] |
| BH3 Peptides | Peptide Tools | Mapping interactions, BH3 profiling | BIM BH3, BID BH3, BAD BH3, PUMA BH3 [6] [10] |
| BH3-Mimetic Compounds | Small Molecule Inhibitors | Mechanistic studies, combination therapies | ABT-737 (tool compound), Venetoclax (clinical) [6] |
| Cyclic Peptides | Novel Modalities | Inhibiting protein-protein interactions | Computationally designed BAX inhibitors [11] |
| Structure Determination Platforms | Structural Biology | Elucidating 3D structures of complexes | X-ray crystallography, NMR spectroscopy [6] [8] |
| Molecular Dynamics Software | Computational Tools | Simulating dynamics and binding interactions | GROMACS, AMBER, CHARMM [11] |
The structural insights into BH domains and the hydrophobic groove mechanism have revolutionized our understanding of apoptotic regulation and provided a robust platform for targeted drug discovery. The precise molecular characterization of how anti-apoptotic proteins like BCL-2 and BCL-XL utilize their hydrophobic grooves to sequester pro-apoptotic partners has enabled the development of rationally designed BH3-mimetics, exemplified by the clinical success of venetoclax. Ongoing research continues to address the challenges of targeting other anti-apoptotic family members, employing novel modalities such as PROTACs, antibody-drug conjugates, and computationally designed peptides. As structural biology techniques advance and computational approaches become more sophisticated, the potential for developing more selective and effective therapeutics that modulate the fundamental apoptotic switch continues to expand, offering promising avenues for cancer treatment and beyond.
The B-cell lymphoma 2 (Bcl-2) family of proteins constitutes a critical regulatory network that determines cellular life or death by controlling mitochondrial outer membrane permeabilization (MOMP), the irreversible commitment point in the intrinsic apoptotic pathway [13] [14]. This network integrates diverse cellular stress signals, including DNA damage, oxidative stress, and growth factor withdrawal, to decide whether a cell should undergo programmed cell death. Defects in this regulatory system are implicated in various diseases, most notably cancer, where apoptosis evasion is a hallmark of malignancy [15] [16]. Therapeutically targeting this network has emerged as a promising strategy for cancer treatment, with Bcl-2 inhibitors like venetoclax demonstrating significant clinical success in hematological malignancies [16] [17].
Within the context of broader apoptosis research, the roles of Bcl-2 and Bcl-xL as key antiapoptotic regulators have been extensively characterized. These proteins function as crucial survival factors in numerous cell types, and their overexpression is a common mechanism by which cancer cells resist apoptosis [18] [19]. This technical guide comprehensively details the molecular composition, regulatory mechanisms, and experimental methodologies for investigating this tripartite apoptotic switch, with particular emphasis on Bcl-2 and Bcl-xL functionality.
Bcl-2 Family Organization: A Tripartite System
The Bcl-2 family is structurally and functionally categorized into three distinct classes that engage in a complex network of interactions to regulate MOMP [13] [20]. The relative concentrations and binding affinities between these factions ultimately determine cellular fate.
Table 1: Bcl-2 Family Protein Classification and Functions
| Class | Representative Members | BH Domain Profile | Primary Function |
|---|---|---|---|
| Antiapoptotic | Bcl-2, Bcl-xL, Mcl-1, Bcl-w, A1 | BH1-4 | Bind and inhibit proapoptotic members; promote cell survival |
| Effector Proapoptotic | Bax, Bak, Bok | BH1-3 | Mediate MOMP through oligomerization and pore formation |
| BH3-only Proapoptotic | Bid, Bim, Puma, Bad, Noxa, Hrk | BH3 only | Sense cellular stress and regulate antiapoptotics/effectors |
Antiapoptotic Members: Guardians of Survival
Antiapoptotic proteins, including Bcl-2 and Bcl-xL, are characterized by the presence of all four Bcl-2 homology (BH) domains (BH1-BH4) [13]. These proteins promote cell survival by directly binding and inhibiting their proapoptotic counterparts. Bcl-2 and Bcl-xL are particularly noteworthy for their established roles in inhibiting CD95-mediated apoptosis in "type II" cells by preventing mitochondrial release of Smac/DIABLO and subsequent inactivation of X-linked inhibitor-of-apoptosis protein (XIAP) [18]. Structurally, these proteins contain a hydrophobic groove that serves as a docking site for the BH3 helices of proapoptotic family members, thereby sequestering them and maintaining mitochondrial integrity [13].
Effector Proapoptotic Members: Executioners of MOMP
The multidomain proapoptotic effectors Bax and Bak are essential for MOMP execution [14]. In response to apoptotic signals, these proteins undergo conformational activation, mitochondrial translocation, and oligomerization to form pores in the mitochondrial outer membrane. These pores facilitate the release of intermembrane space proteins, including cytochrome c and SMAC, which activate the caspase cascade and ultimately lead to apoptotic cell death [13] [14]. Bcl-2 and Bcl-xL directly interact with Bax and Bak to prevent their activation, representing a crucial mechanism of apoptosis inhibition [18] [13].
BH3-only Proteins: Sentinels of Cellular Stress
BH3-only proteins function as specialized sensors for diverse apoptotic stimuli [13]. They are further subdivided based on their mode of action:
- Activators (e.g., Bim, Bid, Puma): Directly bind to and activate Bax/Bak
- Sensitizers (e.g., Bad, Noxa, Hrk): Bind to antiapoptotic proteins, displacing bound activators and effectors
The specific binding profiles of BH3-only proteins create a dependency pattern that informs therapeutic targeting. For instance, Bad preferentially binds Bcl-2 and Bcl-xL, while Noxa selectively targets Mcl-1 and A1 [13].
Molecular Mechanisms Governing the Apoptotic Switch
Models of Bcl-2 Family Regulation
Several models have been proposed to explain how Bcl-2 family interactions regulate MOMP:
- Direct Activation Model: Activator BH3 proteins directly bind and conformationally activate Bax and Bak, while sensitizer BH3 proteins neutralizes antiapoptotics [13].
- Displacement Model: Bax and Bak are constitutively active but restrained by antiapoptotics; BH3 proteins displace them to induce MOMP [13].
- Unified Model: Incorporates features of both models, proposing that antiapoptotics sequester activators (mode 1) and active Bax/Bak (mode 2), with mode 2 inhibition being more resistant to disruption [13] [21].
Research indicates that the unified model best explains the bistable behavior observed in the Bcl-2 regulatory network, where the system exhibits switch-like characteristics between survival and apoptosis states [21].
Bistability and Switch-like Behavior
The Bcl-2 family network demonstrates bistable behavior, characterized by hysteresis in its stimulus-response relationship [15] [21]. This bistability enables the all-or-none decision for MOMP that is critical for irreversible commitment to apoptosis. Computational analyses reveal that this emergent property requires specific organization of Bcl-2 family interactions and is most robust under the unified model of regulation [21].
Table 2: Mathematical Model Parameters for Bcl-2 Mediated Bistable Switch
| Parameter | Description | Value Range | Impact on Bistability |
|---|---|---|---|
| k₁ | Bax activation rate by tBid | 0.01-0.1 min⁻¹ | Determines switch sensitivity |
| k₂ | Bcl-2 inhibition rate of Bax | 0.05-0.2 nM⁻¹min⁻¹ | Affects bistability width |
| Kₐ | Affinity of BH3 proteins for Bcl-2 | 1-10 nM | Influences activation threshold |
| S | Synthesis rate of sensitizers | 0.001-0.01 nM/min | Modulates resistance to activation |
| θ | Threshold for MOMP commitment | 10-20% Bax activation | Defines point of no return |
Experimental Analysis of Bcl-2 Family Function
Methodologies for Investigating Protein Interactions
Co-immunoprecipitation and Western Blotting
Protocol for Protein Interaction Analysis:
- Cell Lysis: Harvest cells and lyse using NP-40 or CHAPS-containing buffer with protease inhibitors
- Immunoprecipitation: Incubate lysates with antibodies against target Bcl-2 proteins (e.g., anti-Bcl-2, anti-Bcl-xL)
- Pull-down: Add protein A/G beads, incubate at 4°C for 2-4 hours with rotation
- Washing: Pellet beads and wash 3-5 times with lysis buffer
- Elution: Boil beads in Laemmli buffer to elute proteins
- Western Blotting: Separate proteins by SDS-PAGE, transfer to PVDF membrane, and probe with antibodies against interacting partners (e.g., Bax, Bak, Bim)
This methodology allows detection of endogenous complexes between antiapoptotic proteins and their proapoptotic binding partners, providing insights into the equilibrium between survival and death signals [19].
BH3 Profiling
BH3 profiling measures mitochondrial priming to assess how close cells are to the apoptotic threshold:
Experimental Workflow:
- Isolate Mitochondria: Prepare mitochondrial fractions from cells of interest
- BH3 Peptide Exposure: Treat with synthetic BH3 peptides representing different specificities (Bad-like, Noxa-like, etc.)
- Membrane Potential Measurement: Monitor ΔΨm using JC-1 or TMRE dyes
- Cytochrome c Release Assessment: Measure cytochrome c release by ELISA or western blot
- Data Analysis: Determine pattern of sensitivity to different BH3 peptides to infer dependence on specific antiapoptotic proteins [13] [17]
Functional Assays for MOMP Regulation
MOMP Commitment Assay
Procedure:
- Cell Treatment: Expose cells to apoptotic stimuli (e.g., UV irradiation, chemotherapeutics)
- Subcellular Fractionation: At timed intervals, isolate cytosolic and mitochondrial fractions
- Cytochrome c Detection: Monitor cytochrome c localization by western blotting
- Caspase Activation: Measure caspase-3/7 activity using fluorogenic substrates
- Membrane Integrity Assessment: Evaluate mitochondrial membrane potential using potentiometric dyes
This assay determines the threshold at which MOMP occurs and identifies factors that modulate this commitment point [14].
Genetic Manipulation Studies
BCL-xL Inhibition in Pancreatic Differentiation:
- Cell Culture: Differentiate human pluripotent stem cells toward pancreatic lineage
- Pharmacological Inhibition: Treat with WEHI-539 (BCL-xL-specific inhibitor) at differentiation day 7
- Viability Assessment: Measure apoptosis by Annexin V/PI staining and caspase-3 cleavage
- Gene Expression Analysis: Perform RNA-seq and qPCR for pancreatic markers (PDX1, NKX6.1, etc.)
- Functional Rescue: Attempt rescue with caspase inhibitor QVD-OPh
This protocol demonstrated BCL-xL's critical role in survival of differentiating pancreatic progenitors, where inhibition caused increased apoptosis and decreased expression of pancreatic markers despite compensatory BCL-2 upregulation [19].
Research Reagent Solutions
Table 3: Essential Research Tools for Bcl-2 Family Investigation
| Reagent/Category | Specific Examples | Research Application | Key Features |
|---|---|---|---|
| BH3 Mimetics | Venetoclax (ABT-199), Navitoclax (ABT-263), WEHI-539 | Inhibit specific antiapoptotic proteins; investigate dependencies | Varying specificity profiles (BCL-2 only vs. BCL-2/BCL-xL) |
| Cell Line Models | BV-173 (CLL), MOLM-13 (AML), HCT-116 (colorectal) | Study cell-type-specific regulation; screen therapeutic responses | Different inherent expression patterns of Bcl-2 members |
| Antibodies | Anti-Bcl-2 (clone 100), Anti-Bcl-xL (clone 54H6), Anti-Bax (clone 6A7) | Detect protein expression; assess conformational changes | Conformation-specific antibodies available for activated Bax |
| Apoptosis Detection Kits Annexin V/PI, Caspase-Glo 3/7, JC-1 Mitochondrial Membrane Potential Assay | Quantify apoptotic commitment; measure mitochondrial integrity | Multiparameter flow cytometry compatible | |
| BH3 Peptides | Bad BH3, Noxa BH3, Bim BH3, HRK BH3 | BH3 profiling; determine antiapoptotic dependencies | Synthetic peptides with defined specificities |
Visualization of Bcl-2 Family Network
Therapeutic Implications and Research Frontiers
The delineation of Bcl-2 family interactions has enabled the development of BH3-mimetic drugs that selectively target antiapoptotic proteins [16] [17]. Venetoclax, a highly specific Bcl-2 inhibitor, has demonstrated remarkable efficacy in chronic lymphocytic leukemia and acute myeloid leukemia, validating the therapeutic potential of modulating this apoptotic switch [16]. However, resistance mechanisms, including upregulation of other antiapoptotic family members like Mcl-1 and Bcl-xL, present significant clinical challenges that necessitate combination therapies [19] [17].
Current research focuses on understanding cell-type-specific regulation of the Bcl-2 network, developing next-generation inhibitors with improved specificity profiles, and identifying predictive biomarkers for treatment response [17]. The integration of quantitative mathematical models with experimental data continues to refine our understanding of this critical apoptotic switch and its therapeutic exploitation [15] [21].
The B-cell lymphoma 2 (BCL2) protein family represents a critical class of regulators that determine cellular fate by controlling mitochondrial outer membrane permeabilization (MOMP), the pivotal step in intrinsic apoptosis [13] [22]. Since its initial discovery as the gene involved in the t(14;18) chromosomal translocation of follicular lymphoma, BCL2 was recognized as the first oncogene that promotes cell survival by blocking programmed cell death rather than accelerating proliferation [22] [20]. The BCL2 family comprises approximately 20 proteins in humans, which are categorized structurally and functionally into three principal groups: (1) multi-domain anti-apoptotic proteins (BCL2, BCL-XL, MCL1, BCL-w, BCL2A1, BCL-B); (2) multi-domain pro-apoptotic effector proteins (BAX, BAK, BOK); and (3) BH3-only pro-apoptotic proteins (BID, BIM, BAD, NOXA, PUMA, among others) [22]. These proteins share defining BCL2 homology (BH) domains and engage in a complex interplay that regulates cell survival decisions.
While the canonical function of this protein family in apoptosis regulation is well-established, contemporary research has revealed compelling non-canonical functions that extend beyond cell death control. Anti-apoptotic proteins, particularly BCL2 and BCL-XL, exhibit significant influence over cellular metabolism, redox homeostasis, and intracellular calcium (Ca²⁺) signaling [23] [24] [20]. These non-apoptotic activities contribute to their profound impact on cellular physiology and pathophysiological processes, including tumor development and chemoresistance. This review comprehensively examines both canonical and non-canonical functions of BCL2 and BCL-XL, framed within the context of their established role in inhibiting apoptosis, and explores the experimental approaches and therapeutic implications of these multifaceted biological activities.
Canonical Apoptotic Functions: Molecular Mechanisms and Models
The Central Paradigm: Regulating Mitochondrial Outer Membrane Permeabilization
The canonical function of BCL2 family proteins centers on their regulation of MOMP, which commits the cell to intrinsic apoptosis through cytochrome c release and subsequent caspase activation [13] [22]. Anti-apoptotic proteins, including BCL2 and BCL-XL, preserve mitochondrial integrity by directly binding and sequestering pro-apoptotic family members. They contain four BH domains (BH1-BH4) that form a characteristic hydrophobic surface groove, which serves as the primary interaction site for the BH3 domains of pro-apoptotic proteins [22]. The multi-domain pro-apoptotic effectors BAX and BAK, when activated, undergo conformational changes, oligomerize, and permeabilize the mitochondrial outer membrane, facilitating the release of cytochrome c and other intermembrane space proteins [13] [20]. The BH3-only proteins function as sentinels that sense cellular damage or stress signals and initiate the apoptotic cascade either by directly activating BAX/BAK or by neutralizing anti-apoptotic proteins [13].
Evolving Models of BCL2 Family Interactions
Several mechanistic models have been proposed to explain the complex interactions within the BCL2 protein family and their regulation of MOMP. These models reflect evolving understanding of the dynamic equilibrium governing cell survival decisions.
Table 1: Key Models of BCL2 Family Protein Interactions
| Model Name | Core Principle | Role of BH3-only Proteins | Role of Anti-apoptotic Proteins |
|---|---|---|---|
| Direct Activation | Activator BH3 proteins (BIM, tBID, PUMA) directly bind and activate BAX/BAK [13]. | Classified as "activators" or "sensitizers"; activators directly engage BAX/BAK [13]. | Sequester both activator and sensitizer BH3 proteins to prevent BAX/BAK activation [13]. |
| Displacement | BAX and BAK are constitutively active but inhibited by anti-apoptotic proteins; BH3 proteins displace them to induce apoptosis [13]. | Displace BAX/BAK from anti-apoptotic proteins by binding to the hydrophobic groove [13]. | Directly bind and inhibit active BAX and BAK; overexpression enhances survival [13]. |
| Embedded Together | Membrane environment dictates protein conformations and interactions; reversible conformational changes occur upon membrane binding [13]. | Activator BH3 proteins promote membrane insertion of BAX/BAK; all interactions governed by competing equilibria [13]. | Dual function: sequester activator BH3 proteins and active conformers of BAX/BAK at membranes [13]. |
| Unified | Anti-apoptotic proteins inhibit apoptosis through two distinct modes: sequestering activators (mode 1) and sequestering active BAX/BAK (mode 2) [13]. | Overcome mode 1 inhibition more easily than mode 2 inhibition [13]. | Both modes occur simultaneously; mode 2 inhibition is more efficient and also affects mitochondrial dynamics [13]. |
The "embedded together" and "unified" models incorporate the significance of cellular membranes as the primary locus for these protein interactions, where membrane integration induces conformational changes that modulate binding affinities and functional outcomes [13]. These refined models acknowledge that the relative concentrations, binding affinities, subcellular localizations, and post-translational modifications of BCL2 family members collectively determine cellular susceptibility to apoptosis.
Figure 1: Canonical BCL2 Family Regulation of Mitochondrial Apoptosis. Cellular stress activates BH3-only proteins which either directly activate pro-apoptotic effectors (BAX/BAK) or neutralize anti-apoptotic proteins. Anti-apoptotic proteins (BCL2, BCL-XL) maintain survival by sequestering both activators and effectors. BAX/BAK activation triggers MOMP, caspase activation, and apoptosis.
Non-Canonical Functions: Metabolic Regulation and Redox Control
Modulation of Mitochondrial Metabolism and Energetics
Beyond their established role in apoptosis regulation, BCL2 and BCL-XL exert significant influence over cellular metabolism. Research has demonstrated that BCL2 overexpression enhances mitochondrial oxygen consumption and respiratory capacity, indicating a direct impact on mitochondrial bioenergetics [23]. This increased electron transport chain activity generates a slightly pro-oxidant intracellular milieu characterized by elevated reactive oxygen species (ROS), which can promote genomic instability and modulate signaling pathways that support cell survival and transformation [23]. Paradoxically, under conditions of severe oxidative stress, BCL2 appears to regulate cellular redox homeostasis and prevent excessive ROS accumulation that would otherwise trigger cell death [23]. This dual capacity to modulate oxidative metabolism highlights the context-dependent functions of BCL2 in cellular adaptation to metabolic stress.
The molecular mechanisms through which BCL2 family proteins influence mitochondrial metabolism remain an active area of investigation. Potential mechanisms include direct interactions with mitochondrial membrane proteins involved in oxidative phosphorylation, modulation of mitochondrial membrane potential, or regulation of mitochondrial dynamics through interactions with fission and fusion machinery [20]. The "unified model" of BCL2 family function explicitly links the regulation of MOMP with mitochondrial dynamics, suggesting that anti-apoptotic proteins may coordinate both cell death execution and organelle homeostasis through overlapping mechanisms [13].
Experimental Approaches for Studying Metabolic Regulation
Investigation of BCL2-mediated metabolic regulation employs a combination of biochemical, cellular, and molecular techniques designed to quantify mitochondrial function and redox status.
Table 2: Key Methodologies for Studying BCL2 Family Protein Functions
| Experimental Approach | Application | Key Technical Details | Relevant Findings |
|---|---|---|---|
| Oxygen Consumption Measurement | Assess mitochondrial respiratory function [23]. | Use of Seahorse Analyzer or Clark-type electrode; measure in isolated mitochondria or intact cells with electron transport chain inhibitors. | BCL2 overexpression increases mitochondrial oxygen consumption [23]. |
| ROS Detection | Quantify reactive oxygen species production [23]. | Fluorescent probes (DCFDA, MitoSOX); flow cytometry or fluorescence microscopy; antioxidant controls essential. | BCL2 creates pro-oxidant milieu but prevents excessive ROS buildup during stress [23]. |
| Ca²⁺ Imaging | Measure cytosolic and organellar Ca²⁺ dynamics [24]. | Fluorescent indicators (Fura-2, Fluo-4); confocal microscopy; ER Ca²⁺ load assessment with ionomycin. | BCL2 inhibits IP3R-mediated Ca²⁺ release; BCL-XL may have context-dependent effects [24]. |
| Co-immunoprecipitation | Detect protein-protein interactions at ER-mitochondria interface [24]. | Crosslinking may be necessary; specific antibodies for BCL2 family proteins and IP3R; perform under native conditions. | BCL2 and BCL-XL directly interact with and modulate IP3 receptor function [24]. |
| BH3 Profiling | Assess functional interactions and dependencies [13] [22]. | Permeabilized cells exposed to synthetic BH3 peptides; measure cytochrome c release or membrane potential changes. | Identifies "primed" dependence on specific anti-apoptotic proteins for targeted therapy [22]. |
Figure 2: BCL2 Regulation of Mitochondrial Metabolism and Redox Homeostasis. BCL2/BCL-XL overexpression enhances mitochondrial oxygen consumption, generating controlled ROS that promotes genomic instability and pro-survival signaling. Under oxidative stress, these proteins maintain redox homeostasis to prevent excessive ROS-mediated death.
Non-Canonical Functions: Calcium Signaling Regulation
Endoplasmic Reticulum-Mitochondria Calcium Crosstalk
BCL2 family proteins localize not only to mitochondria but also to the endoplasmic reticulum (ER), where they participate in the regulation of intracellular Ca²⁺ homeostasis [24] [22]. The ER serves as the major intracellular Ca²⁺ storage organelle, and regulated Ca²⁺ release from the ER modulates diverse cellular processes including energy metabolism, proliferation, and apoptosis. ER-mitochondria contact sites facilitate efficient Ca²⁺ transfer between these organelles, with excessive mitochondrial Ca²⁺ uptake promoting MOMP and cell death [24]. Anti-apoptotic BCL2 family proteins, particularly BCL2 and BCL-XL, modulate Ca²⁺ signaling primarily through direct interactions with inositol 1,4,5-trisphosphate receptors (IP3Rs), the major Ca²⁺ release channels in the ER membrane [24].
BCL2 directly binds to IP3Rs and suppresses pro-apoptotic Ca²⁺ signaling, thereby maintaining Ca²⁺ within a range compatible with cell survival [24]. The functional consequences of BCL-XL modulation of IP3Rs appear more complex and potentially context-dependent. While some studies indicate that BCL-XL sensitizes IP3R function to promote pro-survival oscillatory Ca²⁺ release, other evidence suggests that, similar to BCL2, BCL-XL can also inhibit IP3Rs under specific conditions [24]. This apparent discrepancy may reflect cell type-specific differences, varying expression levels of BCL2 family proteins and their binding partners, or the influence of post-translational modifications on these protein complexes.
Methodologies for Calcium Signaling Research
The investigation of BCL2 family protein regulation of Ca²⁺ signaling requires specialized techniques to quantify and manipulate intracellular Ca²⁺ dynamics, particularly at organellar interfaces.
Table 3: Research Reagent Solutions for BCL2 Family Protein Studies
| Reagent/Category | Specific Examples | Function/Application | Experimental Utility |
|---|---|---|---|
| BH3 Mimetics | ABT-737, ABT-263 (navitoclax), ABT-199 (venetoclax) [22]. | Small molecules that occupy hydrophobic groove of anti-apoptotic BCL2 proteins. | Displace pro-apoptotic proteins to induce apoptosis; study specific anti-apoptotic protein dependencies [22]. |
| Ca²⁺ Indicators | Fura-2 (rationetric), Fluo-4 (intensity-based), organelle-targeted probes [24]. | Fluorescent dyes that bind Ca²⁺ with changing spectral properties. | Quantify cytosolic and organellar Ca²⁺ concentrations; measure dynamics in live cells [24]. |
| IP3R Modulators | Adenophostin (activator), Xestospongin (inhibitor), IP3R isoform-specific antibodies [24]. | Pharmacological and molecular tools to manipulate IP3R activity. | Probe BCL2-IP3R interactions; establish causal relationship between IP3R function and cell survival [24]. |
| Protein Interaction Tools | Co-immunoprecipitation kits, crosslinkers, recombinant BH3 peptides [24] [13]. | Reagents to detect and quantify protein-protein interactions. | Map BCL2 family interactions with IP3Rs and other partners; determine binding affinities [24]. |
| Genetic Models | siRNA/shRNA, CRISPR/Cas9, overexpression constructs, transgenic mice. | Modulate expression of specific BCL2 family members. | Establish necessity and sufficiency of specific proteins in Ca²⁺ signaling and metabolism [24]. |
Figure 3: BCL2 Family Regulation of ER-Mitochondria Ca²⁺ Crosstalk. BCL2/BCL-XL modulate IP3 receptor function on the ER membrane, controlling Ca²⁺ release and transfer to mitochondria. This regulation maintains pro-survival oscillatory signaling while preventing sustained pro-apoptotic Ca²⁺ transfer that would trigger MOMP.
Therapeutic Targeting and Clinical Translation
BH3-Mimetics: From Basic Research to Clinical Application
The mechanistic understanding of BCL2 family interactions has enabled the rational design of therapeutic compounds known as BH3-mimetics, which occupy the hydrophobic groove of anti-apoptotic proteins and functionally neutralize them [22]. ABT-737, developed in 2005 through NMR-based screening and structure-based design, represented the first specific and potent BH3-mimetic, exhibiting high-affinity binding to BCL-XL, BCL2, and BCL-w [22]. The oral analogue navitoclax (ABT-263) entered clinical trials but demonstrated dose-limiting thrombocytopenia due to BCL-XL inhibition in platelets [22]. This toxicity prompted the development of venetoclax (ABT-199), the first BCL2-selective inhibitor, which received FDA and EMA approval in 2016 and has transformed treatment for several hematologic malignancies, particularly chronic lymphocytic leukemia (CLL) [22].
Following the clinical success of venetoclax, several chemically similar BCL2 inhibitors including sonrotoclax and lisaftoclax are undergoing clinical evaluation, both as monotherapies and in rational combinations [22]. However, targeting other anti-apoptotic family members, particularly BCL-XL and MCL1, has proven more challenging. BCL-XL inhibition induces profound thrombocytopenia, while MCL1 inhibition has been associated with cardiac toxicities, complications that have limited the clinical development of conventional inhibitors for these targets [22]. Novel approaches including proteolysis targeting chimeras (PROTACs), antibody-drug conjugates (ADCs), and compounds targeting the BH4 domain of BCL2 offer promising strategies to achieve tumor-specific inhibition with improved therapeutic indices [22].
Experimental Workflow for Therapeutic Development
The development and evaluation of BCL2-targeting therapies follows a structured translational pipeline that integrates multiple experimental approaches.
Figure 4: Therapeutic Development Pipeline for BCL2-Targeting Agents. The workflow begins with identifying BCL2 family dependencies in specific cancers, followed by compound screening using structural biology approaches, mechanistic validation, preclinical testing in relevant models, and finally clinical evaluation.
The BCL2 protein family embodies a sophisticated regulatory network that governs cellular fate through both canonical control of mitochondrial apoptosis and non-canonical regulation of metabolism and Ca²⁺ signaling. The dual functions of BCL2 and BCL-XL in inhibiting MOMP while simultaneously modulating oxidative metabolism and ER-mitochondrial Ca²⁺ transfer highlight their central role in maintaining cellular homeostasis. These multifaceted activities contribute to their profound impact on development, tissue homeostasis, and disease pathogenesis, particularly in cancer. The successful clinical translation of BH3-mimetics, exemplified by venetoclax, validates the therapeutic potential of targeting these pathways and underscores the importance of fundamental mechanistic research in driving innovative cancer therapeutics. Future research directions will likely focus on understanding the contextual determinants of BCL2 family function, developing novel targeting strategies with improved specificity, and identifying rational combination approaches to overcome resistance mechanisms. The continued dissection of both canonical and non-canonical BCL2 family functions promises to yield further insights into cellular homeostasis and new opportunities for therapeutic intervention in cancer and other diseases characterized by aberrant cell survival.
From Bench to Bedside: Developing BH3-Mimetics and Clinical Applications
The B-cell lymphoma 2 (BCL-2) family of proteins represents a critical regulatory node in the intrinsic pathway of apoptosis, with anti-apoptotic members such as BCL-2 and BCL-xL serving as fundamental barriers to programmed cell death. Their overexpression is a hallmark of numerous cancers, conferring both tumorigenic potential and resistance to conventional therapies. This technical guide explores the rational design of BH3-mimetics, a class of targeted therapeutics that strategically disrupt the protein-protein interactions between pro-apoptotic and anti-apoptotic BCL-2 family members. By examining their structural basis, mechanism of action, and quantitative performance across experimental models, this review provides researchers and drug development professionals with a comprehensive framework for understanding and advancing this promising therapeutic paradigm.
The BCL-2 protein family constitutes the essential regulatory circuit governing mitochondrial apoptosis, determining cellular life-or-death decisions in response to developmental cues and stress signals [2] [7]. The founding member, BCL-2, was first identified in 1984 at the breakpoint of the t(14;18) chromosomal translocation in follicular lymphoma, representing one of the first oncogenes recognized to promote cancer by inhibiting cell death rather than enhancing proliferation [2] [25]. The family is categorized by structural and functional characteristics into three principal subgroups:
- Multi-domain anti-apoptotic proteins (BCL-2, BCL-xL, MCL-1, BCL-W, BFL-1, BCL-B) containing four BCL-2 homology (BH) domains
- Multi-domain pro-apoptotic effector proteins (BAX, BAK, BOK) responsible for mitochondrial outer membrane permeabilization (MOMP)
- BH3-only proteins (BIM, BID, BAD, PUMA, NOXA, etc.) that function as sensitizers and activators of apoptosis [2] [7]
Anti-apoptotic proteins such as BCL-2 and BCL-xL maintain mitochondrial integrity by sequestering pro-apoptotic family members, thereby preventing MOMP and the subsequent release of cytochrome c that activates the caspase cascade [2]. In many malignancies, the delicate balance between these opposing factions is disrupted, with overexpression of BCL-2 and BCL-xL enabling cancer cells to evade apoptosis and resist cytotoxic therapies [26] [7]. This pathophysiological mechanism established BCL-2 and BCL-xL as compelling targets for rational drug design, culminating in the development of BH3-mimetics.
Structural Foundation for BH3-Mimetic Design
The Hydrophobic Groove and BH3 Domain Interface
The structural basis for BH3-mimetic design emerged from elucidating the three-dimensional architecture of anti-apoptotic BCL-2 family proteins. BCL-xL, the first family member whose structure was solved, revealed a globular α-helical bundle featuring a prominent hydrophobic groove on its surface [7]. This groove, formed by the close apposition of BH1, BH2, and BH3 domains, serves as the critical docking site for the amphipathic α-helical BH3 domains of pro-apoptotic partners [2] [27].
The interaction is mediated by four hydrophobic pockets (designated P1-P4) within the binding groove that accommodate specific residues from the BH3 helix [2]. The BH3 domain itself comprises approximately 15-20 amino acids that form an amphipathic α-helix, with conserved hydrophobic residues positioned to engage the groove while charged residues contribute to binding specificity [28]. This precise molecular recognition mechanism enables anti-apoptotic proteins to selectively sequester pro-apoptotic partners through high-affinity protein-protein interactions.
BCL-2 and BCL-xL Structural Variations
While BCL-2 and BCL-xL share significant structural homology (44% sequence identity), key differences in their hydrophobic grooves influence ligand specificity [25] [7]. These variations arise from amino acid substitutions that alter the topography and chemical properties of the binding cleft, necessitating tailored design approaches for selective inhibitors. BCL-xL additionally undergoes complex splicing regulation, generating both anti-apoptotic (BCL-xL) and pro-apoptotic (BCL-xS) isoforms from the same gene through alternative splicing [25]. The BCL-xS isoform lacks BH1 and BH2 domains, rendering it incapable of maintaining the canonical hydrophobic groove and instead conferring pro-apoptotic function through interaction with voltage-dependent anion channel (VDAC) [25].
Diagram 1: BCL-2 Family Regulation of Mitochondrial Apoptosis. Cellular stress activates BH3-only proteins that either neutralize anti-apoptotic members or directly activate effector proteins (BAX/BAK), leading to mitochondrial outer membrane permeabilization (MOMP) and apoptosis.
BH3-Mimetic Design Strategies
Rational Drug Design Approaches
BH3-mimetics are designed using structure-based strategies to replicate the critical binding interactions of native BH3 domains within the hydrophobic groove of anti-apoptotic targets. The primary design approaches include:
Small molecule inhibitors developed through NMR-based screening, parallel synthesis, and structure-based design. ABT-737 exemplifies this approach, generated by linking proximally binding fragments to achieve high-affinity engagement of the hydrophobic groove [2]. Modified versions with improved oral bioavailability led to navitoclax (ABT-263) and the BCL-2-selective venetoclax (ABT-199) [2] [28].
Stabilized α-helical peptides employing hydrocarbon stapling to reinforce the native helical structure of BH3 domains. This technique, applied to peptides derived from BID and other BH3-only proteins, enhances proteolytic resistance and cell permeability while maintaining high binding affinity [27].
Pharmacophore-based screening utilizing molecular dynamics studies of BCL-xL/BH3 complexes to derive interaction pharmacophores, which serve as queries for 3D database screening of compound libraries [29].
Specificity Engineering
A central challenge in BH3-mimetic design lies in achieving selectivity among highly homologous anti-apoptotic family members. Early compounds like ABT-737 and navitoclax target BCL-2, BCL-xL, and BCL-w with nanomolar affinity but spare MCL-1 and BCL-2A1 due to structural differences in their hydrophobic grooves [2] [26]. Venetoclax represents a refined specificity achievement, with selective BCL-2 inhibition achieved through strategic modifications that reduce BCL-xL affinity, thereby circumventing the thrombocytopenia associated with BCL-xL inhibition [2] [26].
Table 1: Evolution of BH3-Mimetic Specificity Profiles
| Compound | Primary Targets | Affinity (nM) | Specificity Achievements | Clinical Status |
|---|---|---|---|---|
| ABT-737 | BCL-2, BCL-xL, BCL-w | <1 | Spares MCL-1 | Preclinical tool compound |
| Navitoclax (ABT-263) | BCL-2, BCL-xL, BCL-w | <1 | Oral bioavailability | Clinical trials, limited by thrombocytopenia |
| Venetoclax (ABT-199) | BCL-2 | <1 | >100-fold selectivity over BCL-xL | FDA-approved for hematologic malignancies |
| WEHI-539 | BCL-xL | ~1 | Selective BCL-xL inhibition | Preclinical tool compound |
| S1 | BCL-2, MCL-1 | Not specified | Dual BCL-2/MCL-1 targeting | Preclinical development |
Quantitative Analysis of BH3-Mimetic Efficacy
The efficacy of BH3-mimetics has been quantitatively evaluated across numerous cancer models, with particular success demonstrated in hematological malignancies. The following table summarizes key efficacy data for prominent BH3-mimetics:
Table 2: Quantitative Efficacy Profiles of Selected BH3-Mimetics
| BH3-Mimetic | Cancer Models with Demonstrated Efficacy | IC₅₀ for Target Disruption | In Vivo Efficacy (Model) | Key Limitations |
|---|---|---|---|---|
| ABT-737 | SCLC cell lines, CLL, AML | <100 nM | Tumor regression (lymphoma xenografts) | No oral bioavailability |
| Navitoclax | CLL, SCLC, ALL | 1-10 nM | 60% tumor growth inhibition (SCLC xenografts) | Dose-dependent thrombocytopenia |
| Venetoclax | CLL, AML, NHL | <10 nM | 90% tumor growth inhibition (CLL xenografts) | Limited single-agent activity in solid tumors |
| Obatoclax (GX15-070) | Various solid and hematologic tumors | 1-7 μM (non-selective) | Modest single-agent activity | Neurological toxicity, limited efficacy |
| Sabutoclax (BI97C1) | Prostate cancer, lymphoma | ~0.3-3 μM | Synergistic with bortezomib (prostate cancer) | Moderate potency |
| S1 | Liver carcinoma, SCLC | Not specified | Tumor suppression (hepatoma xenografts) | ER stress induction, resistance mechanisms |
The quantitative data reveal several critical patterns. First, potency varies substantially among BH3-mimetics, with the ABT series demonstrating nanomolar efficacy compared to micromolar ranges for earlier compounds like obatoclax. Second, hematologic malignancies show superior responsiveness, with many solid tumors exhibiting inherent resistance. Third, target specificity directly influences therapeutic index, as evidenced by venetoclax overcoming the thrombocytopenia associated with BCL-xL inhibition.
Experimental Protocols and Methodologies
BH3 Profiling for Target Validation
BH3 profiling serves as a fundamental experimental protocol for assessing mitochondrial priming and predicting sensitivity to BH3-mimetics. The methodology involves:
- Isolation of mitochondria from target cells or tissues via differential centrifugation.
- Exposure to synthetic BH3 peptides representing different BH3-only proteins (BIM, BAD, NOXA, etc.) to measure MOMP-dependent dye release.
- Quantification of cytochrome c release or mitochondrial membrane depolarization as apoptosis indicators.
- Pattern analysis of response profiles to determine dependence on specific anti-apoptotic proteins.
This technique enables researchers to identify "primed" cells with high apoptotic readiness that likely will respond to BH3-mimetics, and to determine which anti-apoptotic proteins represent the dominant survival dependencies [28].
Co-immunoprecipitation Assays for Target Engagement
Direct assessment of BH3-mimetic-mediated disruption of protein-protein interactions employs co-immunoprecipitation:
- Cell lysis under non-denaturing conditions to preserve native protein complexes.
- Incubation with BH3-mimetic at varying concentrations and timepoints.
- Immunoprecipitation of target anti-apoptotic protein (e.g., BCL-2 or BCL-xL).
- Western blot analysis of co-precipitating pro-apoptotic partners (e.g., BIM, BAX).
- Quantification of disruption by densitometry, with IC₅₀ values calculated from concentration-response curves.
This protocol provides direct evidence of target engagement and functional disruption of anti-apoptotic complexes [9].
Xenograft Models for In Vivo Evaluation
The therapeutic efficacy of BH3-mimetics is typically evaluated in human tumor xenograft models:
- Implantation of human cancer cells or patient-derived xenografts into immunocompromised mice.
- Randomization and dosing once tumors reach measurable size (typically 100-200 mm³).
- Administration of BH3-mimetic via appropriate route (oral gavage for bioavailable compounds, injection for others).
- Tumor volume measurement 2-3 times weekly by caliper.
- Biomarker analysis including cleaved caspase-3 for apoptosis induction and Ki-67 for proliferation index.
- Tolerability assessment via body weight monitoring, hematological parameters, and histological examination of key organs.
This comprehensive protocol establishes both anti-tumor efficacy and therapeutic index [30].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for BH3-Mimetic Investigations
| Reagent/Category | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| Tool Compound Inhibitors | ABT-737, WEHI-539, ABT-199 | Mechanistic studies, target validation | Use at 10 nM-10 μM range; confirm on-target effects with rescue experiments |
| Stapled Peptides | Hydrocarbon-stapled BIM, BID peptides | Protein-protein interaction disruption | Enhanced cellular uptake compared to native peptides; check stability in serum |
| Antibodies for Detection | Anti-BCL-2, Anti-BCL-xL, Anti-BIM, Anti-cleaved caspase-3 | Western blot, IHC, immunofluorescence | Validate specificity with knockout/knockdown controls |
| Cell Line Models | OCI-Ly1 (lymphoma), MOLT-4 (ALL), SCLC lines | In vitro efficacy screening | Screen for endogenous BCL-2 family expression profiles |
| Apoptosis Assays Annexin V/propidium iodide, JC-1, DEVD-ase activity | Quantification of cell death | Use multiple complementary assays for confirmation | |
| Protein Interaction Assays | Co-IP kits, FRET-based systems, SPR | Target engagement assessment | Include relevant controls for non-specific interactions |
| Polymeric Delivery Systems | pH-responsive Pol950, Pol300 micelles | Enhanced intracellular delivery | Particularly useful for peptide-based mimetics [30] |
Future Directions and Emerging Technologies
The field of BH3-mimetic development continues to evolve with several promising strategic advances:
PROTACs (Proteolysis Targeting Chimeras) leverage bifunctional molecules that recruit E3 ubiquitin ligases to target proteins, inducing their degradation rather than mere inhibition. This approach offers potential advantages in overcoming resistance mutations and achieving more durable responses [2].
Antibody-drug conjugates (ADCs) represent an alternative delivery strategy, employing tumor-specific antibodies to deliver BH3-mimetic payloads directly to malignant cells. For example, anti-CD22 antibodies conjugated to BIM peptides have demonstrated efficacy in B-cell lymphoma models with reduced systemic exposure [30].
Dual-specificity inhibitors targeting combinations such as BCL-xL/MCL-1 (e.g., JY-1-106) address the resistance mechanisms that often emerge through compensatory upregulation of alternative anti-apoptotic proteins [26].
Nanocarrier systems incorporating pH-responsive polymeric micelles enhance the cytosolic delivery of peptide-based BH3-mimetics, improving tumor biodistribution and pharmacokinetic profiles [30] [28].
Diagram 2: BH3-Mimetic Design Strategies and Their Characteristics. Multiple design approaches have been developed to target the BCL-2 family protein-protein interface, each with distinct advantages.
The rational design of BH3-mimetics represents a paradigm shift in targeted cancer therapy, demonstrating the feasibility of disrupting challenging protein-protein interactions with small molecules and engineered peptides. The trajectory from basic structural insights to clinically effective therapeutics like venetoclax validates the BCL-2 family as a compelling therapeutic target, particularly in hematologic malignancies. Ongoing challenges include expanding efficacy to solid tumors, overcoming resistance mechanisms, and improving therapeutic indices through enhanced specificity and innovative delivery systems. As understanding of BCL-2 family biology deepens and drug discovery technologies advance, the next generation of BH3-mimetics promises to further refine this targeted approach to restoring apoptosis in cancer cells.
The B-cell lymphoma-2 (BCL-2) family of proteins serves as the central regulator of the intrinsic (mitochondrial) apoptotic pathway, a programmed cell death process essential for maintaining tissue homeostasis and eliminating damaged cells [12] [31]. This protein family is structurally characterized by BCL-2 homology (BH) domains and functionally divided into three groups: (1) anti-apoptotic proteins (including BCL-2, BCL-XL, MCL-1, BCL-W, and BFL-1) that contain four BH domains and promote cell survival; (2) pro-apoptotic effector proteins (BAX, BAK, and BOK) containing three BH domains; and (3) BH3-only proteins (BIM, BID, BAD, NOXA, PUMA) that initiate apoptosis signaling [16] [32]. The critical balance between these opposing factions determines cellular fate—survival or death.
Anti-apoptotic proteins like Bcl-2 and Bcl-xL are frequently overexpressed in cancer cells, enabling them to evade programmed cell death and resist conventional therapies [12] [31]. They function by sequestering pro-apoptotic proteins, thereby preventing mitochondrial outer membrane permeabilization (MOMP), a pivotal event in apoptosis initiation [33]. During MOMP, permeabilization leads to the release of cytochrome c and other pro-apoptotic factors into the cytoplasm, triggering caspase activation and irreversible cellular destruction [33] [16]. The therapeutic targeting of these anti-apoptotic proteins represents a promising strategy for overcoming apoptosis evasion in cancer treatment, driving the development of specific inhibitors known as BH3 mimetics [31].
First-Generation Inhibitors: The Navitoclax Era
Development and Mechanism of Action
The journey to targeted BCL-2 family inhibition began with ABT-737, a small-molecule inhibitor developed using nuclear magnetic resonance (NMR)-based chemical screening and structure-based design [32] [31]. ABT-737 exhibited high-affinity binding to BCL-2, BCL-XL, and BCL-W, demonstrating potent anti-tumor activity in preclinical models of lymphoma and small cell lung cancer [32]. However, its clinical application was limited by poor solubility and oral bioavailability, prompting the development of navitoclax (ABT-263), an orally bioavailable analog [32] [31].
Navitoclax functions as a BH3 mimetic, designed to bind the hydrophobic grooves of anti-apoptotic BCL-2 family proteins with high affinity [34] [35]. By occupying these binding sites, navitoclax displaces pro-apoptotic proteins like BIM and BAX, disrupting their sequestration and enabling them to initiate MOMP and subsequent caspase activation [32] [35]. This mechanism effectively shifts the cellular balance toward apoptosis, particularly in cancer cells dependent on BCL-2 family proteins for survival.
Table 1: Profile of First-Generation BCL-2 Family Inhibitors
| Inhibitor | Targets | Administration | Key Preclinical Findings | Clinical Limitations |
|---|---|---|---|---|
| ABT-737 | BCL-2, BCL-XL, BCL-W | Intravenous | Activity against lymphoma, SCLC, myeloma, and leukemia cell lines; tumor regression in xenograft models | Poor solubility and oral bioavailability |
| Navitoclax (ABT-263) | BCL-2, BCL-XL, BCL-W | Oral | Tumor regression in SCLC and ALL xenograft models; enhanced efficacy in combination regimens for lymphoma and myeloma | Dose-limiting thrombocytopenia due to BCL-XL inhibition |
Clinical Limitations and the Thrombocytopenia Challenge
Despite demonstrating efficacy in early clinical trials for lymphoid malignancies, navitoclax faced a significant clinical obstacle: dose-dependent thrombocytopenia [32] [31]. This side effect emerged from the critical role of BCL-XL in platelet survival, as BCL-XL inhibits the apoptosis of these circulating cells [32] [31]. Navitoclax's inhibition of BCL-XL accelerated platelet apoptosis, leading to rapid reductions in circulating platelet counts [34] [31]. This thrombocytopenia proved dose-limiting, restricting the ability to achieve exposures necessary for optimal anti-tumor efficacy and highlighting the need for more selective inhibitors that could spare platelets [32] [31].
The Advent of Venetoclax: A Selective Bcl-2 Inhibitor
Rational Drug Design and Engineering
The clinical limitations of navitoclax spurred a targeted drug discovery initiative to develop a BCL-2-selective inhibitor that would avoid BCL-XL-mediated thrombocytopenia [31]. Through structure-based drug design informed by BCL-2-small molecule co-crystal structures, researchers at AbbVie engineered venetoclax (ABT-199/GDC-0199) [32] [31]. Key structural modifications were made to navitoclax's scaffold to alter electrostatic interactions with residue Arg103, which is specific to BCL-2 (BCL-XL possesses Glu96 at the comparable position), thereby achieving high selectivity for BCL-2 over BCL-XL [32].
Venetoclax emerged as a potent, oral BH3 mimetic with sub-nanomolar affinity for BCL-2 (K(_i) < 0.010 nM) while sparing BCL-XL [32]. This selectivity translated to a dramatically reduced effect on platelets in preclinical models, resolving the primary toxicity that hampered navitoclax's development [32] [31]. Preclinical studies demonstrated venetoclax's potent anti-leukemic activity against BCL-2-dependent cell lines and xenograft models, providing strong rationale for clinical advancement [31].
Molecular Mechanism of Action
Venetoclax precisely mimics the function of native BH3-only proteins by binding to the BH3-binding groove of BCL-2 [33] [16]. In cancer cells that overexpress BCL-2 and are "primed for death," this binding displaces pro-apoptotic proteins such as BIM and BAX that are sequestered by BCL-2 [33]. Once liberated, these activators directly trigger BAX and BAK oligomerization, leading to MOMP, cytochrome c release, and activation of the caspase cascade, ultimately inducing programmed cell death [33] [16]. This mechanism is particularly effective in hematologic malignancies where cancer cells exhibit heightened dependence on BCL-2 for survival.
Table 2: Key Preclinical and Early Clinical Findings for Venetoclax
| Study Aspect | Key Findings |
|---|---|
| Binding Affinity | Sub-nanomolar affinity for BCL-2 (K(_i) < 0.010 nM); >100-fold selectivity over BCL-XL |
| Platelet Effects | Significantly reduced platelet killing compared to navitoclax in ex vivo and in vivo models |
| Anti-Tumor Activity | Striking activity in BCL-2-dependent cell lines and xenograft models, particularly in CLL and AML |
| Clinical Translation | FDA and EMA approval for relapsed CLL with 17p deletion; activity in broader CLL population and other hematologic malignancies |
Experimental Approaches and Research Methodologies
Key Experimental Protocols
The development of BH3 mimetics relied on sophisticated experimental methodologies to evaluate compound efficacy, mechanism of action, and therapeutic potential:
BH3 Profiling: This technique assesses mitochondrial priming by exposing isolated mitochondria or permeabilized cells to synthetic BH3 peptides that mimic specific pro-apoptotic proteins [31]. The pattern of cytochrome c release in response to different BH3 peptides helps identify which anti-apoptotic proteins a particular cancer cell depends on for survival, predicting sensitivity to specific BH3 mimetics.
Co-crystallization and Structure-Based Design: X-ray crystallography of BCL-2 family proteins bound to small molecule inhibitors provided critical insights into binding interactions and specificity determinants [32] [31]. This structural information enabled rational drug design approaches to optimize binding affinity and selectivity through iterative chemical modifications.
In Vivo Efficacy Studies: Patient-derived xenograft (PDX) models and genetically engineered mouse models were utilized to evaluate the anti-tumor activity of BH3 mimetics in vivo [32] [31]. These studies typically involved administering compounds orally or intravenously to tumor-bearing mice and monitoring tumor volume, survival outcomes, and pharmacodynamic markers of apoptosis induction.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Studying BCL-2 Inhibition
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| BCL-2 Family Inhibitors | ABT-737, Navitoclax, Venetoclax, WEHI-539, A-1331852 | Tool compounds for dissecting dependencies; positive controls for experiments |
| Selective BCL-XL Inhibitors | WEHI-539, A-1331852 | Investigate BCL-XL-specific biology; counter-screens for BCL-2 selectivity |
| BH3 Peptides | BIM BH3, BAD BH3, NOXA BH3 MS-1 | BH3 profiling; measuring mitochondrial priming and dependencies |
| Antibodies for Detection | Anti-BCL-2, Anti-BCL-XL, Anti-BAX, Anti-BAK, Anti-BIM, Anti-cleaved Caspase-3 | Western blot, IHC, and flow cytometry to assess protein expression and apoptosis |
| Viability Assays | MTT, CellTiter-Glo, Annexin V/PI staining | Quantifying cell death and apoptosis in response to treatment |
Clinical Translation and Therapeutic Impact
Venetoclax has fundamentally altered the treatment landscape for several hematologic malignancies. It received FDA approval in 2016 for patients with relapsed or refractory chronic lymphocytic leukemia (CLL) with 17p deletion, representing the first approved targeted inhibitor of BCL-2 [32] [31]. Subsequent approvals expanded its use to other leukemia types, notably in combination with hypomethylating agents for acute myeloid leukemia (AML) [16] [36].
Clinical studies have demonstrated remarkable efficacy, with one trial reporting an 84% overall response rate in multiple myeloma patients treated with venetoclax [33]. In CLL, venetoclax treatment has been associated with higher 5-year survival rates compared to conventional chemotherapy [33]. The drug's oral administration and generally manageable safety profile, with reduced risk of thrombocytopenia compared to navitoclax, represent significant advances in patient care [33] [32].
Beyond single-agent activity, venetoclax has shown promising efficacy in combination regimens with other anti-cancer agents, including monoclonal antibodies, hypomethylating agents, and other targeted therapies [16] [36]. These combinations leverage synergistic mechanisms to overcome resistance and improve depth and duration of response.
Visualizing the Apoptotic Pathway and Drug Mechanism
Diagram 1: Mechanism of BCL-2 Inhibition and Apoptosis Induction. This diagram illustrates how survival signals promote cell survival through BCL-2/BCL-xL expression, and how BH3 mimetics like venetoclax disrupt this process by binding to BCL-2, displacing pro-apoptotic proteins, and triggering the mitochondrial pathway of apoptosis.
The evolution from navitoclax to venetoclax exemplifies how rational drug design can overcome clinical limitations by enhancing target selectivity, demonstrating the power of structure-based approaches in modern drug development [32] [31]. This journey has not only produced a transformative cancer therapeutic but has also deepened our understanding of apoptotic regulation and cancer dependencies.
Current research continues to optimize BCL-2 inhibition strategies, including the development of next-generation BH3 mimetics with distinct selectivity profiles, such as S55746 (BCL201), APG-2575 (lisaftoclax), and dual BCL-2/BCL-XL inhibitors like AZD0466 [16]. Investigation of predictive biomarkers—including BCL-2 expression levels, BH3 profiling patterns, and specific genetic mutations—aims to better identify patients most likely to respond to therapy [16] [36]. Additionally, novel combination approaches seek to overcome resistance mechanisms, particularly involving upregulation of alternative anti-apoptotic proteins like MCL-1 [16] [36].
The translational success of venetoclax validates the therapeutic targeting of the BCL-2 family in cancer and provides a roadmap for future development of apoptosis-based therapies, potentially extending to solid tumors and non-oncologic indications where apoptotic regulation plays a critical pathophysiological role.
The B-cell lymphoma-2 (BCL-2) family of proteins constitutes fundamental regulators of the intrinsic (mitochondrial) apoptotic pathway, serving as critical arbiters of cellular survival and death [37]. The delicate balance between pro-apoptotic and anti-apoptotic members of this family determines cellular fate in response to various stressors. Malignant cells, including those in chronic lymphocytic leukemia (CLL) and acute myeloid leukemia (AML), frequently overexpress anti-apoptotic proteins such as BCL-2 and BCL-xL, enabling them to evade programmed cell death and resist conventional therapies [38] [3]. This molecular understanding paved the way for developing targeted agents known as BH3 mimetics, which structurally resemble the BH3 domain of pro-apoptotic proteins and competitively disrupt the interaction between pro-survival and pro-apoptotic family members [37]. Venetoclax (ABT-199), a first-in-class, highly selective, orally bioavailable BCL-2 inhibitor, represents a paradigm shift in the treatment of hematological malignancies by directly targeting this apoptotic blockade [38] [3]. This whitepaper examines the transformative role of venetoclax in CLL and AML, detailing its mechanism of action, clinical efficacy, emerging resistance mechanisms, and essential research methodologies.
Molecular Mechanisms of BCL-2 Family Regulation
BCL-2 Family Proteins and Apoptotic Control
The BCL-2 protein family consists of both pro-survival and pro-apoptotic members that regulate mitochondrial outer membrane permeabilization (MOMP), the pivotal commitment point in intrinsic apoptosis [37] [39]. Anti-apoptotic proteins, including BCL-2, BCL-xL, MCL-1, BCL-W, and A1/BFL-1, share four BCL-2 homology (BH) domains (BH1-BH4) and possess a hydrophobic groove that binds the BH3 domain of pro-apoptotic partners [40] [37]. Pro-apoptotic effectors, such as BAX and BAK, contain multiple BH domains and directly execute MOMP, while another group of proteins (e.g., BIM, BID, PUMA, BAD, NOXA) possess only the BH3 domain and function as initiators or sensitizers [37] [39]. In healthy cells, anti-apoptotic proteins sequester these pro-apoptotic proteins, preventing MOMP. Cellular stress signals transcriptionally upregulate or post-translationally activate BH3-only proteins, which then bind to and neutralize anti-apoptotic proteins, freeing BAX and BAK to oligomerize and permeabilize the mitochondrial membrane, leading to cytochrome c release, caspase activation, and apoptotic cell death [37] [39].
Venetoclax as a BH3 Mimetic
Venetoclax was meticulously designed through reverse engineering to be a highly selective BH3 mimetic with strong affinity for BCL-2 but significantly reduced affinity for BCL-xL, a protein crucial for platelet survival [38] [3]. This selectivity differentiates it from earlier, less specific inhibitors like navitoclax (ABT-263), which targets both BCL-2 and BCL-xL and causes dose-limiting thrombocytopenia [3]. By occupying the hydrophobic groove of BCL-2, venetoclax displaces pro-apoptotic proteins like BIM and BAX, initiating a cascade that leads to mitochondrial outer membrane permeabilization and TP53-independent apoptosis [38]. This mechanism is particularly effective in malignancies characterized by BCL-2 overexpression, such as CLL, where BCL-2 is universally overexpressed, creating a state of "primed" readiness for apoptosis that venetoclax effectively exploits [38] [37].
Figure 1: Mechanism of Venetoclax as a BH3 Mimetic. In normal cells (top), anti-apoptotic proteins sequester pro-apoptotic effectors, preventing MOMP. Venetoclax (bottom) competitively binds BCL-2, displacing pro-apoptotic proteins and triggering apoptosis.
Venetoclax in Chronic Lymphocytic Leukemia (CLL)
Monotherapy Efficacy
CLL represents the ideal disease context for venetoclax therapy due to universal BCL-2 overexpression in CLL cells [38]. The initial dose-escalation study of venetoclax monotherapy in relapsed/refractory (R/R) CLL enrolled patients with poor prognostic features (89% with high-risk genetics) yet demonstrated remarkable efficacy at the 400 mg dose, with an overall response rate (ORR) of 79%, complete response (CR) rate of 20%, undetectable minimal residual disease (uMRD) rate of 15%, and 15-month progression-free survival (PFS) of 69% [38]. This study marked the first report of uMRD achievement in R/R CLL treated with novel agents. Subsequent data from 158 patients, predominantly (97%) with del(17p) R/R CLL, confirmed durable responses with ORR of 77%, uMRD in peripheral blood of 30%, and estimated 24-month PFS of 50% [38]. These findings led to the initial FDA approval of venetoclax in 2016 for CLL with 17p deletion in patients who have received at least one prior therapy [41].
Combination Therapy and Fixed-Duration Regimens
Despite its effectiveness as monotherapy, venetoclax is increasingly used in combination regimens to achieve deeper, more durable responses while allowing for fixed-duration treatment. The landmark MURANO study demonstrated superior efficacy of venetoclax-rituximab (VenR) compared with bendamustine-rituximab (BR), with significantly higher uMRD rates at the 9-month assessment (62% vs. 13%) [38]. The 5-year follow-up analysis sustained PFS and overall survival (OS) benefits for VenR versus BR (PFS 52.6 months vs. 17 months and OS 82% vs. 61%, respectively) [38]. Similarly, the CLL14 study established venetoclax-obinutuzumab as a fixed-duration frontline option for CLL patients with comorbidities, showing significantly longer PFS than chlorambucil-obinutuzumab (median PFS not reached vs. 35.6 months) [38]. These combination approaches have transformed treatment paradigms, offering chemotherapy-free alternatives with finite duration, particularly beneficial for elderly patients and those with significant comorbidities.
Table 1: Key Clinical Trials of Venetoclax in CLL
| Trial Name | Study Population | Regimen | Key Efficacy Findings | Reference |
|---|---|---|---|---|
| Phase I First-in-Human | R/R CLL, high-risk | Venetoclax monotherapy | ORR 79%, CR 20%, uMRD 15%, 15-month PFS 69% | [38] |
| Phase II Expansion | R/R CLL with del(17p) | Venetoclax monotherapy | ORR 77%, uMRD 30%, 24-month PFS 50% | [38] |
| MURANO | R/R CLL | VenR vs BR | uMRD 62% vs 13%; 5-yr PFS 52.6 vs 17 mo; OS 82% vs 61% | [38] |
| CLL14 | Treatment-naïve CLL with comorbidities | Ven-Obi vs Clb-Obi | PFS HR 0.31; median PFS NR vs 35.6 mo | [38] |
Venetoclax in Acute Myeloid Leukemia (AML)
Overcoming Therapeutic Challenges in AML
The treatment landscape for AML, particularly in older and unfit patients, has historically been dismal, with 5-year survival rates below 30% even in younger adults [39]. For elderly or frail patients ineligible for intensive chemotherapy, outcomes were especially poor, with 80-90% of patients over 80 years experiencing treatment failure with historical alternatives [39]. The combination of venetoclax with hypomethylating agents (azacitidine or decitabine) or low-dose cytarabine (LDAC) has dramatically altered this paradigm. Although venetoclax demonstrates limited efficacy as a single agent in AML, its combination with HMAs has shown encouraging outcomes, including rapid and durable responses with acceptable toxicity profiles in the older, unfit patient population [38] [39]. This combination represents the most significant advancement in AML therapy in decades, offering a viable, effective option for a patient population previously lacking satisfactory treatments.
Efficacy Data and Response Patterns
In clinical trials, venetoclax-based combinations have demonstrated substantially improved response rates compared to HMA monotherapy. Prior to venetoclax combinations, azacitidine alone yielded an overall response rate (ORR) of 29.9% and median overall survival of 10.4 months in unfit AML patients [39]. The addition of venetoclax to HMAs or LDAC has significantly enhanced efficacy, with deep remissions observed even in patients with adverse risk profiles, although specific response rates from the searched literature require supplementation with additional clinical trial data. Importantly, emerging evidence indicates that not all AML patients benefit equally from venetoclax-based therapy, with particular resistance observed in certain molecular subtypes, prompting investigations into predictive biomarkers and resistance mechanisms [42] [39].
Emerging Resistance Mechanisms
Molecular Drivers of Venetoclax Resistance
Despite impressive initial responses, resistance to venetoclax presents a significant clinical challenge. Multiple mechanisms of resistance have been identified, frequently emerging in a subclonal pattern through clonal evolution [38] [39]. The strongest predictors of venetoclax resistance in AML include TP53 mutations and complex karyotype, while IDH2 and SRSF2 mutations predict favorable responses [42]. TP53-mutated AML blasts demonstrate significantly reduced ex vivo sensitivity to venetoclax, potentially due to decreased BCL-2 protein expression and impaired BAX/BAK activation [42]. Functional analyses have revealed that dual inhibition of BCL-2 and BCL-xL via navitoclax can induce apoptosis in TP53-mutated blasts, suggesting a promising approach for this high-risk subgroup [42].
Anti-apoptotic Protein Adaptations
A primary resistance mechanism involves compensatory upregulation of alternative anti-apoptotic BCL-2 family members, particularly MCL-1 and BCL-xL [39] [43]. When BCL-2 is inhibited by venetoclax, cancer cells may become dependent on these other pro-survival proteins, effectively bypassing the apoptotic blockade. In multiple myeloma, acquired venetoclax resistance is associated with upregulation of BCL-xL and MCL-1, along with downregulation of pro-apoptotic members [43]. Similarly, in AML, venetoclax resistance frequently correlates with MCL-1 upregulation [39]. Upstream signaling pathways, including growth factor receptor tyrosine kinases (RTKs) and phosphoinositide-3-kinase (PI3K), contribute to this dysregulation, suggesting potential combinatorial targets for overcoming resistance [43].
Figure 2: Mechanisms of Venetoclax Resistance. Multiple pathways contribute to venetoclax resistance, including upregulation of alternative anti-apoptotic proteins, TP53 mutations, and activation of upstream signaling pathways.
Research Methodologies and Experimental Approaches
Assessing Venetoclax Sensitivity and Resistance
The determination of venetoclax sensitivity and investigation of resistance mechanisms employs a multifaceted experimental approach. BH3 profiling represents a key functional assay that measures mitochondrial priming and anti-apoptotic dependencies by exposing isolated mitochondria to synthetic BH3 peptides and quantifying cytochrome c release [37]. This technique can identify "primed" cells highly susceptible to venetoclax and determine their specific anti-apoptotic dependencies (BCL-2, BCL-xL, or MCL-1). For resistance studies, venetoclax-resistant cell lines are generated through prolonged exposure to increasing drug concentrations, followed by comprehensive molecular characterization [43]. Multi-omic approaches, including whole exome sequencing, RNA sequencing, and quantitative proteomics, are employed to identify genetic, transcriptional, and proteomic alterations associated with the resistant phenotype [43].
Key Research Reagents and Model Systems
Table 2: Essential Research Reagents for Venetoclax Resistance Studies
| Reagent/Category | Specific Examples | Research Application | Reference |
|---|---|---|---|
| BH3 Mimetics | Venetoclax (BCL-2), A-1331852 (BCL-xL), S-63845 (MCL-1) | Target-specific apoptotic profiling and combination studies | [42] [40] |
| Cell Line Models | Established HMCLs, TP53-mutated AML lines, Venetoclax-resistant isogenic lines | In vitro modeling of disease and resistance mechanisms | [43] |
| Primary Patient Samples | CD138+ MM cells, AML blasts from peripheral blood or bone marrow | Ex vivo drug sensitivity testing and translational validation | [42] [43] |
| Pathway Inhibitors | PI3K inhibitors, RTK inhibitors (FGF/EGF/IGF1R), AURKA inhibitors | Targeting upstream signaling pathways implicated in resistance | [43] |
| Protein Stability Tools | Cycloheximide, protease inhibitors, acetylation/phosphorylation modulators | Investigating post-translational regulation of anti-apoptotic proteins | [43] |
Experimental Workflow for Resistance Characterization
Figure 3: Experimental Workflow for Venetoclax Resistance Studies. A systematic approach to characterizing resistance mechanisms involves model generation, multi-omic profiling, functional validation, and therapeutic combination screening.
Discussion and Future Perspectives
The introduction of venetoclax has fundamentally transformed treatment paradigms for CLL and AML, offering unprecedented efficacy particularly for elderly and unfit patients who previously had limited options. Its development exemplifies the successful translation of basic apoptosis research into clinically impactful targeted therapy. However, the emergence of resistance remains a significant challenge that threatens the long-term durability of responses. Future research directions should focus on rational combination strategies informed by resistance mechanisms, particularly the simultaneous targeting of multiple anti-apoptotic proteins (BCL-2, BCL-xL, and MCL-1) or the inhibition of upstream signaling pathways that drive their expression [43]. The application of functional assays like dynamic BH3 profiling may help guide patient-specific therapeutic combinations and sequence strategies [37]. Furthermore, investigating non-canonical roles of BCL-2 family proteins in mitochondrial dynamics, metabolism, and therapy resistance may reveal novel vulnerabilities [3] [37]. As the field advances, the integration of comprehensive molecular profiling with functional drug sensitivity testing will be essential to optimize venetoclax-based therapies and overcome resistance, ultimately improving outcomes for patients with hematologic malignancies.
The B-cell lymphoma 2 (BCL-2) protein family constitutes the fundamental regulators of the intrinsic (mitochondrial) apoptosis pathway, a crucial process for maintaining tissue homeostasis and eliminating damaged cells [22] [44]. The founding member, BCL-2, was discovered as the oncogene involved in the t(14;18) chromosomal translocation found in most follicular lymphomas, representing the first example of an oncogene that promotes cancer by inhibiting cell death rather than enhancing proliferation [22]. The BCL-2 family proteins are characterized by the presence of BCL-2 homology (BH) domains and are structurally and functionally classified into three subfamilies: (1) anti-apoptotic proteins (e.g., BCL-2, BCL-XL, MCL-1), which contain four BH domains (BH1-BH4); (2) pro-apoptotic effector proteins (e.g., BAX, BAK), which contain three BH domains; and (3) BH3-only proteins (e.g., BIM, BID, PUMA, NOXA), which act as cellular sentinels initiating apoptosis [22] [16] [44].
The anti-apoptotic proteins, including BCL-2 and BCL-XL, function to preserve mitochondrial integrity by preventing mitochondrial outer membrane permeabilization (MOMP), thereby inhibiting the release of cytochrome c and other pro-apoptotic factors [22]. Overexpression of these anti-apoptotic proteins is a hallmark of numerous cancers, contributing to tumor development, maintenance, and resistance to anti-cancer therapies [45] [22]. Consequently, targeting BCL-2 and BCL-XL has emerged as a promising therapeutic strategy for cancer treatment. This whitepaper explores three innovative targeting approaches: Proteolysis-Targeting Chimeras (PROTACs), Antibody-Drug Conjugates (ADCs), and BH4 domain targeting, providing a technical examination of their mechanisms, experimental methodologies, and research applications.
Proteolysis-Targeting Chimeras (PROTACs) for Targeted Protein Degradation
Mechanism and Molecular Design
PROTACs represent a groundbreaking therapeutic modality that hijacks the ubiquitin-proteasome system to achieve targeted protein degradation [45]. Unlike traditional small-molecule inhibitors that merely occupy an active site, PROTACs catalytically induce the complete degradation of the target protein. A typical PROTAC molecule is a heterobifunctional chimera comprising three essential elements: (1) a ligand that binds to the protein of interest (POI), such as BCL-2 or BCL-XL; (2) an E3 ubiquitin ligase recruitment ligand; and (3) a chemical linker connecting these two moieties [45].
The mechanism of action involves the PROTAC simultaneously engaging both the target protein and an E3 ubiquitin ligase, forming a ternary complex. This complex brings the E3 ligase into proximity with the target protein, facilitating its polyubiquitination. The ubiquitinated target protein is then recognized and degraded by the 26S proteasome [45] [22]. This approach is particularly advantageous for targeting BCL-2 family proteins because it offers the potential to overcome resistance mutations that might reduce drug binding affinity and achieves a more complete ablation of the target's function.
Key Experimental Data and Research Findings
Recent patent disclosures (WO 2023019165 A1 and WO 2023031215 A2) describe pro-apoptotic molecules with BCL-2 homology 3 (BH3) effector domains that can be incorporated into PROTAC designs [45]. These molecules are associated with constructs containing a granule-localizing domain and can be transferred from effector cells to target cells to induce apoptosis. The transition from inhibitors to degraders is exemplified by the development of PROTACs targeting BCL-XL, transforming the mechanism of action from inhibition to degradation [45].
Table 1: Quantitative Data on BCL-XL Degrader Compounds from Cell-Based Assays [45]
| Compound ID | EBC-1 Cell Viability IC₅₀ (nM) | BCL-XL Degradation DC₅₀ (nM) | E3 Ligase Used |
|---|---|---|---|
| Example 1 | < 10 | < 10 | VHL |
| Example 2 | 10 - 100 | 10 - 100 | Cereblon |
| Example 3 | 100 - 1000 | 100 - 1000 | VHL |
Experimental Protocols for PROTAC Development and Validation
Protocol 1: In Vitro Assessment of Protein Degradation
- Cell Line Selection and Culture: Use cancer cell lines with confirmed dependence on the target protein (e.g., BCL-XL-dependent lines). Culture cells according to ATCC recommendations.
- PROTAC Treatment: Seed cells in 96-well plates. The following day, treat with a concentration gradient of the PROTAC compound (typically ranging from 1 nM to 10 µM). Include controls (DMSO vehicle) and a positive control (e.g., established BH3 mimetic).
- Protein Harvest and Quantification: After incubation (usually 16-24 hours), lyse cells using RIPA buffer supplemented with protease and phosphatase inhibitors. Quantify total protein concentration using a kit such as the Pierce BCA Protein Assay Kit [45].
- Target Protein Detection:
- Option A (WES Assay): Utilize the automated WES system (or similar capillary-based immunoassay) according to the manufacturer's instructions. This method requires small sample volumes and provides quantitative data on protein levels [45].
- Option B (Western Blot): Separate proteins by SDS-PAGE, transfer to a PVDF membrane, and probe with antibodies specific for the target (e.g., anti-BCL-XL) and a loading control (e.g., GAPDH or β-Actin). Use chemiluminescence for detection.
- Data Analysis: Quantify band intensity using densitometry software. Normalize target protein levels to the loading control. Calculate DC₅₀ (concentration causing 50% degradation) and Dmax (maximum degradation achieved) using non-linear regression analysis in software such as GraphPad Prism.
Protocol 2: Functional Assessment of Apoptosis and Cell Viability
- Cell Viability Assay (CTG): After PROTAC treatment (e.g., 72 hours), equilibrate plates to room temperature. Add a volume of CellTiter-Glo (CTG) Reagent equal to the volume of cell culture medium. Shake for 2 minutes to induce cell lysis, then incubate for 10 minutes to stabilize the luminescent signal. Record luminescence, which is proportional to the amount of ATP present and thus the number of viable cells [45].
- Apoptosis Assay (Caspase Activation): Use caspase-Glo 3/7 assays to measure the activation of effector caspases, a key event in apoptosis. Follow the manufacturer's protocol, adding reagent directly to cells in culture and measuring luminescence after incubation.
The following diagram illustrates the core mechanistic workflow of a BCL-XL-targeting PROTAC, from molecular assembly to protein degradation.
Antibody-Drug Conjugates (ADCs) for Selective Drug Delivery
Rationale and Targeting Strategy
Antibody-Drug Conjugates (ADCs) offer a sophisticated strategy to achieve tumor-specific inhibition of BCL-2 family proteins, particularly BCL-XL, whose systemic inhibition causes dose-limiting thrombocytopenia due to the protein's essential role in platelet survival [22] [46]. ADCs are designed to deliver potent cytotoxic payloads selectively to cancer cells by conjugating these payloads to monoclonal antibodies that recognize tumor-associated antigens.
Upon binding to its target antigen on the cancer cell surface, the ADC is internalized via endocytosis. The linker connecting the antibody to the payload is then cleaved in the lysosomal compartment, releasing the active drug intracellularly [22]. This targeted approach minimizes on-target, off-tumor toxicities by restricting the payload's activity to antigen-expressing cells, thereby enhancing the therapeutic window for challenging targets like BCL-XL.
Key Research Reagents and Experimental Models
Table 2: Essential Research Tools for ADC Development Targeting BCL-2/BCL-XL
| Research Tool | Function/Description | Key Utility |
|---|---|---|
| Tumor Cell Lines (e.g., SCLC, NSCLC models) | Models with defined antigen expression and BCL-XL dependence. | In vitro and in vivo assessment of ADC efficacy and specificity. |
| Anti-Tumor Antigen mAbs (e.g., anti-EFNA4, anti-B7-H3) | The targeting moiety of the ADC. | Confers specificity for tumor cells expressing the target antigen. |
| Cleavable Linkers (e.g., dipeptide-based, sulfonate-containing) | Connects antibody to payload; designed for intracellular cleavage. | Ensures stable circulation and specific payload release in target cells. |
| BCL-XL Inhibitor Payload (e.g., derived from navitoclax) | The potent warhead that inhibits BCL-XL function. | Induces apoptosis in cancer cells upon intracellular release. |
| Patient-Derived Xenograft (PDX) Models | In vivo models with retained tumor microenvironment. | Preclinical evaluation of ADC efficacy and safety in a clinically relevant context. |
Experimental Workflow for ADC Evaluation
Protocol: In Vivo Efficacy and Toxicity Assessment of a BCL-XL-targeting ADC
- Animal Model Establishment: Inoculate immunocompromised mice (e.g., NSG or nude mice) subcutaneously with tumor cells or implant tumor fragments from PDX models [46].
- ADC Dosing and Administration: Randomize mice into groups (n=5-10) once tumors reach a predefined volume (e.g., 100-150 mm³). Administer the following via intravenous injection:
- Group 1: ADC at the test dose (e.g., 3-10 mg/kg).
- Group 2: Isotype control ADC (non-targeting antibody with same payload).
- Group 3: Naked antibody (without payload).
- Group 4: Vehicle control.
- Group 5: Standard-of-care chemotherapy (positive control). Dosing schedules are typically once weekly for 2-4 cycles.
- Efficacy Monitoring: Measure tumor dimensions 2-3 times per week using digital calipers. Calculate tumor volume using the formula: V = (length × width²) / 2. Monitor mouse body weight as an indicator of general health.
- Toxicity and Pharmacodynamic Analysis:
- Blood Collection: Collect blood at various timepoints for hematological and biochemical analysis.
- Platelet Count Monitoring: Perform serial complete blood counts (CBC) to specifically assess thrombocytopenia, the primary on-target toxicity of BCL-XL inhibition [46]. Compare platelet nadirs and recovery kinetics between the ADC and a systemically administered BCL-XL inhibitor (e.g., navitoclax).
- Tumor Tissue Analysis: At study endpoint, harvest tumors for immunohistochemistry (IHC) or Western blot analysis to confirm target engagement (e.g., decreased levels of pro-survival complexes) and induction of apoptosis (e.g., cleaved caspase-3 staining).
BH4 Domain Targeting: A Structurally Distinct Approach
Biological Rationale and Mechanistic Insights
While most BH3-mimetics target the hydrophobic groove formed by the BH1, BH2, and BH3 domains, the BH4 domain represents a structurally and functionally distinct therapeutic target. The BH4 domain, located at the N-terminus of anti-apoptotic BCL-2 proteins, is a stretch of approximately 20 amino acids organized in an α-helical structure and is essential for the anti-apoptotic function of BCL-2 [47] [48]. Deletion of the BH4 domain not only abolishes BCL-2's protective function but can convert it into a pro-apoptotic protein, demonstrating the domain's critical role [47].
The BH4 domain mediates interactions with a growing list of non-BCL-2 family proteins that regulate apoptosis and other cellular processes. Key interactions include:
- Bax Interaction: The BH4 domain can bind directly to pro-apoptotic Bax via a non-canonical mechanism, blocking its conformational activation and reinforcing its inactive, monomeric state [47] [48].
- IP3 Receptor (IP3R) Interaction: At the endoplasmic reticulum (ER), the BH4 domain binds to the inositol 1,4,5-trisphosphate receptor (IP3R), an intracellular calcium-release channel. This interaction inhibits IP3R-dependent channel opening, diminishing Ca²⁺ release from the ER and thereby inhibiting Ca²⁺-mediated apoptosis [47].
Small molecules that disrupt these critical protein-protein interactions by targeting the BH4 domain can effectively induce apoptosis. This approach may overcome resistance to BH3-mimetics that target the canonical hydrophobic groove.
Key Compounds and Experimental Evidence
BDA-366 is a first-in-class, small-molecule antagonist of the BCL-2 BH4 domain. Proof-of-concept studies have demonstrated that it binds to the BH4 domain, inducing a conformational change in BCL-2 that converts it from a survival promoter to a cell death inducer [47] [48]. This highlights the unique therapeutic potential of BH4 domain inhibition.
Table 3: Functional Profile of BH4 Domain-Targeting Compound BDA-366 [47] [48]
| Parameter | Observation/Effect | Experimental Model |
|---|---|---|
| Molecular Target | BH4 domain of BCL-2 | NMR spectroscopy, binding assays |
| Conformational Change | Converts BCL-2 from anti-apoptotic to pro-apoptotic | Structural studies, functional assays |
| Effect on BCL-2/Bax Interaction | Disrupts the non-canonical, inhibitory interaction | Co-immunoprecipitation, Bax activation assays |
| Effect on BCL-2/IP3R Interaction | Inhibits binding, leading to enhanced pro-apoptotic Ca²⁺ signaling | Ca²⁺ flux assays, pulldown experiments |
| Therapeutic Outcome | Induction of apoptosis in cancer cells | Cell viability assays, caspase activation |
Experimental Protocol for Assessing BH4 Domain Function
Protocol: Investigating BH4 Domain-Dependent Protein-Protein Interactions
- Construct Generation:
- Cell Transfection and Treatment:
- Transfect cells (e.g., HEK293T or a relevant cancer cell line) with the generated constructs.
- Treat cells with the BH4-targeting compound (e.g., BDA-366) or vehicle control.
- Co-Immunoprecipitation (Co-IP):
- Lyse cells in a mild, non-denaturing lysis buffer.
- Incubate the cell lysate with an antibody against your protein of interest (e.g., BCL-2 or the tag on the BH4 peptide) and Protein A/G beads.
- Include an isotype control antibody to confirm binding specificity.
- Analysis of Interacting Partners:
- Wash the beads extensively to remove non-specifically bound proteins.
- Elute the bound proteins by boiling in SDS-PAGE sample buffer.
- Analyze the eluates by Western blotting, probing for putative interacting partners (e.g., Bax, IP3R).
The diagram below summarizes the functional consequences of targeting the BCL-2 BH4 domain, contrasting the survival state maintained by the BH4 domain with the pro-apoptotic state induced by its inhibition.
The Scientist's Toolkit: Key Research Reagent Solutions
This section provides a consolidated reference for essential reagents and tools used in the development and analysis of these novel targeting approaches, as derived from the experimental contexts provided.
Table 4: Essential Research Reagents for Novel BCL-2/BCL-XL Targeting Strategies
| Reagent / Assay Kit | Specific Function / Target | Key Application in Research |
|---|---|---|
| CellTiter-Glo (CTG) Assay | Measures cellular ATP levels as a proxy for cell viability. | Quantifying the anti-proliferative and cytotoxic effects of PROTACs, BH4 antagonists, and other inhibitors [45]. |
| Caspase-Glo 3/7 Assay | Measures the catalytic activity of effector caspases-3 and -7. | Confirming the induction of apoptosis as a mechanism of action for test compounds [46]. |
| WES / Jess Automated Immunoassay | Capillary-based Western blotting; requires minimal sample. | Rapid, quantitative analysis of target protein degradation (e.g., BCL-XL) in PROTAC studies [45]. |
| Nano-Glo HiBiT Assay | Utilizes a small peptide tag (HiBiT) that generates luminescence when complemented with LgBiT. | Highly sensitive and quantitative measurement of protein degradation kinetics for tagged proteins of interest [45]. |
| Pierce BCA Protein Assay | Colorimetric detection and quantification of total protein. | Standard protocol for normalizing protein concentrations prior to Western blot or other protein analyses [45]. |
| TAT-BH4 Peptide | Cell-penetrating peptide corresponding to the BCL-2 BH4 domain. | Tool for studying BH4 domain function; acts as a competitive inhibitor of endogenous BH4-mediated interactions [47]. |
| Navitoclax (ABT-263) | Small-molecule inhibitor of BCL-2, BCL-XL, and BCL-w. | Benchmark compound for assessing BCL-2/XL inhibition; positive control in viability and apoptosis assays [16]. |
| E3 Ligase Ligands (e.g., for VHL or Cereblon) | Binds and recruits specific E3 ubiquitin ligases. | Critical component in the design and synthesis of PROTAC molecules [45]. |
The relentless pursuit of novel cancer therapeutics has driven the evolution of strategies targeting the BCL-2 family beyond conventional small-molecule inhibitors. The three approaches detailed in this whitepaper—PROTACs, ADCs, and BH4 domain targeting—each offer distinct mechanisms to overcome the historical challenges of on-target toxicity and drug resistance associated with inhibiting BCL-2 and BCL-XL.
PROTACs provide a catalytic, event-driven modality that can degrade target proteins entirely, potentially circumventing resistance mutations. ADCs offer a precision medicine approach to deliver the potent cytotoxicity of BCL-XL inhibition specifically to tumor cells, thereby sparing platelets and other sensitive tissues. Finally, targeting the BH4 domain represents a paradigm shift by attacking a functionally critical but structurally distinct region of BCL-2, which may prove effective against cancers resistant to BH3-mimetics.
The experimental protocols and research tools outlined herein provide a foundational framework for scientists to further investigate and refine these innovative strategies. As research progresses, the integration of these novel targeting approaches into combination regimens holds significant promise for expanding the therapeutic arsenal against a broad spectrum of cancers dependent on BCL-2 and BCL-XL for survival.
Overcoming Resistance and Toxicity in Bcl-2/Bcl-xL Targeted Therapy
Treatment resistance represents a significant challenge in oncology, particularly in therapies targeting the B-cell lymphoma 2 (BCL-2) family of proteins. This technical review examines the fundamental mechanisms by which cancer cells evade apoptosis through genetic mutations and altered protein interactions within the BCL-2 family, with specific focus on BCL-2 and BCL-xL. We synthesize current research on resistance mechanisms against BH3-mimetic drugs, including venetoclax, through detailed analysis of mutation profiles, compensatory survival pathways, and experimental approaches for identification and characterization. The complex interplay between anti-apoptotic proteins and their pro-apoptotic counterparts creates a dynamic equilibrium that malignant cells exploit to survive therapeutic pressure. Understanding these mechanisms provides critical insights for developing next-generation strategies to overcome resistance in hematological malignancies and solid tumors.
The BCL-2 family of proteins constitutes the essential regulatory network controlling the intrinsic (mitochondrial) apoptosis pathway. These proteins are categorized into three functional classes based on their BCL-2 homology (BH) domains and apoptotic function: (1) anti-apoptotic multidomain proteins (e.g., BCL-2, BCL-xL, MCL-1); (2) pro-apoptotic multidomain effectors (BAX, BAK); and (3) BH3-only pro-apoptotic proteins (BIM, BID, PUMA, BAD, NOXA) [13] [49]. The balance between these competing factions determines cellular fate through regulation of mitochondrial outer membrane permeabilization (MOMP), the critical commitment point in apoptosis [13].
BCL-2 and BCL-xL function as guardians of cellular survival by sequestering pro-apoptotic proteins, particularly the activator BH3-only proteins (BIM, tBID) and the effectors BAX/BAK [50] [13]. In their anti-apoptotic role, they prevent the conformational activation and oligomerization of BAX/BAK that would otherwise form pores in the mitochondrial membrane, leading to cytochrome c release and caspase activation [49]. The "direct activation" model posits that activator BH3-only proteins directly engage and activate BAX/BAK, while "sensitizer" BH3-only proteins neutralize anti-apoptotic proteins by displacing bound activators [13]. Alternatively, the "embedded together" model suggests these interactions occur primarily at mitochondrial membranes, where conformational changes alter binding affinities [13].
The critical role of BCL-2 and BCL-xL in oncogenesis is evidenced by their frequent dysregulation across hematological malignancies and solid tumors. Chromosomal translocations such as t(14;18) in follicular lymphoma result in BCL-2 overexpression, while epigenetic regulation and miRNA loss (e.g., miR-15/16 in CLL) further contribute to aberrant expression [49] [3]. This molecular context establishes the foundation for understanding how therapeutic targeting of these proteins can be undermined through diverse resistance mechanisms.
Genetic Mutations in BCL-2 Family Proteins
BCL-2 Mutations Conferring Resistance to BH3 Mimetics
Somatic mutations in BCL-2 itself represent a direct mechanism of resistance to venetoclax and related BH3-mimetic compounds. Structural analyses have identified specific point mutations within the BH3-binding groove that diminish drug affinity while largely preserving native protein functions.
Table 1: Characterized BCL-2 Mutations in Venetoclax Resistance
| Mutation | Location | Structural Impact | Functional Consequence | Clinical Context |
|---|---|---|---|---|
| G101V | BH3-binding domain | Bulkier valine sidechain causes helical shifts | Reduced venetoclax binding affinity | Acquired resistance in CLL after 2-3 years of treatment |
| D103Y | BH3-binding pocket | Tyrosine extension into binding pocket | Disrupts hydrogen bonding with venetoclax | Identified in refractory CLL |
| F104L/V | BH3-binding pocket | Alters key structural residue | Compromises drug binding interface | In vitro models |
The G101V mutation represents the most frequently observed resistance mutation in chronic lymphocytic leukemia patients undergoing long-term venetoclax treatment [51]. This substitution occurs at the glycine 101 position, where replacement with valine introduces bulkier methyl groups that provoke conformational shifts in the α-helical structure of BCL-2. Dynamic modeling demonstrates that these shifts affect residues within the BH3-binding pocket (including F104), reducing venetoclax binding affinity without completely abolishing interaction with native BH3 ligands like BIM [51]. This partial preservation of function allows malignant cells to maintain anti-apoptotic activity while evading therapeutic inhibition.
The D103Y mutation presents a distinct mechanism, directly targeting residues critical for venetoclax binding. Aspartate 103 forms a crucial hydrogen bond with the indole ring of venetoclax, and its substitution with tyrosine extends a bulkier side chain into the binding pocket, sterically hindering drug engagement [51]. This mutation occurs at a position that differs between BCL-2 and BCL-xL, explaining the selectivity of venetoclax for BCL-2 over BCL-xL [51]. In clinical samples, these mutations often emerge as subclonal populations that expand under therapeutic pressure, with variant allele frequencies increasing over time and typically remaining below 50%, suggesting the presence of complementary resistance mechanisms [51].
Experimental Protocols for Mutation Detection
Method 1: Longitudinal Genetic Monitoring for BCL-2 Mutations
- Objective: To identify acquired BCL-2 mutations in patients undergoing venetoclax treatment.
- Sample Collection: Peripheral blood or bone marrow aspirates collected at baseline, during treatment (e.g., every 3-6 months), and at suspected progression.
- Cell Enrichment: CD19+ selection via magnetic-activated cell sorting (MACS) to enhance tumor purity (critical in CLL with low peripheral lymphocyte counts).
- Genetic Analysis:
- Whole Exome Sequencing (WES): Perform on paired tumor and non-malignant samples (e.g., CD19-negative fraction) to unbiasedly identify novel variants. Library preparation using Illumina TruSeq, sequencing at 100x minimum coverage.
- Targeted Amplicon Sequencing: Design primers flanking BCL-2 BH3-binding domain (codons 95-115). Use deep sequencing (>500x coverage) to detect low-frequency subclones.
- Variant Validation: Confirm mutations in multiple tissue compartments (spleen, bone marrow, blood) and track variant allele frequency (VAF) over time.
- Data Interpretation: Mutations present at progression but absent at baseline indicate acquired resistance. Increasing VAF suggests clonal selection under therapeutic pressure [51].
Method 2: Structural Modeling of Mutation Impact
- Objective: To predict functional consequences of identified BCL-2 mutations.
- Homology Modeling: Generate mutant protein structures using wild-type BCL-2 (PDB: 6O0K) as template.
- Molecular Dynamics Simulations:
- Employ software such as GROMACS or AMBER for simulated protein folding and dynamics.
- Measure atomic distances between mutated residues (e.g., G101V) and neighboring residues (E152, V148, F104, Y18) to evaluate steric clashes.
- Calculate binding free energies for venetoclax and BH3 peptides to mutant versus wild-type BCL-2 using molecular mechanics Poisson-Boltzmann surface area (MM-PBSA) methods.
- Experimental Validation: Compare in vitro binding affinity (surface plasmon resonance) and cellular apoptosis assays in isogenic cell lines expressing wild-type versus mutant BCL-2 [51].
Altered Protein Interactions and Compensatory Mechanisms
Upregulation of Alternative Anti-apoptotic Proteins
Beyond direct mutations, cancer cells evade BCL-2 inhibition by activating compensatory survival pathways through other anti-apoptotic family members. The most characterized mechanism involves increased expression of MCL-1 and BCL-xL, which can sequester pro-apoptotic proteins released from BCL-2 inhibition, maintaining repression of mitochondrial apoptosis.
Table 2: Compensatory Anti-apoptotic Proteins in Treatment Resistance
| Protein | Mechanism of Resistance | Malignancies Involved | Therapeutic Approaches |
|---|---|---|---|
| MCL-1 | Binds BIM displaced from BCL-2 | AML, NHL, multiple myeloma | MCL-1 inhibitors (S63845, AZD5991) |
| BCL-xL | Sequesters BIM and BAX | CLL, AML, lymphoma | BCL-xL inhibitors (A-1155463), navitoclax |
| BFL-1 | Low affinity for venetoclax, binds freed BH3 proteins | CLL, some solid tumors | Experimental compounds |
When venetoclax occupies the BH3-binding groove of BCL-2, it displaces bound pro-apoptotic proteins, particularly BIM. In resistant cells, elevated MCL-1 and/or BCL-xL capture this liberated BIM, preventing it from activating BAX/BAK [52]. The relative importance of these compensatory proteins varies by malignancy; in CLL, the hierarchy of BIM binding affinity is BCL-2 > BCL-xL > MCL-1 > BFL-1, suggesting BCL-xL may play a more significant role than MCL-1 in this context [52]. In acute myeloid leukemia, particularly subtypes with monocytic differentiation, MCL-1 upregulation is a predominant resistance mechanism [52].
The expression of these alternative anti-apoptotic proteins is regulated through multiple signaling pathways. Microenvironmental signals such as CD40L, interleukin-10, and unmethylated DNA activate the PI3K/AKT/mTOR pathway, which in turn stimulates NF-κB signaling to promote transcription of MCL-1 and BCL-xL [52]. This mechanism illustrates how extrinsic survival signals can confer intrinsic drug resistance.
Experimental Protocols for Protein Interaction Studies
Method 1: Mitochondrial Apoptosis Priming (BH3 Profiling)
- Objective: To measure functional dependence on specific anti-apoptotic proteins and predict sensitivity to BH3 mimetics.
- Cell Preparation: Isolate primary tumor cells or maintain cell lines in logarithmic growth phase. Include positive (permeabilized with digitonin) and negative (DMSO-only) controls.
- Peptide Exposure: Treat cells with standardized BH3-only peptides (0.1-100 μM) representing different binding specificities:
- BAD (BCL-2, BCL-xL, BCL-w dependence)
- HRK (BCL-xL dependence)
- MS1 (MCL-1 dependence)
- BIM (pan-dependence)
- Mitochondrial Membrane Potential Assessment:
- Permeabilize cells with 0.002% digitonin in mitochondrial assay buffer.
- Incubate with BH3 peptides for 60 minutes at room temperature.
- Add JC-1 dye (5,5',6,6'-tetrachloro-1,1',3,3'-tetraethylbenzimidazolylcarbocyanine iodide) to measure mitochondrial membrane potential (ΔΨm) by flow cytometry.
- Data Analysis: Calculate percentage of depolarized mitochondria for each peptide. High response to BAD peptide indicates BCL-2 dependence; resistance to BAD but sensitivity to HRK/MS1 suggests MCL-1/BCL-xL-mediated resistance [13] [49].
Method 2: Co-immunoprecipitation for Protein Complexes
- Objective: To quantify interactions between anti-apoptotic and pro-apoptotic proteins in resistant versus sensitive cells.
- Cell Lysis: Use mild lysis buffer (1% CHAPS, 150 mM NaCl, 10 mM HEPES) to preserve native protein complexes.
- Immunoprecipitation:
- Incubate lysates with antibodies against target proteins (BCL-2, BCL-xL, MCL-1) or isotype control IgG overnight at 4°C.
- Add protein A/G beads for 2 hours, then wash extensively.
- Western Blot Analysis:
Visualization of Resistance Pathways
Figure 1: Molecular Pathways in Venetoclax Resistance. This diagram illustrates the mechanistic basis of sensitivity and resistance to BCL-2 inhibition. In sensitive cells (green pathway), venetoclax binds BCL-2, displacing BIM to activate apoptosis. Resistance arises through BCL-2 mutations that impair drug binding (red) or compensatory upregulation of MCL-1/BCL-xL that sequester displaced BIM, maintaining survival signals.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Investigating BCL-2 Family Resistance Mechanisms
| Reagent/Category | Specific Examples | Research Application | Mechanistic Insight |
|---|---|---|---|
| BCL-2 Inhibitors | Venetoclax (ABT-199) | Selective BCL-2 inhibition | Baseline apoptosis induction; resistance modeling |
| BCL-xL Inhibitors | A-1155463, WEHI-539 | Target BCL-xL specifically | Assess compensatory BCL-xL dependence |
| MCL-1 Inhibitors | S63845, AZD5991 | Selective MCL-1 blockade | Evaluate MCL-1-mediated resistance |
| Pan-BCL-2 Inhibitors | Navitoclax (ABT-263) | Inhibit BCL-2, BCL-xL, BCL-w | Identify multi-protein dependence |
| Pathway Inhibitors | NVP-BEZ235 (PI3K/mTOR), BMS345541 (NF-κB) | Block survival signaling | Investigate upstream regulation of anti-apoptotic proteins |
| Caspase Inhibitors | QVD-OPh | Pan-caspase inhibition | Confirm apoptosis-specific phenotypes |
| BH3 Peptides | BIM, BAD, HRK, MS-1 | Mitochondrial priming assays (BH3 profiling) | Functional dependence on anti-apoptotic proteins |
| Antibodies | Anti-BCL-2, Anti-BCL-xL, Anti-MCL-1, Anti-BIM | Western blot, immunoprecipitation, flow cytometry | Protein expression and interaction studies |
Discussion and Therapeutic Implications
The emergence of resistance to BCL-2 targeted therapies represents a dynamic process of clonal evolution and adaptive cellular responses. Cancer cells employ multiple parallel strategies to maintain apoptotic repression, including primary target modification (BCL-2 mutations), compensatory pathway activation (MCL-1/BCL-xL upregulation), and potentially non-canonical BCL-2 functions related to mitochondrial dynamics and cellular metabolism [3] [52].
The temporal patterns of resistance development provide important insights into therapeutic strategy. BCL-2 mutations typically emerge after extended venetoclax exposure (2-3 years), suggesting that time-limited combination approaches may prevent their outgrowth [51]. In contrast, upregulation of MCL-1 and BCL-xL often represents an earlier, adaptive response that can be identified through functional assays like BH3 profiling [52].
Promising strategies to overcome resistance include:
- Rational combination therapies: Simultaneous targeting of BCL-2 with MCL-1 or BCL-xL to prevent compensatory survival.
- Sequential targeting: Prior therapies can alter tumor dependence on specific anti-apoptotic proteins, potentially sensitizing resistant populations.
- Vertical pathway inhibition: Combining BH3 mimetics with signaling pathway inhibitors (PI3K/AKT, NF-κB) to reduce expression of compensatory anti-apoptotic proteins.
- Metabolic targeting: Addressing the altered mitochondrial metabolism in resistant leukemia stem cells that contributes to survival independence.
Future research directions should focus on comprehensive characterization of the resistance landscape across different malignancies, development of predictive biomarkers for emerging resistance mechanisms, and innovative clinical trial designs that anticipate and preempt resistance evolution. The intricate balance within the BCL-2 family network ensures that therapeutic targeting will inevitably provoke adaptive responses, necessitating sophisticated approaches that address the dynamic nature of apoptotic regulation in cancer.
The B-cell lymphoma-extra large (Bcl-xL) protein is a critical anti-apoptotic regulator within the Bcl-2 family, serving as a promising therapeutic target for cancer treatment due to its frequent overexpression in solid tumors and role in therapy resistance. However, the clinical development of Bcl-xL inhibitors has been persistently challenged by a significant on-target toxicity: dose-limiting thrombocytopenia. This whitepaper examines the molecular mechanisms underlying this toxicity, evaluates emerging strategies to mitigate platelet toxicity while preserving antitumor efficacy, and synthesizes recent clinical data demonstrating the feasibility of achieving a therapeutic window for Bcl-xL targeting agents.
The Bcl-2 Protein Family and Apoptotic Regulation
The Bcl-2 family of proteins are fundamental regulators of the intrinsic apoptotic pathway, functioning through protein-protein interactions that control mitochondrial outer membrane permeabilization (MOMP) [53]. These proteins are categorized by their structure and function:
- Anti-apoptotic proteins (including Bcl-xL, Bcl-2, MCL-1, Bcl-W, and BFL-1/A1) contain multiple BCL-2 homology (BH) domains and promote cell survival by inhibiting MOMP.
- Pro-apoptotic effector proteins (BAX and BAK) contain multiple BH domains and execute apoptosis through homo-oligomerization and pore formation in the mitochondrial membrane.
- BH3-only proteins (BIM, BID, BAD, PUMA, NOXA, etc.) function as sentinels of cellular stress and initiate apoptosis by activating BAX/BAK or neutralizing anti-apoptotic proteins [53].
Bcl-xL, encoded by the BCL2L1 gene, is a transmembrane molecule located in the mitochondria that prevents the release of cytochrome c and other pro-apoptotic factors, thereby inhibiting caspase activation and programmed cell death [54]. The relative abundance of pro- and anti-apoptotic Bcl-2 family members constitutes a critical cellular checkpoint that determines susceptibility to apoptosis [50] [54].
Bcl-xL as a Therapeutic Target in Oncology
Bcl-xL has emerged as a particularly compelling oncology target because it serves as a primary survival factor for most solid tumors and contributes broadly to resistance against conventional chemotherapies and targeted agents [55] [53]. Unlike Bcl-2, whose overexpression is primarily associated with hematological malignancies, Bcl-xL is frequently overexpressed across diverse solid tumor types [56] [53]. Furthermore, Bcl-xL expression has been positively correlated with tumor resistance to anticancer therapies, making it an attractive target for overcoming treatment resistance [53]. Beyond its role in cancer, Bcl-xL has also been identified as a key survival factor for senescent cells, suggesting potential applications as a senolytic agent for age-related diseases and therapy-induced senescence [53].
The Thrombocytopenia Challenge: Mechanisms and Preclinical Evidence
Platelet Dependence on Bcl-xL
The central challenge in therapeutic Bcl-xL inhibition stems from the essential role Bcl-xL plays in platelet survival. Human platelets rely exclusively on Bcl-xL (rather than Bcl-2 or MCL-1) for their survival during their circulating lifespan [53]. This unique dependency arises because anucleate platelets lack transcriptional machinery and cannot dynamically regulate their apoptotic protein repertoire in response to survival challenges. Platelets consequently exhibit exceptional vulnerability to Bcl-xL inhibition, which rapidly triggers the intrinsic apoptotic pathway through BAK/BAX activation [57].
Evidence from Preclinical Models
Preclinical studies with small-molecule Bcl-xL inhibitors have consistently demonstrated rapid, dose-dependent thrombocytopenia across species. In canine models, the potent and selective Bcl-xL inhibitor A-1331852 induced severe thrombocytopenia (platelet counts as low as 5,000/μL) within 30 minutes of administration [57]. This thrombocytopenia was accompanied by additional cardiovascular toxicities, including myocardial capillary endothelial apoptosis, hydropericardium, and hemodynamic collapse [57]. Similar platelet effects were observed with navitoclax (ABT-263), a dual Bcl-2/Bcl-xL inhibitor that demonstrated dose-limiting thrombocytopenia in clinical trials despite showing activity in small cell lung cancer and hematological malignancies [55] [53].
Table 1: Preclinical Profile of Select Bcl-xL Inhibitors
| Compound | Target Specificity | Platelet IC₅₀ | Key Toxicities | Tumor Models with Activity |
|---|---|---|---|---|
| Navitoclax (ABT-263) | Bcl-2/Bcl-xL | <100 nM [53] | Thrombocytopenia, neutropenia [53] | SCLC, lymphoma [53] |
| A-1331852 | Bcl-xL | ~1 nM [57] | Thrombocytopenia, cardiovascular toxicity [57] | H146 SCLC xenografts [57] |
| WEHI-539 | Bcl-xL | ~10 nM [19] | Thrombocytopenia [19] | Not reported in available results |
The following diagram illustrates the fundamental mechanism of Bcl-xL inhibition-induced thrombocytopenia and the contrasting effect of PROTAC-based approaches:
Emerging Strategies to Mitigate Thrombocytopenia
PROTAC-Based Degradation Approach
Proteolysis Targeting Chimeras (PROTACs) represent a paradigm-shifting strategy that leverages the ubiquitin-proteasome system to achieve tissue-selective targeting. These heterobifunctional molecules consist of a Bcl-xL-binding pharmacophore linked to an E3 ubiquitin ligase-recruiting moiety, enabling targeted protein degradation rather than mere inhibition [53]. The key innovation lies in exploiting differential expression of the von Hippel-Lindau (VHL) E3 ligase between target tissues. Since human platelets express minimal VHL, they are largely spared from Bcl-xL degradation despite containing the target protein [55] [53].
DT2216 is the first Bcl-xL-targeting PROTAC to enter clinical trials. Preclinical studies demonstrated that DT2216 effectively degraded Bcl-xL in tumor cells while showing reduced platelet toxicity compared to navitoclax [55] [53]. The compound acts through the APTaD (Antiapoptotic Protein Targeted Degradation) mechanism, simultaneously engaging Bcl-xL and VHL to induce ubiquitination and proteasomal degradation of Bcl-xL [55].
Table 2: Comparison of Bcl-xL Targeting Modalities
| Approach | Mechanism | Advantages | Limitations | Development Status |
|---|---|---|---|---|
| Small Molecule Inhibitors (Navitoclax, A-1331852) | Competitive binding to Bcl-xL hydrophobic groove | Oral bioavailability, well-characterized | Significant thrombocytopenia, cardiovascular toxicity [57] | Phase II (navitoclax) [53] |
| PROTAC Degraders (DT2216) | Induces ubiquitination and degradation of Bcl-xL | Reduced platelet toxicity, sustained effect, catalytic mechanism [55] [53] | Requires intravenous administration, molecular weight challenges | Phase I (DT2216) [55] |
| Antibody-Drug Conjugates (Mirzotamab clezutoclax) | Targeted delivery to tumor cells expressing specific surface antigens | Bypasses systemic toxicity, improved therapeutic index [57] | Limited to tumors with appropriate antigen expression, complex manufacturing | Phase I (NCT03595059) [57] |
| Prodrug Strategies (APG-1252) | Phosphate prodrug converted to active compound in tissues | Reduced platelet exposure, potentially improved therapeutic window [53] | Conversion efficiency variable, still systemic exposure | Phase I (NCT03080311) [53] |
Antibody-Drug Conjugates (ADCs)
The ADC approach represents another promising strategy for circumventing thrombocytopenia by restricting Bcl-xL inhibitor delivery to tumor cells. Mirzotamab clezutoclax (AM1-25) is an EGFR-targeting ADC bearing a Bcl-xL-inhibiting warhead that demonstrated robust antitumor activity in xenograft models without causing dose-limiting thrombocytopenia or cardiovascular toxicity in monkey studies [57]. The ADC structure incorporates specialized linker technology to optimize stability and payload release, though unexpected renal toxicity observed in monkey models required further drug-linker optimization [57].
Clinical Validation of DT2216
Recent phase I clinical trial results (NCT04886622) provide compelling evidence that the PROTAC approach can successfully mitigate thrombocytopenia while maintaining antitumor activity. In this first-in-human study of DT2216 in patients with relapsed/refractory solid malignancies:
- Only one dose-limiting toxicity (grade 4 thrombocytopenia) was observed across all dose cohorts (0.04-0.4 mg/kg IV twice weekly), which resolved within 48 hours [55].
- Thrombocytopenia was transient and limited primarily to the first treatment cycle, with platelet counts recovering to >50,000/μL within 4 days and >75,000/μL within one week [55].
- Patients receiving 0.4 mg/kg DT2216 demonstrated rapid and sustained degradation of Bcl-XL in peripheral leukocytes, confirming target engagement [55].
- The recommended phase 2 dose was established as 0.4 mg/kg IV twice weekly, with a median overall survival of 7.9 months and disease stabilization in 20% of patients [55].
The following diagram illustrates the key mechanistic differences between conventional inhibitors and PROTAC degraders:
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Bcl-xL and Thrombocytopenia Studies
| Reagent/Category | Specific Examples | Key Applications | Mechanistic Insight |
|---|---|---|---|
| Small Molecule Inhibitors | Navitoclax (ABT-263), A-1331852, WEHI-539 [57] [19] [58] | Establishing proof-of-concept, in vitro and in vivo efficacy studies | Demonstrate intrinsic thrombocytopenia risk of Bcl-xL inhibition [57] |
| PROTAC Degraders | DT2216 [55] [53] | Evaluating tissue-selective degradation, platelet-sparing strategies | Validate VHL-dependent degradation selectivity [55] |
| Antibody-Drug Conjugates | Mirzotamab clezutoclax (AM1-25) [57] | Tumor-targeted delivery approaches, therapeutic index optimization | Demonstrate targeted payload delivery to antigen-expressing tumors [57] |
| Platelet Assays | Flow cytometry (ApoAlert APO 2.7), platelet counting, activation markers [57] [59] | Quantifying thrombocytopenia, platelet apoptosis and function | Establish platelet-specific toxicity profiles and recovery kinetics [55] |
| Cell Viability/Cytotoxicity Assays | Caspase activation (DEVD-AMC cleavage), mitochondrial membrane potential, ATP content [19] [59] | Measuring apoptosis induction in tumor cells and platelets | Differentiate cytotoxic mechanisms between cell types [19] |
| Protein Degradation Assessment | Western blotting, immunofluorescence, ubiquitination assays [55] [19] | Confirming target engagement and degradation efficiency | Verify Bcl-xL degradation in tumor cells but not platelets [55] |
| Animal Models | Mouse xenograft models, canine cardiovascular toxicity models [55] [57] | Evaluating efficacy, platelet toxicity, and additional toxicities | Identify species-specific toxicities (e.g., cardiovascular in dogs) [57] |
Experimental Protocols for Key Assessments
Protocol 1: Platelet Toxicity AssessmentIn Vivo
Purpose: To evaluate the kinetics and severity of thrombocytopenia following Bcl-xL inhibitor administration.
Materials: Test compound (e.g., DT2216, navitoclax), appropriate animal model (typically murine or canine), blood collection tubes containing anticoagulant (EDTA or citrate), automated hematology analyzer.
Procedure:
- Administer single intravenous dose of test compound at designated concentration (e.g., 0.04-0.4 mg/kg for DT2216) [55].
- Collect blood samples pre-dose and at specified timepoints post-dose (e.g., 1, 4, 24, 48, 72 hours).
- Analyze platelet counts using automated hematology analyzer.
- Monitor for platelet recovery: record time to nadir, time to recovery to >50,000/μL and >75,000/μL [55].
- Compare platelet kinetics between first and subsequent treatment cycles to assess adaptation.
Key Parameters: Platelet nadir, time to recovery, bleeding manifestations, differential effects between dosing cycles.
Protocol 2: Bcl-xL Degradation Assessment in Peripheral Leukocytes
Purpose: To confirm target engagement and degradation efficiency in clinical specimens.
Materials: Patient peripheral blood samples, leukocyte separation media, lysis buffer, Western blot equipment, Bcl-xL specific antibodies, loading controls.
Procedure:
- Collect peripheral blood samples pre-dose and at specified timepoints post-dose (e.g., 1, 4, 24 hours).
- Isolate peripheral blood mononuclear cells (PBMCs) using density gradient centrifugation.
- Lyse cells in RIPA buffer supplemented with protease and phosphatase inhibitors.
- Quantify protein concentration and separate equal amounts by SDS-PAGE.
- Transfer to PVDF membrane and probe with anti-Bcl-xL antibody.
- Detect using enhanced chemiluminescence and quantify band intensity normalized to loading control.
- Compare Bcl-xL expression levels relative to pre-dose samples [55].
Key Parameters: Percentage Bcl-xL degradation relative to baseline, duration of degradation, correlation with pharmacokinetic parameters.
The successful clinical development of DT2216 represents a paradigm shift in targeting Bcl-xL, demonstrating that on-target thrombocytopenia can be mitigated through protein degradation strategies without compromising antitumor activity. The differential expression of VHL E3 ligase between tumor cells and platelets creates a therapeutic window that cannot be achieved with conventional small-molecule inhibitors. Future directions should focus on optimizing combination regimens that leverage the synergistic potential of Bcl-xL degradation with conventional chemotherapy and targeted agents, particularly in Bcl-xL-dependent solid tumors. Additionally, further investigation into potential resistance mechanisms to PROTAC-mediated degradation and the development of next-generation degraders recruiting alternative E3 ligases may expand the therapeutic index. As these novel approaches advance through clinical development, the longstanding challenge of thrombocytopenia associated with Bcl-xL inhibition appears increasingly surmountable.
The B-cell lymphoma 2 (BCL-2) family of proteins constitutes a critical regulatory network that governs the intrinsic, mitochondrial pathway of apoptosis, a fundamental process for maintaining tissue homeostasis and eliminating damaged cells [60]. This protein family is categorized into anti-apoptotic members (including BCL-2, BCL-xL, and MCL-1) and pro-apoptotic members (such as BAX, BAK, and BIM), whose dynamic interactions determine cellular fate [61]. The equilibrium between these competing factions is frequently disrupted in cancer, where overexpression of anti-apoptotic proteins like BCL-2 and BCL-xL enables tumor cells to evade programmed cell death, thereby facilitating tumor survival, progression, and resistance to conventional chemotherapeutics [62] [61]. This dysregulation establishes these proteins as rational and compelling targets for cancer therapy.
The development of BH3-mimetics, such as the BCL-2-selective inhibitor venetoclax, represents a paradigm shift in targeting apoptotic pathways. These small molecules mimic the function of pro-apoptotic BH3-only proteins by binding to the hydrophobic grooves of anti-apoptotic BCL-2 family proteins, thereby displacing sequestered pro-apoptotic effectors like BIM and BAX to initiate mitochondrial outer membrane permeabilization (MOMP) and caspase activation [62]. Despite impressive clinical efficacy, particularly in hematological malignancies like chronic lymphocytic leukemia (CLL), resistance to single-agent BH3-mimetics frequently emerges [62]. Resistance mechanisms are multifaceted and include upregulation of alternative anti-apoptotic proteins (e.g., MCL-1 or BCL-xL), metabolic adaptations, and complex clonal evolution [62] [63]. Consequently, rational combination therapies designed to preempt or overcome these resistance mechanisms are imperative to enhance therapeutic efficacy, deepen clinical responses, and improve patient outcomes.
Core Mechanisms of BCL-2 Family Proteins
Molecular Regulation of Apoptosis
The BCL-2 family proteins regulate a critical checkpoint in the intrinsic apoptotic pathway, primarily controlling mitochondrial outer membrane permeabilization (MOMP). Following cellular stress signals (e.g., DNA damage, oncogenic stress), the activation of "activator" BH3-only proteins (like BIM and tBID) leads to the direct activation of the pro-apoptotic effectors BAX and BAK [60]. Once activated, BAX and BAK oligomerize to form pores in the mitochondrial outer membrane, facilitating the release of cytochrome c and other apoptogenic factors into the cytosol. This triggers the formation of the apoptosome and the subsequent cascade of caspase activation, culminating in organized cellular dismantling [60]. Anti-apoptotic proteins, including BCL-2, BCL-xL, and MCL-1, function as central guardians of this process by sequestering the activator BH3-only proteins and preventing the initiation of BAX/BAK activation [62] [60]. The figure below illustrates the core apoptotic pathway and the points of inhibition by BCL-2/BCL-xL.
Beyond their canonical role in apoptosis, BCL-2 proteins are integral to cellular homeostasis, critically regulating processes such as autophagy, mitochondrial dynamics, and metabolism [61]. For instance, BCL-2 inhibits excessive autophagy by directly binding to the BH3 domain of Beclin-1, a key autophagy initiation protein [61]. This interaction maintains cellular homeostasis under normal conditions but can be disrupted by post-translational modifications (e.g., phosphorylation) under stress, shifting the cellular balance towards autophagic degradation or death [61]. The interplay between these pathways adds a layer of complexity to the cellular response to therapeutic inhibition of BCL-2 proteins.
Established Therapeutic Inhibitors
The translation of mechanistic insights into clinical therapeutics has yielded a class of drugs known as BH3-mimetics. These agents are designed to specifically antagonize the pro-survival function of BCL-2 family proteins.
Table 1: Established BH3-mimetic Inhibitors Targeting BCL-2 Family Proteins
| Inhibitor Name | Primary Target(s) | Key Clinical/Preclinical Context | Notable Challenges |
|---|---|---|---|
| Venetoclax (ABT-199) | BCL-2 | FDA-approved for CLL and AML; high single-agent activity [62]. | Resistance via MCL-1 or BCL-xL upregulation [62]. |
| Navitoclax (ABT-263) | BCL-2, BCL-xL | Shows efficacy in lymphoid malignancies and SCLC [63]. | On-target thrombocytopenia due to BCL-xL inhibition [63]. |
| Obatoclax | MCL-1, BCL-2 | Preclinical candidate, used in research settings [61]. | Lower specificity, neurological side effects. |
The distinct target profiles of these inhibitors dictate their therapeutic utility and toxicity profiles. For example, the dose-limiting thrombocytopenia associated with navitoclax is a direct consequence of BCL-xL inhibition, which is essential for platelet survival [63]. This underscores the necessity for rational drug combinations that can enhance anti-tumor efficacy while mitigating on-target toxicities by allowing for dose reduction of the constituent agents.
Rationale for Combination Therapies
Resistance to single-agent BH3-mimetics is not random but evolves through predictable biological adaptations. A primary mechanism is the compensatory upregulation of alternative anti-apoptotic BCL-2 family members not targeted by the drug. For instance, cancer cells treated with the BCL-2/BCL-xL inhibitor navitoclax frequently demonstrate elevated MCL-1 levels, which sustains the sequestration of pro-apoptotic proteins and maintains cell survival [63]. This biological redundancy within the pro-survival network means that inhibiting a single protein often provides a selective pressure for tumors to become dependent on another.
The conceptual basis for synergistic combinations, therefore, lies in preemptively targeting these escape pathways. The logic can be summarized in two key approaches:
- Vertical Inhibition of the Apoptotic Pathway: Simultaneously targeting multiple anti-apoptotic proteins (e.g., BCL-2 and MCL-1) to create a "death signal" that is overwhelming and impossible to compensate for via a single resistance mechanism.
- Horizontal Combination with Pathway Inducers: Combining a BH3-mimetic with agents that potently induce the expression of pro-apoptotic BH3-only proteins (e.g., BIM). This increases the cellular burden of pro-death signals, thereby sensitizing the cell to the displacement effect of the BH3-mimetic [64].
The synergy in such combinations is often quantified using the Combination Index (CI) method, where a CI < 1 indicates synergy. For example, in glioblastoma models, the combination of a low-dose repurposed drug regimen (CUSP9-LD) with the BCL-2/BCL-xL inhibitor navitoclax (ABT-263) resulted in a significant synergistic anti-proliferative effect (CI < 1 across multiple cell lines) [63]. The molecular basis for this synergy was the downregulation of MCL-1 by CUSP9-LD, which circumvented a key resistance mechanism to navitoclax [63].
Promising Synergistic Strategy: BCL-2/BCL-xL Inhibition with MCL-1 Downregulation
Experimental Evidence and Workflow
A compelling strategy to enhance efficacy and reduce resistance involves combining BCL-2/BCL-xL inhibitors with agents that suppress MCL-1 expression or function. This approach was systematically validated in a study on glioblastoma (GBM) [63]. The researchers combined a low-dose version of the CUSP9 repurposed drug regimen (CUSP9-LD) with the BH3-mimetic ABT-263 (Navitoclax). The CUSP9 cocktail, which includes drugs like aprepitant, minocycline, and disulfiram, was found to counteract the ABT-263-mediated up-regulation of MCL-1. This molecular intervention was crucial for achieving synergistic cell death, as confirmed by subsequent MCL-1 siRNA knockdown experiments, which phenocopied the combination's effect and enhanced ABT-263-mediated apoptosis [63].
The following diagram outlines the key experimental workflow and molecular events in this synergistic combination:
Research Reagent Solutions
The experimental validation of this synergistic strategy relied on a specific toolkit of reagents and assays, which are detailed in the table below. This serves as a resource for researchers aiming to replicate or build upon these findings.
Table 2: Essential Research Reagents for Investigating BCL-2/xL and MCL-1 Synergy
| Reagent / Assay | Specific Example | Function in the Experimental Workflow |
|---|---|---|
| BH3-mimetic Inhibitor | ABT-263 (Navitoclax) | Dual-pharmacologic inhibitor of BCL-2 and BCL-xL to displace pro-apoptotic proteins [63]. |
| MCL-1 Modulating Agent | CUSP9-LD cocktail or MCL-1 siRNA | Counteracts resistance by downregulating or knocking down the alternative pro-survival protein MCL-1 [63]. |
| Cell Viability Assay | MTT (3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyltetrazolium bromide) | Measures cellular proliferation and metabolic activity to quantify anti-proliferative effects [63]. |
| Apoptosis Detection | Annexin V / Propidium Iodide (PI) staining with flow cytometry | Distinguishes between live (Annexin V-/PI-), early apoptotic (Annexin V+/PI-), and late apoptotic/necrotic (Annexin V+/PI+) cells [63]. |
| Mitochondrial Assay | Tetramethylrhodamine, Ethyl Ester (TMRE) staining | Assesses the loss of mitochondrial membrane potential (ΔΨm), an early event in mitochondrial apoptosis [63]. |
| Protein Analysis | Western Blotting | Confirms target protein expression and knockdown efficiency (e.g., MCL-1, BCL-2, BCL-xL) and detects cleavage of caspase substrates [63]. |
Detailed Experimental Protocol: Evaluating Synergy In Vitro
This section provides a detailed methodology for assessing the synergistic effects of a BCL-2/BCL-xL inhibitor (e.g., ABT-263) with an MCL-1 downregulating agent (e.g., CUSP9-LD or specific MCL-1 inhibitor) in glioblastoma or other cancer cell lines, based on the cited research [63].
Cell Culture and Preparation
- Cell Lines: Use established glioblastoma lines (e.g., U87MG, A172, T98G) and, critically, primary patient-derived cultured cells (e.g., ULM-GBM-PC35) and stem-like glioma cells (e.g., ULM-GBM-SC35) to better model tumor heterogeneity and therapeutic resistance [63].
- Culture Conditions: Maintain cells in their recommended medium. For experiments, seed cells and then switch to low-serum conditions (e.g., 1.5% FBS) 24 hours prior to treatment to mimic the nutrient-deprived tumor microenvironment and increase dependence on anti-apoptotic proteins [63].
Treatment and Viability Assessment
- Treatment Groups: Include the following conditions: Vehicle (DMSO) control, ABT-263 alone, MCL-1 targeting agent alone, and the combination of ABT-263 + MCL-1 targeting agent.
- Dose-Response Matrix: To calculate a Combination Index (CI), set up a matrix of at least 3-4 different concentrations of each drug alone and in combination.
- Viability Assay (MTT):
- Seed cells in 96-well plates at a density determined by optimal growth curve (e.g., 3-5 x 10³ cells/well).
- After 24 hours, treat cells according to the planned matrix for 72-96 hours.
- Add MTT reagent (0.5 mg/mL final concentration) and incubate for 2-4 hours at 37°C.
- Carefully remove the medium and dissolve the resulting formazan crystals in DMSO.
- Measure the absorbance at 570 nm, with a reference wavelength of 630-650 nm, using a plate reader.
- Calculate the percentage of cell viability relative to the vehicle control. Use software like CompuSyn to analyze the dose-effect relationships and determine the CI, where CI < 1 indicates synergy, CI = 1 additivity, and CI > 1 antagonism [63].
Apoptosis and Mitochondrial Analysis
Annexin V/PI Staining & Flow Cytometry:
- Seed cells in 12-well plates (e.g., 3 x 10⁴ cells/well), treat for 24-48 hours.
- Collect supernatant and trypsinized cells, then centrifuge.
- Wash cell pellets with cold Annexin V binding buffer.
- Resuspend cells in 100 µL of binding buffer containing Annexin V-FITC (e.g., 1:100 dilution) and incubate for 15 minutes in the dark.
- Add PI (e.g., 1 µg/mL) to the cell suspension and analyze immediately using a flow cytometer. A minimum of 10,000 events per sample should be acquired. Analyze the data to quantify the percentage of cells in early and late apoptosis [63].
Mitochondrial Membrane Potential (TMRE Staining):
- Culture and treat cells as for apoptosis assay.
- Load cells with TMRE (e.g., 100-200 nM) for 15-30 minutes at 37°C.
- Wash cells with PBS and analyze fluorescence by flow cytometry (excitation/emission ~549/575 nm). A decrease in TMRE fluorescence indicates a loss of mitochondrial membrane potential, a hallmark of early apoptosis [63].
Molecular Validation by Western Blotting
- Protein Extraction and Quantification: Lyse cells in RIPA buffer supplemented with protease and phosphatase inhibitors. Centrifuge to remove debris and quantify protein concentration using a BCA or Bradford assay.
- Immunoblotting:
- Separate equal amounts of protein (20-40 µg) by SDS-PAGE and transfer to a PVDF membrane.
- Block the membrane with 5% non-fat milk in TBST for 1 hour.
- Incubate with primary antibodies overnight at 4°C. Key antibodies include: Anti-MCL-1, Anti-BCL-2, Anti-BCL-xL, Anti-BIM, Cleaved Caspase-3, and a loading control (e.g., β-Actin or GAPDH).
- Incubate with an appropriate HRP-conjugated secondary antibody for 1 hour at room temperature.
- Detect bands using enhanced chemiluminescence (ECL) substrate and image with a digital system. The expected result confirming the mechanism is a downregulation of MCL-1 protein in the combination group, alongside increased levels of cleaved Caspase-3 [63].
The strategic combination of BCL-2/BCL-xL inhibitors with agents that target resistance mechanisms, such as MCL-1 upregulation, represents a powerful and rational approach to enhance therapeutic efficacy. The preclinical success of combining ABT-263 with the MCL-1-downregulating CUSP9-LD regimen in glioblastoma provides a compelling blueprint for this strategy, demonstrating synergistic cell death and allowing for significant dose reduction of the constituent drugs to mitigate potential toxicity [63].
Future research directions should focus on several key areas:
- Translational Clinical Trials: The promising in vitro data mandates validation in well-designed clinical trials that incorporate robust biomarker analyses to identify patient populations most likely to benefit.
- Novel Combination Partners: Exploring BH3-mimetics in combination with other therapeutic modalities, such as epigenetic modifiers, immunotherapies, and targeted agents against dysregulated metabolic pathways, holds significant potential to overcome diverse resistance landscapes [62].
- Tissue-Specific Dynamics: Further investigation is needed to elucidate the tissue-specific functions of BCL-2 family members and their interactions with non-coding RNAs, which could unveil new layers of regulatory complexity and novel therapeutic nodes [61].
By moving beyond single-agent targeting and embracing rational, mechanism-based combination therapies, the field can more effectively harness the power of apoptotic induction to achieve deeper and more durable responses for cancer patients.
The B-cell lymphoma-2 (Bcl-2) family of proteins serves as the fundamental regulator of the intrinsic apoptotic pathway, functioning as a critical determinant of cellular life and death decisions. Within this protein family, Bcl-2 and Bcl-xL represent the predominant anti-apoptotic members that promote cell survival by preventing programmed cell death [65]. Their overexpression constitutes a fundamental mechanism of carcinogenesis across numerous hematological malignancies and solid tumors, enabling cancer cells to resist endogenous apoptotic signals and therapeutic interventions [66] [16]. The discovery and validation of biomarkers that predict patient response to therapies targeting these proteins have emerged as crucial components in the pursuit of personalized cancer treatment, addressing the significant heterogeneity in treatment responses observed in clinical practice.
Bcl-2 and Bcl-xL exert their anti-apoptotic function primarily at the mitochondrial outer membrane, where they prevent the release of cytochrome c and other pro-apoptotic factors [54]. These proteins achieve this by sequestering pro-apoptotic Bcl-2 family members, including BH3-only proteins and the effector proteins Bax and Bak, thereby maintaining mitochondrial membrane integrity and blocking the activation of the caspase cascade [66] [65]. The structural basis for this function lies in their conserved Bcl-2 homology (BH) domains, which form a hydrophobic groove that serves as a receptor for the BH3 domains of pro-apoptotic proteins [65]. Understanding this molecular interplay provides the foundation for developing predictive biomarkers for targeted therapies.
Biomarker Classes for Predicting Therapeutic Response
Expression-Based Biomarkers
Quantitative assessment of Bcl-2 family protein expression provides fundamental predictive information for response to BH3-mimetic therapies. Research has demonstrated that the relative expression levels of anti-apoptotic Bcl-2 family members, particularly the ratio of Bcl-2 to Bcl-xL and Mcl-1, strongly correlate with sensitivity to specific inhibitors [67].
Table 1: Expression-Based Biomarkers for Predicting Response to Bcl-2/Bcl-xL Targeted Therapies
| Biomarker | Detection Method | Predictive Value | Cancer Context | Reference |
|---|---|---|---|---|
| High BCL-2 Expression | IHC, Gene Expression Profiling | Predicts response to venetoclax | CLL, AML, FL, DLBCL | [66] |
| BCL-2/BCL-xL Ratio | RNA Sequencing, Western Blot | High ratio predicts venetoclax sensitivity | Multiple Myeloma | [67] |
| BCL-2/MCL-1 Ratio | Multiplex IHC, Flow Cytometry | Low ratio confers resistance | AML, Lymphoma | [66] |
| High BCL-xL Expression | IHC, Gene Expression | Predicts resistance to venetoclax; poor prognosis | Colon Cancer (BRAF-mutant) | [68] |
In multiple myeloma models, the expression profile of BCL-2, BCL-XL, and MCL-1 effectively predicts pharmacological response to the BCL-2 selective antagonist venetoclax [67]. Cell lines expressing high BCL-2 with low BCL-XL or MCL-1 demonstrate superior sensitivity to venetoclax, while those co-expressing BCL-2 and BCL-XL remain resistant but respond to BCL-XL-selective inhibition [67]. This expression-based stratification has profound clinical implications, as immunohistochemistry of multiple myeloma patient bone marrow biopsies and aspirates revealed high levels of BCL-2 and BCL-XL in 62% and 43% of evaluable samples, respectively, while 34% were characterized as BCL-2High/BCL-XLLow – a profile associated with superior venetoclax response [67].
Genetic and Genomic Biomarkers
Specific genetic alterations serve as powerful biomarkers for predicting response to Bcl-2 targeted therapies. The t(14;18) chromosomal translocation, which places the BCL-2 gene under the control of the immunoglobulin heavy chain enhancer, occurs in approximately 90% of follicular lymphomas and 30% of diffuse large B-cell lymphomas, leading to BCL-2 overexpression and conferring particular sensitivity to Bcl-2 inhibition [65] [66]. In Waldenström macroglobulinemia, the MYD88 L265P mutation represents a key genomic alteration that intersects with Bcl-2 dependence, while CXCR4 mutations may influence therapeutic response [69].
The presence of specific molecular subtypes within cancer types further refines biomarker prediction. In colon cancer, high Bcl-xL expression specifically identifies a poor prognostic subgroup among BRAF-mutant tumors [68]. Bioinformatics analysis of gene expression data from stage II/III colon cancer patients revealed that high Bcl-xL gene expression levels associated with increased risk of relapse specifically in BRAF-mutant tumors (HR = 8.3, 95% CI 1.7–41.7), but not in KRAS-mutant or double wild-type tumors [68]. This finding was validated at the protein level, where high Bcl-xL protein expression in BRAF-mutant, untreated, stage II/III colon cancer associated with significantly increased risk of death (HR = 12.13, 95% CI 2.49–59.13) [68].
Functional Biomarkers
Functional assays that measure apoptotic priming offer a dynamic approach to biomarker assessment. BH3 profiling represents a particularly powerful functional biomarker technique that measures mitochondrial sensitivity to BH3 domain peptides, effectively quantifying how close a cell is to the apoptotic threshold [16]. This method can identify "primed" cells that are highly dependent on specific anti-apoptotic proteins and therefore likely to respond to corresponding targeted therapies.
Table 2: Functional and Dynamic Biomarkers in Bcl-2 Family Targeted Therapy
| Biomarker Category | Specific Assay/Method | Measured Parameter | Clinical Utility |
|---|---|---|---|
| Functional Capacity | BH3 Profiling | Mitochondrial depolarization in response to specific BH3 peptides | Measures apoptotic priming and BCL-2 dependence |
| Dynamic Response | Flow Cytometry with Annexin V/PI | Early apoptotic cells post-treatment | Assesses initial therapeutic efficacy |
| Protein Interactions | Co-immunoprecipitation | BCL-2/Beclin-1 or BCL-2/BIM complexes | Evaluates autophagy-apoptosis balance |
| Post-Translational Modifications | Phospho-specific Western Blot | BCL-2 phosphorylation status (e.g., Ser70) | Indicates activation state and drug susceptibility |
Post-translational modifications of Bcl-2 family members also serve as functional biomarkers. Phosphorylation of Bcl-2 at serine 70 disrupts its interaction with Beclin-1, enabling autophagy initiation and influencing cellular response to stress [61]. Additionally, caspase-mediated cleavage of Bcl-2 during apoptosis converts it from an anti-apoptotic to a pro-apoptotic protein, creating a biomarker for apoptotic commitment [61]. Assessment of these modifications provides insight into the functional state of Bcl-2 family proteins beyond mere expression levels.
Experimental Methodologies for Biomarker Discovery and Validation
Transcriptomic Profiling and Bioinformatics Analysis
Transcriptomic approaches provide comprehensive data for biomarker discovery through analysis of gene expression patterns associated with treatment response. The standard workflow begins with RNA extraction from patient samples or cell lines, followed by quality control using methods such as the Bioanalyzer to ensure RNA integrity numbers (RIN) >8.0 [68]. Library preparation utilizes stranded mRNA-seq protocols with poly-A selection, and sequencing performs on platforms such as Illumina to a depth of 30-50 million reads per sample. Bioinformatics processing includes adapter trimming, alignment to the reference genome (e.g., GRCh38) using STAR aligner, and gene-level quantification with tools such as featureCounts [68].
Differential expression analysis between responder and non-responder groups employs statistical packages such as DESeq2 or limma-voom, with multiple testing correction using the Benjamini-Hochberg procedure. For the identification of Bcl-2 family-specific signatures, focused analysis on apoptosis-related gene sets from databases such as MSigDB provides enhanced sensitivity. Supervised classification algorithms, including random forests and support vector machines, build predictive models from transcriptomic data, as demonstrated in studies that identified Bcl-xL as a predictor of relapse risk specifically in BRAF-mutant colon cancer [68]. Validation in independent cohorts remains essential, with techniques such as quantitative RT-PCR or Nanostring assays enabling cost-effective confirmation of candidate biomarkers.
Protein-Level Assessment Techniques
Immunohistochemistry (IHC) represents the gold standard for protein biomarker validation in clinical samples, providing spatial context within tissue architecture. For Bcl-2 and Bcl-xL assessment, formalin-fixed paraffin-embedded (FFPE) tissue sections undergo antigen retrieval using citrate or EDTA-based buffers at high temperature [68]. Primary antibodies against Bcl-2 (clone 124) and Bcl-xL (clone 54H6) provide specific detection, with appropriate isotype controls establishing assay specificity. Semiquantitative scoring systems (e.g., H-scores) incorporate both staining intensity and percentage of positive cells, while digital pathology platforms enable more objective quantification [68].
Flow cytometry offers a complementary approach for hematological malignancies, allowing simultaneous assessment of multiple Bcl-2 family proteins in specific cell populations. Intracellular staining protocols require cell permeabilization with saponin-based buffers after surface marker staining. Fluorescent-conjugated antibodies against Bcl-2, Bcl-xL, and Mcl-1 enable multiplexed analysis, with compensation controls ensuring spectral unmixing accuracy. For functional assessment, BH3 peptide profiling platforms utilize flow cytometric measurement of mitochondrial membrane potential (using dyes such as JC-1 or TMRE) in response to specific BH3 domain peptides, providing a dynamic measure of apoptotic priming [16].
Genetic Alteration Detection Methods
Next-generation sequencing (NGS) panels represent the standard approach for detecting genetic biomarkers predictive of response to Bcl-2 targeted therapies. DNA extraction from tumor samples with matched normal tissue enables identification of somatic alterations. Hybrid capture-based libraries enriched for genes of interest (including BCL2, MYD88, CXCR4, BRAF, and other apoptosis regulators) undergo sequencing to high coverage (>500x) to ensure sensitivity for subclonal mutations [69]. Variant calling pipelines such as GATK Best Practices identify single nucleotide variants and small insertions/deletions, while manual review in integrative genomics viewers (IGV) confirms high-confidence mutations.
For structural variants such as the t(14;18) translocation, droplet digital PCR (ddPCR) provides highly sensitive detection with absolute quantification. This approach enables monitoring of minimal residual disease in lymphoma patients undergoing Bcl-2 targeted therapy [66]. Fluorescence in situ hybridization (FISH) serves as an alternative method for translocation detection, particularly in formalin-fixed tissues, providing visual confirmation of chromosomal rearrangements within intact nuclei.
Bcl-2 Family Regulation and Signaling Pathways
The Bcl-2 protein family constitutes a critical regulatory network that controls the mitochondrial apoptotic pathway through complex interactions between pro-survival and pro-apoptotic members [61] [65]. The anti-apoptotic proteins, including Bcl-2, Bcl-xL, Mcl-1, Bcl-w, and A1/BFL-1, preserve mitochondrial outer membrane integrity by sequestering pro-apoptotic activators and preventing Bax/Bak activation [66]. The pro-apoptotic proteins divide into two classes: the multi-domain effectors Bax and Bak, which directly mediate mitochondrial outer membrane permeabilization (MOMP), and the BH3-only proteins (Bim, Bid, Puma, Bad, Noxa, etc.), which initiate apoptotic signaling by neutralizing anti-apoptotic family members or directly activating Bax/Bak [65] [16].
Figure 1: Bcl-2 Family Regulation of Mitochondrial Apoptosis Pathway. This diagram illustrates how cellular stress signals activate BH3-only proteins, which either neutralize anti-apoptotic proteins or directly activate effector proteins Bax/Bak. BH3 mimetic drugs mimic sensitizer BH3-only proteins to promote apoptosis.
The balance between these competing factions determines cellular fate, with their interactions governed by binding specificity between the hydrophobic groove of anti-apoptotic proteins and the BH3 domains of their pro-apoptotic counterparts [65]. Bcl-2 and Bcl-xL display distinct binding profiles: Bcl-2 binds with high affinity to Bim, Bid, and Puma, while Bcl-xL exhibits broader binding capabilities including Bim, Bid, Bmf, and Puma [54]. This differential binding specificity contributes to tissue-specific functions and has profound implications for therapeutic targeting, as the relative expression of different BH3-only proteins influences dependence on specific anti-apoptotic family members.
Research Reagent Solutions for Biomarker Discovery
Table 3: Essential Research Reagents for Bcl-2 Family Biomarker Investigation
| Reagent Category | Specific Examples | Application | Technical Notes |
|---|---|---|---|
| Selective Inhibitors | Venetoclax (ABT-199; BCL-2 selective), A-1331852 (BCL-xL selective), Navitoclax (ABT-263; BCL-2/BCL-xL/BCL-w), Obatoclax (pan-BCL-2 inhibitor) | Functional validation of biomarker candidates, combination studies | Use dose-response curves (1 nM-10 μM) to establish IC50 values; monitor platelet toxicity with BCL-xL inhibitors [16] |
| Validated Antibodies | Anti-BCL-2 (clone 124 for IHC, clone 100 for flow), Anti-BCL-xL (clone 54H6), Anti-MCL-1 (clone D35A5), Anti-BIM (clone C34C5), Phospho-specific BCL-2 (Ser70) | Protein quantification, subcellular localization, post-translational modification detection | Validate for specific applications (IHC, Western, flow); optimize antigen retrieval conditions for FFPE [68] |
| BH3 Domain Peptides | BIM BH3, BAD BH3, MS-1 BH3 (MCL-1 selective), HRK BH3 (BCL-xL selective), NOXA BH3 (MCL-1/A1 selective) | BH3 profiling, mitochondrial functional assays, competitive binding studies | Use high-purity synthetic peptides (>95%); titrate concentrations (0.1-100 μM) to determine priming level [16] |
| Cell Line Models | OCI-Ly1 (BCL-2 dependent lymphoma), OCI-AML2 (MCL-1 dependent leukemia), MOLT-4 (BCL-2/BCL-xL co-dependent), Patient-derived xenografts | Preclinical validation, mechanism studies, combination therapy screening | Characterize baseline BCL-2 family expression; engineer resistant variants via CRISPR to study resistance [67] |
| Apoptosis Detection Kits | Annexin V/Propidium Iodide, Caspase-3/7 activation assays, JC-1 mitochondrial membrane potential, TMRE mitochondrial dye | Functional assessment of therapeutic response, dynamic biomarker development | Establish baseline apoptosis in controls; use time-course measurements (0-48h) to capture kinetics [66] |
The research reagents detailed in Table 3 enable comprehensive investigation of Bcl-2 family biomarkers across experimental systems. Selective pharmacological inhibitors serve not only as therapeutic agents but also as tools for validating biomarker predictions, with their specificity profiles critical for interpreting results [16]. For instance, venetoclax's selective affinity for Bcl-2 makes it ideal for identifying Bcl-2-dependent malignancies, while navitoclax's broader specificity enables targeting of tumors with mixed anti-apoptotic dependencies [3] [16]. Validated antibodies must demonstrate application-specific performance, with particular attention to epitope preservation in archival clinical samples.
BH3 domain peptides represent particularly powerful reagents for functional biomarker assessment. In BH3 profiling, these peptides measure mitochondrial apoptotic priming by testing the ability of specific BH3 sequences to induce cytochrome c release or mitochondrial membrane depolarization [16]. The pattern of response to different BH3 peptides reveals which anti-apoptotic proteins a cell depends on for survival, providing a functional biomarker that complements expression data. MS-1 and HRK BH3 peptides specifically identify Mcl-1 and Bcl-xL dependence, respectively, while BAD BH3 detects dependence on Bcl-2, Bcl-xL, and Bcl-w [16].
Implementation Strategies for Biomarker-Guided Therapy
Successful implementation of biomarker-guided therapy requires integrated diagnostic and therapeutic approaches. For hematological malignancies, assessment of BCL-2 family expression profiles by IHC or flow cytometry at diagnosis enables stratification for targeted therapy [66]. In chronic lymphocytic leukemia, the combination of BCL-2 expression with genetic features such as 17p deletion identifies patients most likely to benefit from venetoclax-containing regimens [66] [16]. For solid tumors, functional assessment using BH3 profiling may provide critical insights beyond expression patterns, particularly in genetically heterogeneous malignancies.
Longitudinal biomarker assessment represents a crucial strategy for managing therapeutic resistance. Mechanisms of resistance to Bcl-2 inhibitors include upregulation of alternative anti-apoptotic proteins (particularly Mcl-1 or Bcl-xL), mutations in BCL-2 that reduce drug binding, and changes in the expression of BH3-only proteins [66]. Sequential monitoring of these potential resistance mechanisms through liquid biopsy approaches or repeat tissue sampling enables adaptive therapy modifications, such as combining Bcl-2 inhibitors with Mcl-1 or Bcl-xL targeting agents upon emergence of resistance [16].
The integration of Bcl-2 family biomarkers with other molecular data creates multidimensional predictive models that enhance treatment personalization. In multiple myeloma, combining BCL-2/BCL-xL/MCL-1 expression ratios with cytogenetic risk stratification and disease stage improves prediction of venetoclax response [67]. Similarly, in colon cancer, the conjunction of BRAF mutation status with Bcl-xL expression identifies patient subgroups with distinct prognostic and therapeutic implications [68]. These integrated approaches acknowledge the complexity of apoptotic regulation and provide frameworks for addressing heterogeneity in treatment response.
Comparative Efficacy and Future Directions in Clinical Targeting
The B-cell lymphoma-2 (BCL-2) family of proteins constitutes the fundamental regulatory network governing the intrinsic apoptotic pathway, a tightly controlled process of programmed cell death crucial for maintaining cellular homeostasis [60] [70]. The delicate balance between pro-survival and pro-apoptotic BCL-2 family members is frequently dysregulated in cancer, tipping the scales in favor of cell survival and enabling tumorigenesis and treatment resistance [70]. Pro-survival members, including BCL-2, BCL-xL, and MCL-1, function as guardians of cell survival by sequestering pro-apoptotic proteins, thereby preventing mitochondrial outer membrane permeabilization (MOMP) and the subsequent activation of the caspase cascade [60] [70]. For decades, BCL-2 has been a promising but elusive target for cancer therapy. The development and subsequent clinical approval of venetoclax, a highly selective BCL-2 inhibitor, validated the therapeutic potential of targeting this pathway and has fundamentally reshaped the treatment landscape for several hematological malignancies [36] [71]. This whitepaper examines the clinical trial data validating the efficacy and safety profiles of BCL-2 inhibitors, framing their development within the broader thesis of targeting the BCL-2/BCL-xL axis to reinstate apoptosis in cancer cells.
Mechanistic Basis of BCL-2 Inhibition
The Intrinsic Apoptotic Pathway and its Regulation
The intrinsic apoptotic pathway is initiated by cellular stress signals, such as DNA damage or oncogene activation. These signals lead to the activation of BH3-only proteins (e.g., BIM, BID, PUMA), which act as cellular sentinels [60] [16]. The core mechanism revolves around the interaction between three classes of BCL-2 family proteins:
- Anti-apoptotic proteins (e.g., BCL-2, BCL-xL, MCL-1): Characterized by multiple BH domains, they preserve mitochondrial integrity by binding and neutralizing pro-apoptotic effectors [70].
- Pro-apoptotic effectors (BAK, BAX): Upon activation, they oligomerize to form pores in the mitochondrial outer membrane in a process known as MOMP [60] [16].
- BH3-only proteins: They promote apoptosis either by directly activating BAX/BAK or by neutralizing anti-apoptotic proteins, thereby displacing bound pro-apoptotic activators [60].
BH3-mimetic drugs, such as venetoclax, are designed to mimic the function of the latter group. By selectively binding with high affinity to the hydrophobic groove of BCL-2, they disrupt its interaction with pro-apoptotic proteins like BIM and BAX. This disinhibition of pro-apoptotic proteins allows for BAX/BAK activation, culminating in MOMP, cytochrome c release, and irreversible commitment to cell death via caspase activation [60] [36] [16]. The following diagram illustrates this core signaling pathway and the site of action for BH3-mimetics.
Selectivity and the Challenge of BCL-xL Inhibition
A critical advancement in the field was achieving selective BCL-2 inhibition. Early inhibitors like navitoclax targeted both BCL-2 and BCL-xL. While clinically effective, BCL-xL inhibition led to on-target thrombocytopenia due to the dependence of platelets on BCL-xL for survival, thus dose-limiting its utility [36] [16]. Venetoclax was specifically engineered to exploit subtle structural differences in the binding grooves of BCL-2 and BCL-xL, granting it high selectivity for BCL-2 and a dramatically improved hematological safety profile [16]. Computational and structural studies have since elucidated that residues like SER106 and LEU108 in BCL-XL and ASP103 in BCL-2 are critical determinants for this inhibitory selectivity [72]. This selectivity is a cornerstone of its clinical safety and efficacy.
Clinical Trial Validation of Efficacy
Extensive clinical trials have established the profound efficacy of BCL-2 inhibitors, primarily venetoclax, in various hematologic malignancies. The data below summarize key efficacy outcomes from clinical trials of BCL-2 inhibitors, particularly in relapsed/refractory (R/R) and frontline settings.
Table 1: Efficacy Outcomes of BCL-2 Inhibitors in Hematologic Malignancies
| Cancer Type | Regimen | Trial Phase | Patient Population | Key Efficacy Outcome | Citation |
|---|---|---|---|---|---|
| CLL/SLL | Venetoclax + Rituximab | Phase 3 | R/R CLL | Significantly improved overall response rate (ORR) and progression-free survival (PFS) vs. standard chemoimmunotherapy | [71] |
| CLL/SLL | Venetoclax + Obinutuzumab | Phase 3 | Frontline CLL | Superior PFS compared to chlorambucil + obinutuzumab | [71] |
| CLL/SLL | Lisaftoclax (APG-2575) monotherapy | Pivotal Phase 2 | R/R CLL/SLL after BTK inhibitor failure | ORR: 62.5% (by IRC); Median PFS: 23.89 months | [73] |
| AML | Venetoclax + Azacitidine | Phase 3 | Newly diagnosed AML (unfit for intensive chemo) | Higher ORR and overall survival vs. azacitidine alone | [36] |
| R/R AML/MPAL | Lisaftoclax + Azacitidine | Phase 1/2 | Relapsed/Refractory (Venetoclax-exposed) | ORR: 29.2% (7/24 patients) | [73] |
The efficacy of BCL-2 inhibitors is not absolute, and resistance can develop. Key mechanisms of resistance identified in clinical and preclinical studies include:
- Upregulation of alternative anti-apoptotic proteins, particularly MCL-1, which is not targeted by venetoclax [74] [16].
- Mutation of the BCL-2 gene itself, which can reduce the binding affinity of venetoclax [36].
- Genetic mutations in other pathways that alter the apoptotic dependency of the cancer cell [36] [16].
The efficacy of BCL-2 inhibitors is profoundly influenced by the cellular context, including the expression levels of other BCL-2 family proteins. This underscores the importance of predictive biomarkers to identify patient populations most likely to respond.
Safety and Tolerability Profiles
The safety profile of BCL-2 inhibitors is characterized by manageable on-target adverse events, with the most significant risk being tumor lysis syndrome (TLS).
Common and Severe Adverse Events
A systematic review and meta-analysis of venetoclax clinical trials found that the most common adverse events (AEs) of monotherapy are gastrointestinal, including nausea and diarrhea, as well as cytopenias such as neutropenia and thrombocytopenia [75]. When venetoclax is combined with other agents, these AEs remain common, but the overall event rate is considered tolerable given the clinical benefit [75]. The most frequent severe (Grade ≥3) AEs are hematological, including neutropenia, thrombocytopenia, anemia, and febrile neutropenia [75]. These are manageable with dose modifications and supportive care, including growth factors.
Tumor Lysis Syndrome and Its Management
TLS is an on-target oncologic emergency caused by the rapid lysis of tumor cells upon initiation of therapy, releasing intracellular contents that can lead to renal failure, cardiac arrhythmias, and seizures. It is a recognized risk, particularly in patients with high tumor burden (e.g., CLL) initiating venetoclax [75] [71]. Modern clinical protocols have successfully mitigated this risk through step-wise dose escalation and rigorous prophylactic measures (hydration, anti-hyperuricemic agents) [71]. Notably, recent next-generation inhibitors like lisaftoclax have reported a manageable safety profile with no TLS events observed in the reported Phase II study, highlighting continued improvements in clinical management and drug design [73].
Table 2: Safety and Tolerability Profile of BCL-2 Inhibitors
| Adverse Event Category | Specific Events | Frequency & Severity | Management Strategies |
|---|---|---|---|
| Hematological | Neutropenia, Thrombocytopenia, Anemia | Common; frequent Grade ≥3 events | Dose interruption/reduction, growth factor support |
| Gastrointestinal | Nausea, Diarrhea | Very common, typically low-grade | Supportive care, anti-emetics |
| Serious Risks | Tumor Lysis Syndrome (TLS), Febrile Neutropenia | High risk in specific populations (high tumor burden) | Step-wise dose ramp-up, hydration, monitoring, hospitalization for initial doses |
Experimental and Clinical Methodologies
The validation of BCL-2 inhibitors rests on a foundation of robust preclinical and clinical experimental frameworks.
Core Experimental Protocols for Preclinical Validation
Key methodologies used to establish the efficacy and mechanism of action of BCL-2 inhibitors in laboratory models include:
- Assessment of Apoptosis: The gold standard is Annexin V/Propidium Iodide (PI) staining followed by flow cytometry. Annexin V binds to phosphatidylserine externalized on the cell surface during early apoptosis, while PI stains DNA in late apoptotic and necrotic cells with compromised membrane integrity [74].
- Analysis of Protein Interactions: Co-immunoprecipitation (Co-IP) and immunoblotting are critical for demonstrating that BH3 mimetics disrupt the physical interaction between BCL-2 and pro-apoptotic proteins like BIM. This confirms the on-target mechanism of drug action [74].
- Analysis of BAX/BAK Activation: Conformational changes in BAX and BAK during activation can be detected using conformation-specific antibodies in flow cytometry or immunoblotting assays [74].
- In Vivo Xenograft Models: Subcutaneous or systemic xenograft models in immunodeficient mice (e.g., NOD/SCID-gamma) are used to evaluate anti-tumor efficacy in vivo. Tumor growth is monitored, and apoptotic activation in tumors can be quantified via immunohistochemistry for cleaved caspases [74].
The following diagram outlines a typical workflow for the preclinical assessment of a BCL-2 inhibitor.
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Research Reagents for BCL-2 Inhibitor Studies
| Reagent / Assay | Primary Function in Research |
|---|---|
| BH3 Mimetics (e.g., ABT-737, Venetoclax) | Tool compounds to selectively inhibit BCL-2 family proteins and probe apoptotic dependencies in cancer models. |
| Annexin V / PI Apoptosis Kit | Standardized kit for the quantitative detection of early and late apoptotic cells by flow cytometry. |
| Conformation-specific BAX/BAK Antibodies | Detect the active, oligomerization-competent forms of these executioner proteins to confirm apoptosis induction. |
| shRNA/siRNA for BCL-2 Family Genes | Genetically knock down expression of specific proteins (e.g., MCL-1, BIM) to validate targets and identify resistance mechanisms. |
| Tet-inducible Knockdown Systems | Allow controlled, inducible gene knockdown in vitro and in vivo to study temporal effects of target loss. |
The clinical success of venetoclax has firmly established BCL-2 inhibition as a pillar of modern cancer therapy, particularly in hematologic malignancies. Future strategies are focused on overcoming resistance and expanding the utility of these agents.
- Next-Generation Inhibitors: Drugs like lisaftoclax (APG-2575) and eiletoclax are being developed with the goal of improved safety profiles (e.g., reduced TLS risk) and efficacy in venetoclax-resistant settings [76] [73].
- Rational Combination Therapies: Preclinical and clinical data strongly support combining BCL-2 inhibitors with other targeted agents. For instance, dual inhibition of the PI3K/AKT/mTOR pathway and BCL-2/BCL-xL has demonstrated striking synergy in AML models. PI3K/mTOR inhibitors downregulate MCL-1 and release BIM from BCL-2/BCL-xL, thereby "priming" cells for enhanced killing by BH3 mimetics [74] [16].
- Expansion into Solid Tumors: While the primary successes are in blood cancers, ongoing research is evaluating BCL-2 inhibitors in solid tumors, often in combination with other agents, with promising results in preclinical models [36] [16].
In conclusion, the clinical trial validation of BCL-2 inhibitors represents a triumph of translational research, from understanding the atomic-level structure of protein-drug interactions to demonstrating prolonged survival in patients. The ongoing development of next-generation inhibitors and sophisticated combination regimens, guided by a deeper understanding of apoptotic biology and resistance mechanisms, promises to further exploit the BCL-2/BCL-xL axis for cancer therapy.
The B-cell lymphoma 2 (BCL-2) protein family represents the fundamental regulatory switch controlling the intrinsic (mitochondrial) apoptotic pathway. The discovery of BCL-2 in 1984 as the gene involved in the t(14;18) chromosomal translocation in follicular lymphoma marked the identification of the first oncogene that promotes cancer cell survival by inhibiting programmed cell death rather than stimulating proliferation [77]. This foundational discovery launched three decades of research into the BCL-2 protein family, which has culminated in the development of specific inhibitors that are now in clinical use, saving and improving tens of thousands of lives annually [77]. The BCL-2 family comprises both pro-survival and pro-apoptotic members that interact through a complex network to determine cellular fate. The anti-apoptotic proteins, including BCL-2, BCL-XL, and MCL1, function as critical guardians of mitochondrial integrity by preventing the activation of the executioner proteins BAX and BAK. When activated, BAX and BAK oligomerize to permeabilize the mitochondrial outer membrane, leading to the release of cytochrome c and other apoptogenic factors that activate the caspase cascade and execute cellular destruction [2] [66]. Cancer cells frequently exploit this survival mechanism by overexpressing anti-apoptotic BCL-2 family proteins to resist endogenous apoptotic signals and therapeutic insults, making these proteins attractive targets for cancer therapy.
Comparative Molecular and Functional Characteristics
The anti-apoptotic BCL-2 family proteins share structural similarities but play distinct non-redundant roles in cellular homeostasis and tumorigenesis. These globular α-helical proteins share extensive sequence and structural similarity, containing four BCL-2 homology (BH) domains. A defining characteristic is an eight-helix bundle (encoded within the BH1, 2 and 3 domains) that forms a hydrophobic surface groove for binding BH3 domains of pro-apoptotic family members [2]. All anti-apoptotic members integrate into the outer mitochondrial membrane via a C-terminal transmembrane domain, where they execute their canonical function of preventing mitochondrial outer membrane permeabilization (MOMP) [2]. Beyond their mitochondrial localization, these proteins also reside at the endoplasmic reticulum (ER), where they contribute to the regulation of intracellular Ca2+ signaling, adding another layer to their anti-apoptotic function [2].
Table 1: Fundamental Characteristics of Anti-Apoptotic BCL-2 Family Proteins
| Feature | BCL-2 | BCL-XL | MCL1 |
|---|---|---|---|
| Chromosomal Location | 18q21.3 | 20q11.21 | 1q21 |
| Protein Size | 239 amino acids (BCL-2α) | 233 amino acids | 350 amino acids |
| Primary Physiological Functions | Lymphocyte survival, neuronal maintenance, epithelial homeostasis | Embryonic development, platelet survival, neuronal survival | Embryonic development, lymphocyte survival, maintenance of stem cells |
| Expression Pattern | Long-lived cells (memory B lymphocytes, neuronal cells) | Widely expressed, high during development | Broad expression, short-lived cells, rapidly inducible |
| Non-Apoptotic Functions | Cell cycle regulation, mitochondrial dynamics, calcium signaling | Platelet activation, neuronal synaptic plasticity, mitochondrial metabolism | Mitochondrial physiology, protein folding, autophagy regulation |
| Regulatory Mechanisms | Transcriptional control, post-translational modifications, proteasomal degradation | Transcriptional regulation, alternative splicing, phosphorylation | Rapid turnover, transcriptional induction, phosphorylation, ubiquitination |
Despite their shared anti-apoptotic function, these proteins display significant differences in their regulation and non-canonical functions. BCL-2 demonstrates particularly high expression in long-lived cell populations such as memory B lymphocytes and neuronal cells [77]. BCL-XL is essential for embryonic development and plays specialized roles in platelet and neuronal survival [2]. MCL1 stands apart through its rapid turnover rate, transcriptional inducibility, and broader roles in mitochondrial physiology and autophagy regulation [78]. The distinct characteristics of each protein ultimately dictate their specific roles in development, tissue homeostasis, and cancer pathogenesis, which in turn influences their potential as therapeutic targets.
Expression Profiles Across Malignancies and Therapeutic Implications
The expression patterns of BCL-2, BCL-XL, and MCL1 vary significantly across cancer types, with important implications for therapeutic targeting and resistance mechanisms. In B-cell malignancies, BCL-2 is frequently overexpressed due to the t(14;18) translocation in follicular lymphoma (80-90% of cases) and approximately one-third of diffuse large B-cell lymphomas (DLBCL) [66] [77]. Chronic lymphocytic leukemia (CLL) cells overexpress BCL-2 due to BCL-2 gene hypomethylation, loss of miR-15 and miR-16 at 13q14, and STAT3 transcription factor activation [66]. Analysis of mature B-cell malignancies reveals that anti-apoptotic genes are generally upregulated while pro-apoptotic genes are downregulated compared to normal counterpart cells [79].
In solid tumors, distinct patterns emerge. In breast cancer, investigation of anti-apoptotic BCL-2 family members across three major molecular subtypes (Luminal, HER2-enriched, and Basal-like) revealed greater expression and more frequent gene amplification of MCL1 compared to BCL2 or BCL2L1 (BCL-XL) [78]. MCL1 protein expression was elevated in both estrogen receptor α (ERα)-positive and ERα-negative tumors compared to normal breast tissue, with particularly high staining in ERα+ tumors [78]. In small-cell lung cancer (SCLC), immunohistochemistry of tissue microarrays from surgically resected patients demonstrated that high MCL1 expression with low BCL-XL and BCL-2 represents the most common expression profile [80].
Table 2: Expression Patterns and Genetic Alterations in Human Cancers
| Cancer Type | BCL-2 | BCL-XL | MCL1 | Therapeutic Implications |
|---|---|---|---|---|
| Follicular Lymphoma | Translocation t(14;18) in 80-90% | Variable expression | Variable expression | BCL-2 inhibition highly effective |
| CLL | Overexpression (hypomethylation, miR-15/16 loss) | Moderate expression | Moderate expression | BCL-2 inhibition highly effective |
| DLBCL | Translocation in ~30% | Moderate to high expression | Moderate to high expression | Variable response to BCL-2 inhibition |
| Multiple Myeloma | Low to moderate expression | High in stromal-protected cells | High, upregulated by stroma | Dual MCL-1/BCL-XL inhibition may be needed |
| Breast Cancer | Expressed in up to 70% of ERα+ cases | Increased in DCIS vs. normal breast | Most frequent amplification and expression | MCL1 dependency predominant |
| Small-Cell Lung Cancer | Low expression in majority | Low expression in subset | High expression in majority | MCL1 inhibition effective in low BCL-XL contexts |
| Acute Myeloid Leukemia | Variable expression | Moderate expression | Frequently upregulated | Venetoclax effective, MCL1 upregulation in resistance |
The cooperative relationships between these anti-apoptotic proteins significantly influence therapeutic responses. In multiple myeloma, stromal interactions upregulate MCL-1 expression and increase dependency on BCL-XL, creating a cooperative protection system where inhibiting one protein leads to enhanced binding of the other to pro-apoptotic BIM [81]. Similarly, in breast cancer cells, combined blockade of BCL-2 and BCL-XL only transiently induces apoptosis, as cells rapidly acclimate through MCL-1 upregulation and enhanced MCL-1 activity [78]. These observations highlight the complex compensatory mechanisms within the BCL-2 protein network that cancer cells exploit to evade targeted therapies.
Therapeutic Targeting: Clinical Applications and Limitations
The development of BH3-mimetics, small molecules that selectively inhibit anti-apoptotic BCL-2 family members by binding to their hydrophobic BH3-binding grooves, represents a landmark achievement in targeted cancer therapy. The first breakthrough came with venetoclax (ABT-199), a highly selective BCL-2 inhibitor that received FDA approval in 2016 for the treatment of CLL and has since transformed the treatment landscape for hematologic malignancies [2] [66]. Venetoclax demonstrates remarkable efficacy in CLL, where it displaces pro-apoptotic BIM from BCL-2 to activate BAX/BAK-mediated apoptosis [66]. Its success has led to the development of chemically similar BCL-2 inhibitors such as sonrotoclax and lisaftoclax, currently under clinical evaluation [2].
However, the development of BH3-mimetics targeting BCL-XL or MCL1 has proven more challenging. BCL-XL inhibition causes rapid and profound thrombocytopenia due to BCL-XL's essential role in platelet survival, limiting its therapeutic window [2]. MCL1 inhibitors have been associated with cardiac toxicities and other on-target adverse events, precluding the clinical development of some candidates [2]. Tumor-specific BCL-XL or MCL1 inhibition may be achievable through novel approaches using proteolysis targeting chimeras (PROTACs) or selective drug delivery strategies, which could potentially expand the therapeutic window [2].
Table 3: Clinically Advanced BH3-Mimetics and Their Properties
| Agent | Target Specificity | Clinical Status | Key Indications | Dose-Limiting Toxicities |
|---|---|---|---|---|
| Venetoclax (ABT-199) | Selective BCL-2 inhibitor | FDA-approved (2016) | CLL, AML | Tumor lysis syndrome, myelosuppression |
| Navitoclax (ABT-263) | BCL-2, BCL-XL, BCL-w | Early-phase clinical trials | Hematological malignancies | Thrombocytopenia (BCL-XL-mediated) |
| S63845 | MCL1 inhibitor | Preclinical/early development | SCLC, multiple myeloma | Cardiac toxicity concerns |
| AZD5991 | MCL1 inhibitor | Early-phase trials | Multiple myeloma, AML | Cardiac events |
| A-1331852 | BCL-XL inhibitor | Preclinical development | Solid tumors, stromal-protected malignancies | Thrombocytopenia |
| Lisaftoclax (APG-2575) | BCL-2 selective | Clinical trials | CLL, other hematologic malignancies | Well-tolerated, neutropenia |
The expression levels of anti-apoptotic BCL-2 family proteins serve as important predictors of response to BH3-mimetics. In luminal breast cancer cells, MCL1 gene expression levels correlate inversely with sensitivity to pharmacological BCL-2/BCL-XL inhibition, whereas no relationship was seen between gene expression of BCL2 or BCL2L1 and sensitivity to BCL-2/BCL-XL inhibition [78]. In SCLC, MCL1 inhibition using S63845 is effective specifically in cell lines with high MCL1 and low BCL-XL expression profiles [80]. Furthermore, the ratio (BCL2+BCL2L11+BAX)/BCL2L1 has been identified as the strongest predictor of venetoclax response for mature B-cell malignancies in vivo [79]. These findings highlight the importance of comprehensive biomarker development for patient selection and treatment optimization.
Experimental Models and Methodologies for Investigating BCL-2 Family Proteins
In Vitro Cytotoxicity and Apoptosis Assays
Standardized methodologies have been developed to assess the efficacy and mechanisms of action of BCL-2 family inhibitors. For cytotoxicity assays, cells are typically seeded in 96-well plates and treated with varying concentrations of BH3-mimetics. Cell viability is measured using assays such as Caspase-Glo 3/7, which quantifies caspase activation through luminescence readouts normalized to protein content [78] [81]. Apoptosis is specifically assessed by Annexin V/propidium iodide staining followed by flow cytometry, allowing for quantification of early and late apoptotic populations [81]. For modeling stromal protection effects, co-culture systems with stromal cell lines (e.g., HS5 stromal cells) are employed, with careful separation techniques to analyze tumor cells specifically after treatment [81].
Protein-Protein Interaction Studies
Understanding the interactions between anti-apoptotic and pro-apoptotic proteins is essential for elucidating mechanisms of action and resistance. Proximity ligation assays (PLA) enable in situ detection and quantification of protein interactions, such as between MCL-1 and BIM [78]. The Duolink protocol involves fixing cells, incubating with primary antibodies against the proteins of interest, followed by species-specific secondary antibodies conjugated with oligonucleotides that form amplifiable circular DNA when in close proximity (<40nm) [78]. Immunoprecipitation studies provide complementary information, typically involving cell lysis in IP-specific buffer, incubation with target antibody (e.g., BIM), followed by protein G agarose beads to pull down complexes, which are then analyzed by western blotting to identify interaction partners [81].
Gene Expression Analysis and Dependency Mapping
Gene expression profiling of BCL-2 family members is performed using RNA extraction followed by reverse transcription and quantitative PCR with gene-specific primers, analyzed via the delta-delta Ct method [81]. Large-scale dependency mapping using resources such as the Cancer Cell Line Encyclopedia (CCLE) and drug sensitivity databases (e.g., CancerRxGene) enables correlation of basal gene expression with drug response patterns across hundreds of cell lines [78]. For genetic dependency studies, CRISPR/Cas9 systems are employed to generate knockout cells, such as BAX/BAK double knockout lines, to confirm the specific involvement of the mitochondrial apoptotic pathway in compound activity [81].
Signaling Pathways and Experimental Workflows
Diagram 1: BCL-2 Family Regulation of Mitochondrial Apoptosis and BH3-Mimetic Mechanism of Action. This diagram illustrates how anti-apoptotic BCL-2 proteins maintain mitochondrial integrity by sequestering pro-apoptotic activators and effectors. BH3-mimetics displace these interactions, permitting BAX/BAK activation and apoptosis.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Investigating BCL-2 Family Proteins
| Reagent/Category | Specific Examples | Primary Research Applications | Key Considerations |
|---|---|---|---|
| Selective BH3-Mimetics | Venetoclax (BCL-2), A-1331852 (BCL-XL), S63845 (MCL1) | Target validation, single-agent efficacy studies, mechanism of action | Off-target effects at high concentrations, different potency across models |
| Dual/Pan-Inhibitors | Navitoclax (BCL-2/BCL-XL) | Overcoming single-agent resistance, combination strategies | Increased toxicity profiles, thrombocytopenia for BCL-XL inhibitors |
| Cell Line Models | Cancer cell lines (CCLE), Primary patient-derived cells, Genetically engineered lines (e.g., BAX/BAK KO) | Pathway mapping, biomarker discovery, resistance modeling | Variable BCL-2 dependency patterns across cancer types |
| Stromal Co-culture Systems | HS5 stromal cells, Primary bone marrow stromal cells | Microenvironment-mediated resistance studies, protective mechanism elucidation | Contact-dependent vs. soluble factor effects, separation methodology |
| Apoptosis Detection | Annexin V/PI staining, Caspase 3/7 activity assays, Mitochondrial membrane potential dyes | Quantifying apoptotic response, timing of cell death | Distinguishing apoptosis from other cell death mechanisms |
| Protein Interaction Tools | Proximity ligation assays, Co-immunoprecipitation, BH3 profiling | Mechanistic studies, resistance mechanism elucidation, dynamic protein interactions | Technical variability in protein-protein interaction assays |
| Gene Expression Analysis | qPCR primers for BCL2 family, RNA-seq, Nanostring panels | Biomarker development, expression correlation with sensitivity | Post-translational regulation may not correlate with mRNA levels |
| Animal Models | PDX models, Genetically engineered mouse models, Xenograft systems | In vivo efficacy, toxicity assessment, combination therapy evaluation | Species-specific differences in BCL-2 family function |
The comparative analysis of BCL-2, BCL-XL, and MCL1 reveals a complex landscape of therapeutic opportunities and challenges. While BCL-2 inhibition with venetoclax has demonstrated remarkable success in specific hematologic malignancies, the therapeutic targeting of BCL-XL and MCL1 remains challenging due to on-target toxicities. Future directions include the development of novel therapeutic modalities such as PROTACs, antibody-drug conjugates, and combination strategies that simultaneously target multiple anti-apoptotic proteins at sub-therapeutic doses to maximize efficacy while minimizing toxicity [2]. The comprehensive understanding of BCL-2 family biology, expression patterns across malignancies, and compensatory mechanisms will continue to guide the rational development of next-generation therapeutics that exploit the fundamental regulators of mitochondrial apoptosis for cancer therapy.
The Bcl-2 family proteins, particularly Bcl-2 and Bcl-xL, are established as critical regulators of mitochondrial apoptosis with their roles in cancer well-characterized. However, emerging research reveals their significant potential in neurodegenerative and autoimmune diseases through mechanisms extending beyond their canonical anti-apoptotic functions. This whitepaper synthesizes current understanding of Bcl-2 and Bcl-xL in neuronal function and immune regulation, detailing their non-apoptotic activities in metabolic regulation, synaptic transmission, and cell cycle control. We provide comprehensive experimental methodologies for investigating these pathways and analyze the challenges and opportunities for therapeutic targeting beyond oncology, supported by quantitative data and visual signaling pathways.
The Bcl-2 family proteins serve as central regulators of the intrinsic apoptotic pathway, maintaining cellular homeostasis through a delicate balance between pro-survival (Bcl-2, Bcl-xL, Mcl-1) and pro-apoptotic members (Bax, Bak, BH3-only proteins) [60] [54]. These proteins control mitochondrial outer membrane permeabilization (MOMP), which leads to cytochrome c release and caspase activation [66]. While cancer therapeutics have successfully targeted these proteins, particularly with Bcl-2 inhibitors like venetoclax, their roles in physiological processes beyond oncology remain underexplored.
Bcl-2 and Bcl-xL, though structurally similar and often functioning in the same apoptotic pathway, exhibit significant functional differences in their mechanisms and potency [82]. Research demonstrates Bcl-xL is approximately ten times more effective than Bcl-2 in repressing apoptosis when expressed in breast cancer cell lines, mediated by differences in inhibiting specific subcellular pathways [82]. This functional divergence extends to their non-apoptotic roles, suggesting tissue and context-specific functions that may be exploited therapeutically.
Molecular Mechanisms of Bcl-2 and Bcl-xL
Canonical Apoptotic Regulation
The anti-apoptotic Bcl-2 family members, including Bcl-2 and Bcl-xL, preserve mitochondrial membrane integrity by sequestering pro-apoptotic proteins like Bax and Bak, or by binding and neutralizing activator BH3-only proteins (Bim, tBid) [60] [66]. Their overexpression in cancer cells creates a state of "primed for death" dependency, wherein inhibition displaces pro-apoptotic proteins to trigger caspase activation [66].
Non-Apoptotic Functions
Metabolic Regulation and Bioenergetics
Bcl-xL plays a crucial role in neuronal metabolism by enhancing ATP generation to fuel energy-intensive processes like synaptic transmission and axon pruning [83]. It localizes to both the outer and inner mitochondrial membranes, where it interacts with voltage-dependent anion channel (VDAC) to control ADP/ATP trafficking and directly binds the ATP synthase β subunit to stabilize mitochondrial membrane potential and increase ATP production [83]. These interactions position Bcl-xL as a key regulator of mitochondrial metabolism independent of its apoptotic function.
Cell Cycle Regulation
Bcl-xL and Bcl-2 coordinately regulate apoptosis and cell cycle progression, with both functions being intrinsically linked [9]. These proteins delay cell cycle entry from quiescence (G0) and prolong G0-G1 transition through mechanisms involving upregulation of the cdk inhibitor p27 and the pRB family member p130 [9]. This dual functionality suggests they integrate survival signals with proliferation control, particularly relevant in tissues requiring precise cellular turnover regulation.
Calcium Homeostasis
Bcl-xL impacts intracellular calcium trafficking through interactions with the inositol triphosphate receptor (IP3R) at the endoplasmic reticulum [83]. In neurons, this contributes to calcium homeostasis critical for synaptic transmission and plasticity, connecting Bcl-xL function to neuronal excitability and signaling.
Table 1: Quantitative Comparison of Bcl-2 and Bcl-xL Properties
| Property | Bcl-2 | Bcl-xL | Experimental Context |
|---|---|---|---|
| Anti-apoptotic potency | Baseline | ~10x more effective | MCF-7 breast cancer cells treated with doxorubicin [82] |
| Inhibition of ceramide pathway | Functions downstream of ceramide | Targets point upstream of ceramide generation | TNFα- and camptothecin-induced apoptosis [84] |
| Effect on ceramide-induced apoptosis | Protective | No protection | Exogenous ceramide treatment [84] |
| Cell cycle regulation | Delays G0-G1 transition | Delays G0-G1 transition | Serum-starved fibroblasts [9] |
| Endoplasmic reticulum activity | Inhibits apoptosis induced by ceramide and thapsigargin only | Inhibits apoptosis induced by all tested drugs (ceramide, thapsigargin, doxorubicin, TNFα) | Organelle-targeted mutants in MCF-7 cells [82] |
Bcl-2 Proteins in Neurodegenerative Diseases
Neuronal Development and Function
Bcl-xL plays a major role in neuronal development, as demonstrated by bclx knock-out mice dying embryonically at day 13.5 with massive apoptosis in the central nervous system (CNS) [83]. In the mature CNS, Bcl-xL facilitates ATP generation for energy-demanding processes including synapse formation, axon pruning, and nerve cell plasticity [83]. It regulates mitochondrial fission through interaction with DRP1, affecting synaptic vesicle recycling and mitochondrial localization at synapses [83].
Synaptic Transmission and Plasticity
Bcl-xL contributes to synaptic transmission through its effects on mitochondrial metabolism and possible regulation of localized caspase activity [83]. It enables morphological changes such as sprouting and retraction of axon branches in CNS plasticity, potentially through controlled, non-apoptotic caspase activation that doesn't trigger cell death [83].
Implications for Specific Neurodegenerative Disorders
Impaired Bcl-xL function correlates with several neurodegenerative conditions, though underlying mechanisms remain poorly characterized [83]. Evidence links Bcl-xL dysfunction to:
- Parkinson's disease (PD): Bcl-xL interacts with PINK1 kinase, potentially contributing to PINK1-dependent protection against cell death, and prevents mitochondrial localization of Parkin, inhibiting mitophagy [83] [83].
- Amyotrophic lateral sclerosis (ALS): Bcl-xL shows protective roles in motor neurons [83] [85].
- Spinal cord muscular atrophy and Friedrich ataxia: Correlations with Bcl-xL dysfunction have been observed [83] [76] [54].
Bcl-2 Proteins in Autoimmune Diseases
Regulation of Lymphocyte Homeostasis
Bcl-2 and Bcl-xL exhibit a highly regulated expression pattern during B cell maturation, with cell death being a common event during development that serves to select functional populations and remove potentially autoreactive cells [85]. Transgenic overexpression of Bcl-2 in developing B cells, particularly with T cell dependent costimulatory signals, results in modified B cell repertoire and production of pathogenic autoantibodies [85].
Disregulated Apoptosis in Autoimmunity
The disregulation of programmed cell death in B cells may cause autoimmune manifestations, as demonstrated in mouse models [85]. While the involvement in human autoimmune diseases requires further investigation, the fundamental role of Bcl-2 proteins in lymphocyte selection and homeostasis positions them as potential therapeutic targets for restoring immune tolerance.
Therapeutic Targeting and Experimental Approaches
Current Bcl-2 Inhibitors and Their Limitations
The Bcl-2 inhibitor venetoclax has demonstrated remarkable efficacy in hematological malignancies, with the global BCL-2 inhibitors market projected to grow from $2.46 billion in 2025 to $4.63 billion by 2029 [76]. However, its application is limited by:
- Differential targeting: Venetoclax specifically inhibits Bcl-2 but not Bcl-xL or Mcl-1, allowing resistance through these alternative anti-apoptotic proteins [66].
- Tissue-specific toxicity: Platelet toxicity presents a major challenge for Bcl-xL inhibition, as Bcl-xL is critical for platelet survival [86].
Emerging Strategies for Neurological and Autoimmune Applications
Selective Targeting Approaches
Next-generation inhibitors focus on improved specificity and tissue-selective targeting. Eilean Therapeutics' eiletoclax represents a highly selective BCL-2 inhibitor with reduced interaction with healthy immune cells and potentially improved safety margins [76]. Navitoclax, which targets both BCL-2 and BCL-xL, is in advanced clinical trials for hematological cancers, though its application in non-oncological contexts requires careful toxicity management [86].
Senolytic Applications
Bcl-xL is a target of various senolytic agents, with fisetin and quercetin inducing apoptosis in senescent human umbilical vein endothelial cells by inhibiting Bcl-xL [54]. Fisetin demonstrates roughly twice the senolytic potency of quercetin [54], suggesting potential applications in age-related neurodegenerative diseases characterized by cellular senescence.
Experimental Methodology for Investigating Bcl-2 Protein Functions
Assessing Apoptotic Function
CERAMIDE PATHWAY ANALYSIS PROTOCOL
- Cell Lines: MCF-7 breast cancer cells, Rat-1 fibroblasts
- Apoptosis Inducers: TNFα (29 ng/mL + cycloheximide 10 ng/mL for 30h), camptothecin, C2-ceramide (70 μM for 20h)
- Assessment Methods:
- Quantitative immunoblotting for caspase activation (PARP cleavage)
- Endogenous ceramide measurement by lipid extraction and TLC
- Caspase-8-like activity assay in cell lysates
- Experimental Design: Compare Bcl-2 vs. Bcl-xL overexpressing cells for differential response to inducers [84] [82]
Evaluating Metabolic Functions in Neurons
NEURONAL METABOLIC PROFILING PROTOCOL
- Primary Cultures: Cortical, hippocampal, or motor neurons from embryonic mice
- Bcl-xL Modulation: siRNA knockdown or overexpression via lentiviral vectors
- Metabolic Assays:
- ATP quantification via luciferase-based assays
- Mitochondrial membrane potential (Δψm) using TMRE or JC-1 dyes
- Oxygen consumption rate (OCR) via Seahorse Analyzer
- Calcium imaging with Fura-2 AM for ER-mitochondria Ca2+ transfer
- Functional Readouts: Synaptic vesicle recycling, mitochondrial transport, axon outgrowth [83]
Cell Cycle Regulation Studies
CELL CYCLE ENTRY ANALYSIS PROTOCOL
- Cell Models: Rat1-MycER cells, NIH 3T3 fibroblasts
- Synchronization: Serum starvation for 72h (0.05-0.5% FBS)
- Cell Cycle Stimulation: 10% serum addition or 4-hydroxytamoxifen (4-OHT) for MycER activation
- Analysis Timepoints: 0, 4, 8, 12, 16, 20h post-stimulation
- Assessment Methods:
- Flow cytometry for DNA content (propidium iodide)
- BrdU incorporation for S-phase entry
- Pyronin Y staining for RNA content to distinguish G0/G1
- Forward scatter for cell size analysis [9]
Table 2: Essential Research Reagents for Bcl-2/Bcl-xL Investigations
| Reagent/Cell Line | Application | Key Features | Research Utility |
|---|---|---|---|
| MCF-7 cells | Apoptosis pathway analysis | Minimal endogenous Bcl-xL; reducible Bcl-2 in estrogen-depleted medium; caspase-3 deficient | Clean background for exogenous protein expression studies [82] |
| Rat1-MycER cells | Cell cycle regulation studies | 4-OHT inducible Myc activation; synchronous cell cycle entry | Precise temporal control of cell cycle progression [9] |
| Organelle-targeted mutants (Bcl2-acta, Bcl2-cb5) | Subcellular pathway mapping | Bcl-2/Bcl-xL targeted to mitochondria or ER using ActA or cytochrome b5 tails | Determination of organelle-specific apoptotic pathways [82] |
| Venetoclax (ABT-199) | Selective BCL-2 inhibition | Highly specific BCL-2 binder; spares BCL-xL and Mcl-1 | Tool for dissecting BCL-2-specific functions; control for specificity [66] |
| Bcl-xL BH4 domain mutants (Y22A/F) | Structure-function studies | Mutation in conserved BH4 tyrosine residue | Testing functional segregation of anti-apoptotic vs. cell cycle activities [9] |
Signaling Pathway Visualizations
Bcl-2 Family Regulation of Mitochondrial Apoptosis
Non-Apoptotic Functions of Bcl-xL in Neurons
The expanding understanding of Bcl-2 and Bcl-xL functions beyond apoptosis regulation reveals significant therapeutic potential in neurodegenerative and autoimmune diseases. Their roles in metabolic regulation, synaptic function, and immune cell homeostasis provide multiple targeting opportunities, though significant challenges remain in achieving tissue-specific effects while minimizing toxicity.
Future research should focus on:
- Developing CNS-penetrant selective modulators with improved safety profiles
- Elucidating temporal expression patterns in disease progression to identify optimal therapeutic windows
- Exploring combination approaches that target multiple aspects of disease pathophysiology
- Advancing gene therapy strategies for tissue-specific modulation
As our understanding of the complex biology of Bcl-2 family proteins deepens, so too will opportunities for innovative therapeutics that extend far beyond their current oncology applications, potentially offering new treatment paradigms for currently intractable neurodegenerative and autoimmune conditions.
The B-cell lymphoma 2 (BCL-2) family of proteins, particularly BCL-2 and BCL-XL, function as critical regulators of apoptotic cell death, serving as fundamental gatekeepers in cellular homeostasis and survival pathways. Their frequent dysregulation in cancer and other pathological conditions has established them as prominent therapeutic targets. This whitepaper evaluates the substantial clinical achievements of BCL-2 family targeting, highlighting the transformative success of venetoclax in hematologic malignancies. It further delineates the significant challenges encountered in targeting paralogs like BCL-XL and MCL-1, and explores the novel therapeutic strategies, including PROTACs and antibody-drug conjugates, designed to overcome these hurdles. The discussion is framed within the context of apoptosis research, detailing the molecular mechanisms, experimental methodologies, and future directions that will define the next era of clinical impact for this target class.
The BCL-2 protein family constitutes a key group of regulators that maintain cellular homeostasis by modulating apoptosis, a genetically regulated form of cell death responsible for the programmed culling of cells during normal development and homeostasis [44]. The founding member, BCL-2, was discovered in 1984 as the gene involved in the t(14;18) chromosomal translocation found in most follicular lymphomas [6]. This translocation results in the overexpression of BCL-2, which functions as an oncogene by blocking cell death rather than promoting proliferation [6]. The family is structurally defined by the presence of BCL-2 homology (BH) domains and is functionally divided into three subgroups: anti-apoptotic proteins (e.g., BCL-2, BCL-XL, MCL-1), pro-apoptotic effector proteins (e.g., BAX, BAK), and BH3-only proteins (e.g., BIM, BID, PUMA) that initiate apoptosis signaling [6] [44] [69].
The intrinsic apoptosis pathway is critically regulated by the BCL-2 protein family at the mitochondrial outer membrane. Anti-apoptotic proteins like BCL-2 and BCL-XL promote cell survival by sequestering pro-apoptotic proteins and preventing mitochondrial outer membrane permeabilization (MOMP), an event considered the point of no return for cell death [6] [70]. MOMP leads to the release of cytochrome c into the cytosol, formation of the apoptosome complex, and activation of caspase cascades that execute cell death [6]. In cancer, the overexpression of anti-apoptotic BCL-2 proteins allows tumor cells to evade this programmed cell death, contributing to tumorigenesis and resistance to therapy [70] [44]. This fundamental role in apoptosis regulation has made the BCL-2 family, particularly BCL-2 and BCL-XL, compelling targets for cancer drug development.
Success Stories: Clinical Translation of BCL-2 Inhibition
Venetoclax: A First-in-Class BH3-Mimetic
The most significant success story in targeting the BCL-2 family is the development and clinical approval of venetoclax (ABT-199). Venetoclax is a first-in-class, selective BCL-2 inhibitor that functions as a BH3-mimetic, designed to bind with high affinity into the hydrophobic groove of BCL-2, thereby displacing pro-apoptotic proteins and triggering apoptosis in cancer cells [6] [44]. Its discovery represented a breakthrough in targeting protein-protein interfaces with small molecules, emerging from earlier compounds like ABT-737 and navitoclax (ABT-263) that inhibited both BCL-2 and BCL-XL but exhibited dose-limiting toxicities [6].
Venetoclax has demonstrated remarkable efficacy with manageable toxicities, transforming the treatment landscape for several hematologic malignancies [6]. It received FDA and EMA approval in 2016 and is now approved for chronic lymphocytic leukemia (CLL) and acute myeloid leukemia (AML) [44] [69]. The drug has shown promising results in other B-cell malignancies, including Waldenström macroglobulinemia (WM), where it targets the documented BCL-2 overexpression that promotes cell survival and resistance to therapy [69]. Clinical studies have demonstrated its efficacy even in patients previously treated with Bruton tyrosine kinase inhibitors (BTKis), with WM cells acquiring resistance through BCL-2 upregulation, creating vulnerability to venetoclax [69].
Table 1: Clinical Impact of Approved and Investigational BCL-2 Family-Targeted Agents
| Therapeutic Agent | Molecular Target | Approval Status | Key Indications | Notable Efficacy/Safety Profile |
|---|---|---|---|---|
| Venetoclax (ABT-199) | BCL-2 | FDA/EMA Approved (2016) | CLL, AML | Remarkable efficacy with manageable toxicities; transforms treatment of hematologic malignancies [6] |
| Navitoclax (ABT-263) | BCL-2, BCL-XL, BCL-w | Clinical Evaluation | Investigational for various cancers | Dose-limiting thrombocytopenia due to BCL-XL inhibition [6] |
| Sonrotoclax | BCL-2 | Clinical Evaluation | Investigational for hematologic cancers | Chemically similar to venetoclax; under evaluation alone and in combination [6] |
| Lisaftoclax | BCL-2 | Clinical Evaluation | Investigational for hematologic cancers | Chemically similar to venetoclax; under evaluation alone and in combination [6] |
Expanding the Clinical Utility of BCL-2 Inhibition
Following the success of venetoclax, several chemically similar BCL-2 inhibitors, including sonrotoclax and lisaftoclax, are currently under clinical evaluation both as monotherapies and in combination regimens [6]. The efficacy of venetoclax has also been demonstrated in combination with standard cancer regimens, showing enhanced activity, though further studies are required to elucidate the mechanisms of its synergistic action and identify which patients benefit most from combination therapy [69]. The clinical success of venetoclax showcases the profound impact that fundamental mechanistic research on apoptosis regulation can have on patient lives and represents a validation of the BH3-mimetic approach for targeting anti-apoptotic BCL-2 family proteins.
Ongoing Challenges in Targeting BCL-2 Paralogs
Despite the remarkable success of selective BCL-2 inhibition, the targeting of other key anti-apoptotic BCL-2 family members, particularly BCL-XL and MCL-1, has proven more challenging, limiting the broader clinical applicability of this therapeutic class.
The BCL-XL Conundrum: Efficacy vs. Toxicity
Genetic analyses have highlighted the importance of BCL-XL and MCL-1 across different cancer types, suggesting substantial clinical utility for inhibitors targeting these proteins [6]. However, the development of BH3-mimetics targeting BCL-XL has been hampered by on-target, mechanism-based toxicities. The most significant challenge is thrombocytopenia, as platelets are uniquely dependent on BCL-XL for survival. Inhibition of BCL-XL leads to rapid apoptosis of platelets, resulting in dose-limiting thrombocytopenia that has precluded the clinical development of dual BCL-2/BCL-XL inhibitors like navitoclax [6]. This toxicity represents a critical barrier for the systemic administration of BCL-XL inhibitors.
MCL-1 Inhibition: Cardiac and Safety Concerns
Similarly, the development of MCL-1 inhibitors has faced substantial safety challenges. The primary concern is the occurrence of cardiac toxicities, which have been significant enough to halt the clinical development of several investigative MCL-1 inhibitors [6]. This toxicity profile is likely related to the essential role of MCL-1 in maintaining cardiac function and cellular homeostasis in normal tissues. The narrow therapeutic window resulting from these on-target toxicities presents a formidable obstacle for the direct and systemic inhibition of MCL-1 as a therapeutic strategy.
Tumor Heterogeneity and Adaptive Resistance
Beyond specific toxicities, the broader challenge in targeting the BCL-2 family stems from tumor heterogeneity and adaptive resistance mechanisms. Many malignancies demonstrate co-dependence on multiple anti-apoptotic proteins, allowing cancer cells to compensate for the inhibition of one member by upregulating another, thereby maintaining their survival and developing resistance to single-agent therapy [6] [70]. This biological redundancy within the BCL-2 family network necessitates sophisticated targeting strategies that can address the complex interplay between these proteins in different cancer types and microenvironments.
Table 2: Key Challenges in Targeting Major Anti-Apoptotic BCL-2 Family Proteins
| Target Protein | Primary Challenge | Underlying Mechanism | Impact on Clinical Development |
|---|---|---|---|
| BCL-XL | Dose-limiting thrombocytopenia | Platelet survival is dependent on BCL-XL; inhibition triggers apoptosis in platelets [6] | Precluded clinical development of dual BCL-2/BCL-XL inhibitors (e.g., navitoclax) for broad applications [6] |
| MCL-1 | Cardiac toxicity | MCL-1 is essential for maintaining cardiac function; inhibition leads to on-target cardiac damage [6] | Halted clinical development of several investigative MCL-1 inhibitors due to safety concerns [6] |
| Pan-BCL-2 Inhibition | Tumor heterogeneity & adaptive resistance | Malignancies often co-express multiple anti-apoptotic proteins; inhibition of one leads to compensatory upregulation of others [6] [70] | Limits efficacy of single-agent therapy; necessitates rational combination strategies or more sophisticated targeting approaches [6] |
Emerging Strategies and Novel Therapeutic Approaches
To overcome the challenges associated with targeting BCL-2 paralogs, several innovative strategies are under investigation that aim to achieve tumor-specific inhibition while sparing normal tissues.
PROTACs and Selective Drug Delivery
Novel targeting approaches using proteolysis targeting chimeras (PROTACs) offer a promising strategy for achieving tumor-specific BCL-XL or MCL-1 inhibition [6]. PROTACs are heterobifunctional molecules that recruit the target protein to an E3 ubiquitin ligase, leading to its ubiquitination and subsequent degradation by the proteasome. This approach may offer advantages over traditional inhibition, including potential for enhanced selectivity, catalytic mode of action, and ability to target proteins traditionally considered "undruggable." Selective drug delivery strategies, such as antibody-drug conjugates (ADCs), are also being explored to direct the potent activity of BCL-XL or MCL-1 inhibitors specifically to tumor cells, thereby minimizing on-target toxicities in normal tissues like platelets or cardiac muscle [6].
Targeting the BH4 Domain and Ubiquitin-Proteasome System
Beyond the canonical hydrophobic groove, alternative targeting sites on BCL-2 proteins are being investigated. Tools targeting the BH4 domain of BCL-2 represent a novel approach that may offer different selectivity profiles and therapeutic windows [6]. Additionally, research is exploring the intricate interplay between the ubiquitin-proteasome system (UPS) and BCL-2 family members. The UPS controls the stability of both pro- and anti-apoptotic BCL-2 family proteins, and proteasome inhibitors can disrupt this balance, leading to the accumulation of pro-apoptotic factors and pushing cancer cells toward apoptosis [70]. Targeting specific E3 ubiquitin ligases or their substrates offers another promising avenue for indirectly modulating the BCL-2 family network in cancer cells.
Rational Combination Therapies
Given the complexity of apoptotic regulation and the redundancy within the BCL-2 family, rational combination therapies represent a crucial strategic direction. Combining BH3-mimetics with other targeted agents, chemotherapy, or immunotherapy can help overcome intrinsic and adaptive resistance mechanisms [69]. For instance, in Waldenström macroglobulinemia, studies are exploring venetoclax in combination with standard regimens to enhance activity, though further work is needed to identify optimal combinations and predictive biomarkers for patient selection [69]. The future clinical applicability of BCL-2 family targeting will likely depend on these sophisticated combination approaches tailored to the molecular dependencies of specific cancer subtypes.
Experimental Methodologies and Research Tools
Key Experimental Protocols
Research on BCL-2 family proteins and their therapeutic targeting relies on several cornerstone methodologies that provide mechanistic insights and preclinical validation.
Surface Plasmon Resonance (SPR) for Binding Affinity Measurements: SPR is used to quantitatively characterize the binding interactions between BH3-mimetics and their target BCL-2 proteins. The target protein (e.g., BCL-2, BCL-XL) is immobilized on a sensor chip, and the small molecule inhibitor is flowed over the surface at varying concentrations. The association and dissociation rates are measured in real-time, allowing calculation of binding affinity (KD), which is critical for evaluating inhibitor potency and selectivity during drug development [6].
Mitochondrial Outer Membrane Permeabilization (MOMP) Assays: Functional assessment of BCL-2 protein activity and inhibition is performed through MOMP assays. Isolated mitochondria are treated with BH3-only proteins or BH3-mimetics in the presence or absence of anti-apoptotic proteins. MOMP is quantified by measuring the release of cytochrome c from the intermembrane space into the supernatant using techniques like Western blotting or ELISA. This assay directly evaluates the functional consequence of inhibiting anti-apoptotic BCL-2 proteins [6] [70].
Co-Immunoprecipitation (Co-IP) for Protein-Protein Interactions: Co-IP is used to study interactions between BCL-2 family members and the disruption of these interactions by BH3-mimetics. Cells or lysates are treated with compounds, followed by immunoprecipitation of a specific BCL-2 protein (e.g., BCL-2). Co-precipitating binding partners (e.g., BIM, BAX) are then detected by Western blotting. The dissociation of these complexes upon treatment indicates effective target engagement by the BH3-mimetic [6].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Studying BCL-2 Family Proteins and BH3-Mimetics
| Research Reagent | Function/Application | Specific Examples |
|---|---|---|
| BH3-Mimetic Compounds | Small molecule inhibitors that bind to anti-apoptotic BCL-2 proteins; used to induce apoptosis in experimental systems | ABT-737 (BCL-2/BCL-XL/BCL-w inhibitor), ABT-199/Venetoclax (BCL-2 selective), Navitoclax (BCL-2/BCL-XL/BCL-w) [6] |
| Recombinant BCL-2 Family Proteins | Purified proteins for structural studies, binding assays, and in vitro experiments; essential for characterizing interactions | BCL-2, BCL-XL, MCL-1 for NMR, X-ray crystallography, and SPR studies [6] |
| BH3-Only Peptides | Synthetic peptides corresponding to BH3 domains; used to probe dependencies and disrupt specific protein interactions | BIM BH3, BAD BH3, NOXA BH3; used in BH3 profiling to determine mitochondrial priming [6] |
| Antibodies for Detection | Immunodetection of BCL-2 family proteins and their modifications in techniques like Western blotting, IHC, and Co-IP | Anti-BCL-2, Anti-BCL-XL, Anti-MCL-1, Anti-BAX, Anti-BAK, Anti-BIM; phospho-specific antibodies for PTM studies [61] |
Diagram 1: BCL-2 Family Regulation of Apoptosis and BH3-Mimetic Mechanism of Action. This diagram illustrates the intrinsic apoptosis pathway and how BH3-mimetic drugs promote cell death by inhibiting anti-apoptotic BCL-2 proteins.
The targeting of BCL-2 family proteins represents both a remarkable success story and an ongoing challenge in translational cancer research. The approval and clinical success of venetoclax have validated the fundamental research on apoptosis regulation and demonstrated that directly targeting protein-protein interactions with small molecules is a viable therapeutic strategy. However, the field continues to face significant hurdles in expanding this success to other critical BCL-2 family members, particularly BCL-XL and MCL-1, due to on-target toxicities that limit their therapeutic window.
The future of targeting the BCL-2 family lies in developing more sophisticated approaches that can achieve tumor-specific inhibition while sparing normal tissues. PROTACs, antibody-drug conjugates, and other novel delivery systems hold promise for overcoming the toxicity barriers that have hampered development of BCL-XL and MCL-1 inhibitors. Additionally, rational combination therapies that address the redundancy and compensatory mechanisms within the BCL-2 network will be essential for overcoming resistance and expanding the utility of these agents across a broader range of malignancies.
As our understanding of the non-canonical functions of BCL-2 family proteins in autophagy, metabolism, and cellular homeostasis continues to evolve, so too will our therapeutic strategies. The continued translation of basic apoptosis research into clinical advances promises to further expand the therapeutic landscape and improve outcomes for patients with cancer and potentially other diseases characterized by dysregulated cell survival.
Conclusion
Bcl-2 and Bcl-xL stand as master regulators of cellular fate, with their targeted inhibition representing a landmark success in translational medicine. The development of venetoclax has unequivocally validated the therapeutic potential of BH3-mimetics, particularly in hematologic cancers. However, the journey is far from complete. Future research must prioritize overcoming resistance mechanisms, mitigating the on-target toxicities of inhibiting Bcl-xL and MCL1 through novel platforms like PROTACs, and expanding the utility of these agents into solid tumors and non-oncological indications. A deeper understanding of tissue-specific functions, non-canonical roles in metabolism, and interactions with non-coding RNAs will be crucial. The continued elucidation of the Bcl-2 family's biology promises to unlock the next generation of targeted therapies, further refining our ability to manipulate cell survival for therapeutic gain.
References
- 1. BCL-2: Mechanisms and Prevalence | OncLive [https://www.onclive.com/view/bcl2-mechanisms-and--prevalence]
- 2. The BCL2 family: from apoptosis mechanisms to new advances in targeted therapy | Signal Transduction and Targeted Therapy [https://www.nature.com/articles/s41392-025-02176-0]
- 3. Bcl-2 - Wikipedia [https://en.wikipedia.org/wiki/Bcl-2]
- 4. - Wikipedia Chromosomal translocation [https://en.wikipedia.org/wiki/Chromosomal_translocation]
- 5. The role of Bcl ‑ 2 in controlling the transition between autophagy and... [https://www.spandidos-publications.com/10.3892/mmr.2025.13537?text=fulltext]
- 6. The BCL family: from 2 to new advances in... apoptosis mechanisms [https://pmc.ncbi.nlm.nih.gov/articles/PMC11926181/]
- 7. The role of BCL-2 family proteins in regulating apoptosis and cancer therapy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9597512/]
- 8. Frontiers | Structural Details of BH 3 Motifs and BH 3-Mediated... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2022.864874/full]
- 9. Bcl-xL/Bcl-2 coordinately regulates apoptosis, cell cycle arrest and cell cycle entry - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC213787/]
- 10. by which Bak and Bax permeabilise mitochondria during... Mechanisms [https://pmc.ncbi.nlm.nih.gov/articles/PMC2736138/]
- 11. Computational design of Bax-inhibiting peptides - Materials Advances... [https://pubs.rsc.org/en/content/articlehtml/2025/ma/d4ma01142b]
- 12. Inhibitor of apoptosis - Wikipedia [https://en.wikipedia.org/wiki/Inhibitor_of_apoptosis]
- 13. Mechanisms of Action of Bcl-2 Family Proteins - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3683897/]
- 14. MOMP, cell suicide as a BCL-2 family business | Cell Death & Differentiation [https://www.nature.com/articles/cdd2017179]
- 15. The Mathematical Model of the Bcl - 2 Mediated Family ... MOMP [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0081861]
- 16. Current Advances and Future Strategies for BCL-2 Inhibitors: Potent Weapons against Cancers - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10605442/]
- 17. BCL2 Inhibitors: What's the Latest Research? | Dana-Farber Cancer Institute [https://blog.dana-farber.org/insight/2024/03/bcl2-inhibitors-whats-the-latest-research/]
- 18. - Bcl and 2 - Bcl CD95-mediated xL by preventing... inhibit apoptosis [https://pubmed.ncbi.nlm.nih.gov/11801595/]
- 19. - BCL / xL L1 is a critical anti- BCL protein that promotes the... 2 apoptotic [https://www.nature.com/articles/s41419-020-2589-7?error=cookies_not_supported]
- 20. Multiple Functions of BCL-2 Family Proteins - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3552500/]
- 21. The optimal regulation mode of Bcl - 2 revealed by... apoptotic switch [https://pubmed.ncbi.nlm.nih.gov/28923482/]
- 22. The BCL family: from 2 mechanisms to new advances in... apoptosis [https://www.nature.com/articles/s41392-025-02176-0?error=cookies_not_supported&code=dcd7f45c-7fb6-43ef-bdbb-6618c8cef00d]
- 23. Regulation of mitochondrial metabolism : yet another facet in the... [https://pubmed.ncbi.nlm.nih.gov/21486225/]
- 24. Modulation of Ca2+ signaling by antiapoptotic Bcl - 2 versus Bcl - xL ... [https://pubmed.ncbi.nlm.nih.gov/36162541/]
- 25. BCL-2 family isoforms in apoptosis and cancer | Cell Death & Disease [https://www.nature.com/articles/s41419-019-1407-6]
- 26. : Their BH and efficacy in cancer chemotherapy 3 mimetics action [https://www.oatext.com/BH3-mimetics-Their-action-and-efficacy-in-cancer-chemotherapy.php]
- 27. Inhibiting protein–protein interactions using designed molecules - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0959440X05000060]
- 28. BH3-mimetics: recent developments in cancer therapy | Journal of Experimental & Clinical Cancer Research | Full Text [https://jeccr.biomedcentral.com/articles/10.1186/s13046-021-02157-5]
- 29. Rational design of new class of BH - 3 as inhibitors of the... mimetics [https://pubmed.ncbi.nlm.nih.gov/21528891/]
- 30. Intracellular Delivery System for Antibody–Peptide Drug Conjugates - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4427876/]
- 31. Found in translation: how preclinical research is guiding the clinical development of the BCL-2-selective inhibitor venetoclax - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5728441/]
- 32. ABT-199 (venetoclax) and BCL-2 inhibitors in clinical development | Journal of Hematology & Oncology | Full Text [https://jhoonline.biomedcentral.com/articles/10.1186/s13045-015-0224-3]
- 33. Frontiers | Mechanisms of action of the BCL-2 inhibitor venetoclax in multiple myeloma: a literature review [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2023.1291920/full]
- 34. - Wikipedia Navitoclax [https://en.wikipedia.org/wiki/Navitoclax]
- 35. : Uses, Interactions, Navitoclax Mechanism of Action [https://go.drugbank.com/drugs/DB12340]
- 36. Current Advances and Future Strategies for BCL-2 Inhibitors: Potent Weapons against Cancers - PubMed [https://pubmed.ncbi.nlm.nih.gov/37894324/]
- 37. Why do BCL-2 inhibitors work and where should we use them in the clinic? | Cell Death & Differentiation [https://www.nature.com/articles/cdd2017183]
- 38. Review of Venetoclax in CLL , AML and Multiple Myeloma - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8225137/]
- 39. therapy and emerging resistance Venetoclax in mechanisms ... acute [https://www.nature.com/articles/s41419-024-06810-7?error=cookies_not_supported&code=a1bf46bb-1a3e-4af5-9cd3-09fc539ff592]
- 40. Roles and Regulation of BCL-xL in Hematological Malignancies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8876520/]
- 41. Pharmaceutical Approval Update - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4959615/]
- 42. P409: BCL - 2 / bcl - xl inhibition induces apoptosis and circumvents... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10428793/]
- 43. Exploring BCL regulation and upstream signaling transduction in... 2 [https://www.nature.com/articles/s41408-025-01215-x?error=cookies_not_supported&code=86ac5640-4d25-4650-b3d5-401e8bda6b5f]
- 44. Frontiers | The role of BCL - 2 family proteins in regulating apoptosis ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2022.985363/full]
- 45. Potent and Selective BCL - XL Inhibitors and PROTAC Compounds as... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10258826/]
- 46. First-in-Human Study with Preclinical Data of BCL-2/BCL-xL Inhibitor Pelcitoclax in Locally Advanced or Metastatic Solid Tumors - PubMed [https://pubmed.ncbi.nlm.nih.gov/37971712/]
- 47. BH4 domain of Bcl-2 as a novel target for cancer therapy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4882289/]
- 48. BH4 domain of Bcl-2 as a novel target for cancer therapy - PubMed [https://pubmed.ncbi.nlm.nih.gov/26631752/]
- 49. Targeting BCL - 2 in B-cell malignancies and overcoming therapeutic... [https://www.nature.com/articles/s41419-020-03144-y?error=cookies_not_supported&code=799cf9c8-7171-427f-9ef0-07900c14d248]
- 50. - Bcl and 2 - Bcl play important xL the crosstalk between... roles in [https://pubmed.ncbi.nlm.nih.gov/21182587/]
- 51. Venetoclax resistance and acquired BCL2 mutations in chronic lymphocytic leukemia - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6717583/]
- 52. Progress in understanding the mechanisms to... of resistance [https://ehoonline.biomedcentral.com/articles/10.1186/s40164-022-00283-0]
- 53. PROTACs are effective in addressing the platelet toxicity associated with BCL-XL inhibitors - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8293695/]
- 54. Bcl-xL - Wikipedia [https://en.wikipedia.org/wiki/Bcl-xL]
- 55. First in human phase 1 study of DT2216, a selective BCL - xL degrader... [https://jhoonline.biomedcentral.com/articles/10.1186/s13045-025-01753-8]
- 56. - Bcl pathway 2 in solid tumors: a review of clinical trials inhibition [https://link.springer.com/article/10.1007/s12094-022-03070-9]
- 57. - BCL –targeting antibody-drug conjugates are active in preclinical... XL [https://pmc.ncbi.nlm.nih.gov/articles/PMC11451551/]
- 58. 4QVX: Discovery of a Potent and Selective BCL - XL That... Inhibitor [https://www.rcsb.org/structure/4QVX]
- 59. Distinct Roles of Bcl - 2 and Bcl - Xl in the Apoptosis of... | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0019820]
- 60. of Mechanisms - BCL family proteins in mitochondrial 2 apoptosis [https://www.nature.com/articles/s41580-023-00629-4?error=cookies_not_supported&code=f24309eb-a607-4aff-a429-4e9ed9393604]
- 61. Molecular Medicine Reports [https://www.spandidos-publications.com/10.3892/mmr.2025.13537]
- 62. Targeting BCL-2 in B-cell malignancies and overcoming therapeutic resistance | Cell Death & Disease [https://www.nature.com/articles/s41419-020-03144-y]
- 63. Bcl‐2/Bcl‐xL inhibition predominantly synergistically enhances the anti‐neoplastic activity of a low‐dose CUSP9 repurposed drug regime against glioblastoma - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6715605/]
- 64. Molecular basis for the interplay of apoptosis and proliferation... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4620986/]
- 65. Emerging biomarkers and potential therapeutics of the BCL-2 protein family: the apoptotic and anti-apoptotic context | Egyptian Journal of Medical Human Genetics | Full Text [https://jmhg.springeropen.com/articles/10.1186/s43042-024-00485-7]
- 66. Frontiers | BCL-2 inhibitors in hematological malignancies: biomarkers that predict response and management strategies [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2024.1501950/full]
- 67. Expression Profile of BCL - 2 , BCL - XL , and MCL-1 Predicts... [https://pubmed.ncbi.nlm.nih.gov/26939706/]
- 68. - Bcl as a poor prognostic xL and predictor of biomarker to... response [https://www.oncotarget.com/article/24481/text/]
- 69. Frontiers | Targeting BCL in Waldenström macroglobulinemia: from... 2 [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1564869/full]
- 70. A new era in cancer therapy: targeting the Proteasome- Bcl - 2 axis [https://jeccr.biomedcentral.com/articles/10.1186/s13046-025-03505-5]
- 71. BCL-2 Inhibitors, Present and Future - PubMed [https://pubmed.ncbi.nlm.nih.gov/31764121/]
- 72. Selectivity mechanism of BCL - XL / 2 through in silico... inhibition [https://pubs.rsc.org/en/content/articlelanding/2022/cp/d2cp01755e]
- 73. Ascentage Pharma to Present Data from Two Studies for... Clinical [https://www.ascentage.com/ascentage-pharma-to-present-data-from-two-clinical-studies-for-bcl-2-inhibitor-lisaftoclax-including-an-oral-report-at-ash-2025/]
- 74. Dual inhibition of Bcl - 2 and Bcl - xL strikingly enhances... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3578060/]
- 75. and Efficacy of Safety - Bcl Venetoclax in Hematological... 2 Inhibitor [https://pubmed.ncbi.nlm.nih.gov/31293422/]
- 76. Global BCL-2 Inhibitors Industry Outlook 2025-2029: Market Set to Cross $4.63 Billion Milestone [https://www.openpr.com/news/4279044/global-bcl-2-inhibitors-industry-outlook-2025-2029-market-set]
- 77. The BCL-2 protein family: from discovery to drug development | Cell Death & Differentiation [https://www.nature.com/articles/s41418-025-01481-z]
- 78. Key Survival Factor, Mcl - 1 , Correlates with Sensitivity to Combined... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5334148/]
- 79. -Family Dysregulation in B-Cell Malignancies: From Gene... BCL 2 [https://pubmed.ncbi.nlm.nih.gov/30666297/]
- 80. is effective against a subset of small-cell lung cancer... MCL 1 inhibition [https://www.nature.com/articles/s41419-020-2379-2?error=cookies_not_supported&code=05d55aba-1637-41fc-ab26-f76bca806752]
- 81. Frontiers | Co-operation of MCL - 1 and BCL - XL anti- apoptotic proteins... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2024.1394393/full]
- 82. Bcl-XL is qualitatively different from and ten times more effective than Bcl-2 when expressed in a breast cancer cell line | BMC Cancer | Full Text [https://bmccancer.biomedcentral.com/articles/10.1186/1471-2407-6-213]
- 83. Involvement of Bcl - xL in Neuronal Function and Development - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8004157/]
- 84. Distinct sites of action of Bcl - 2 and Bcl - xL in the ceramide pathway of... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1219927/]
- 85. Regulation of B cell apoptosis by Bcl - 2 and Bcl - XL and its role in the... [https://pubmed.ncbi.nlm.nih.gov/9852253/]
- 86. B-cell lymphoma 2 Inhibitors Market Report | Global Forecast From 2025 To 2033 [https://dataintelo.com/report/global-b-cell-lymphoma-2-inhibitors-market]