Caspase Cascade Activation and Executioner Functions: Mechanisms, Regulation, and Therapeutic Targeting
This article provides a comprehensive exploration of the caspase cascade, a cornerstone of programmed cell death (apoptosis) and inflammation.
Caspase Cascade Activation and Executioner Functions: Mechanisms, Regulation, and Therapeutic Targeting
Abstract
This article provides a comprehensive exploration of the caspase cascade, a cornerstone of programmed cell death (apoptosis) and inflammation. Tailored for researchers, scientists, and drug development professionals, it synthesizes foundational knowledge with contemporary research. The scope spans from the fundamental mechanisms of initiator and executioner caspase activation to advanced methodological approaches for studying caspase activity. It further addresses common challenges in experimental models, discusses the validation of caspase functions, and compares the specificity of different caspases. By integrating basic science with clinical applications, this review aims to serve as a critical resource for understanding caspase biology and its immense potential in developing novel therapeutics for cancer, neurodegenerative disorders, and immune diseases.
The Core Machinery: Unraveling Initiator and Executioner Caspase Biology
Caspases are an evolutionarily conserved family of cysteine-dependent aspartate-specific proteases that serve as critical regulators of programmed cell death (PCD) and inflammation [1] [2]. These enzymes hydrolyze peptide bonds in their substrates after specific aspartic acid residues, utilizing a catalytic cysteine residue in their active site [3] [4]. Initially identified for their fundamental role in apoptosis, caspases are now recognized as master regulators of multiple cell death pathways, including pyroptosis and necroptosis, and play essential roles in development, immune responses, and cellular homeostasis [1] [2].
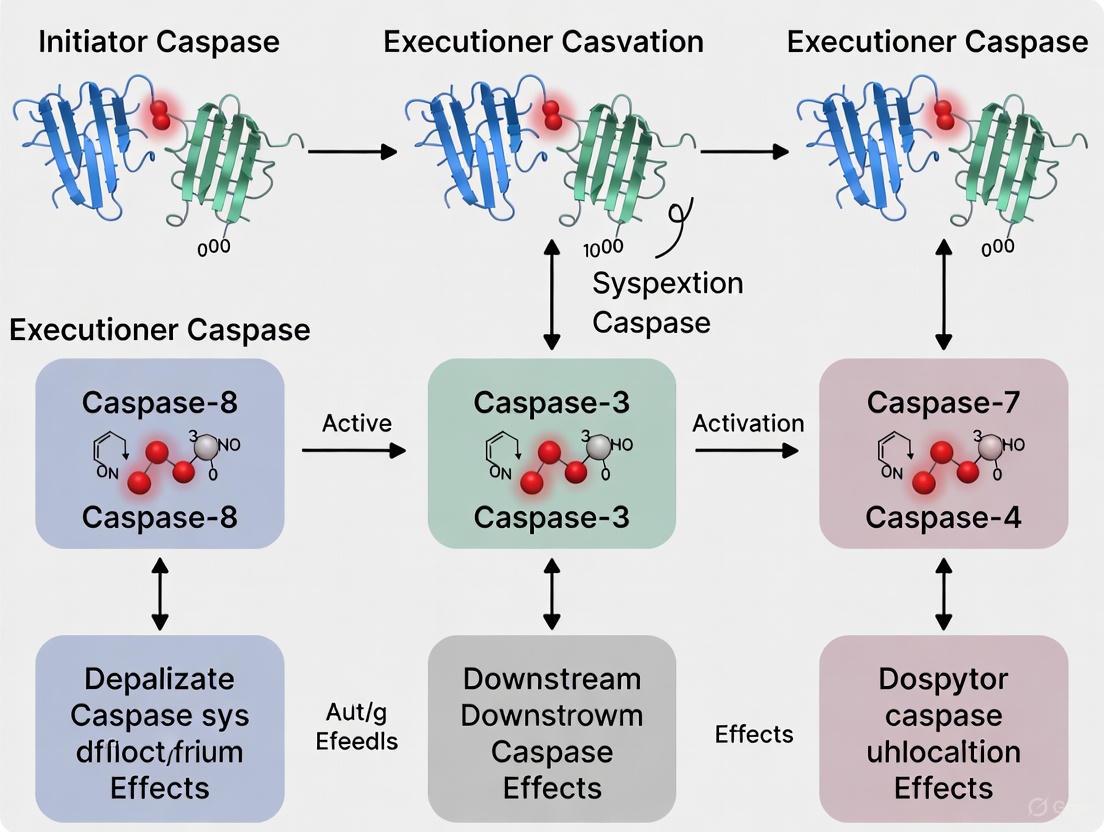
The classification of caspases into initiator, executioner, and inflammatory categories provides a foundational framework for understanding the caspase activation cascade and its functional consequences in both health and disease [4] [2]. This hierarchical organization allows for the precise regulation and amplification of death signals, culminating in the controlled demolition of cellular structures or the activation of inflammatory mediators [3] [5]. Growing understanding of caspase functions has established their importance as potential therapeutic targets for a wide spectrum of diseases, including cancer, neurodegenerative disorders, autoimmune conditions, and infectious diseases [6] [7].
Caspase Classification and Molecular Structure
Caspases are synthesized as inactive zymogens (pro-caspases) that require proteolytic activation for their function [3] [4]. These zymogens consist of three primary domains: an amino-terminal pro-domain, a large catalytic subunit (~20 kDa), and a small catalytic subunit (~10 kDa) [6]. The pro-domain varies significantly among caspase types and contains critical protein-protein interaction motifs that determine how each caspase is activated and recruited into signaling complexes [3] [2].
Table: Caspase Classification by Structure and Function
| Caspase Type | Members | Pro-domain Feature | Activation Mechanism | Primary Functions |
|---|---|---|---|---|
| Initiator | Caspase-2, -8, -9, -10 [4] | Long pro-domain with CARD or DED [3] | Dimerization-induced autoactivation [3] | Initiate apoptosis; signal amplification [5] |
| Executioner | Caspase-3, -6, -7 [4] | Short pro-domain (<30 amino acids) [5] | Cleavage by initiator caspases [3] | Cleave cellular substrates; execute cell death [5] |
| Inflammatory | Caspase-1, -4, -5, -11, -12 [4] [6] | Long pro-domain with CARD [7] | Inflammasome-mediated autoactivation [6] | Process cytokines; drive pyroptosis [6] |
The molecular structure of caspases directly correlates with their activation mechanisms and functional roles. Initiator caspases (caspase-2, -8, -9, -10) and inflammatory caspases contain long pro-domains featuring protein interaction motifs—either a caspase activation and recruitment domain (CARD) or death effector domains (DED) [3] [2]. These domains facilitate recruitment and activation in multiprotein complexes through homotypic interactions [6]. In contrast, executioner caspases (caspase-3, -6, -7) possess only short pro-domains and depend on cleavage by initiator caspases for their activation [5].
The following diagram illustrates the structural organization of caspase zymogens and their activation mechanisms:
Caspase Structure and Activation Mechanisms
Caspase Activation Cascades and Signaling Pathways
Apoptotic Caspase Activation
Apoptosis, a non-inflammatory form of programmed cell death, proceeds through two principal pathways: the extrinsic (death receptor) pathway and the intrinsic (mitochondrial) pathway [3] [1]. Both pathways converge on the activation of executioner caspases that orchestrate the controlled demolition of cellular components [5].
The extrinsic pathway initiates when extracellular death ligands (e.g., FasL, TRAIL) bind to cell surface death receptors, leading to the formation of the death-inducing signaling complex (DISC) [3]. The DISC recruits and activates initiator caspase-8 (and caspase-10 in humans) through dimerization mediated by death effector domains (DED) [3] [5]. In certain cell types (designated Type I), caspase-8 directly activates executioner caspases; in others (Type II), it connects to the intrinsic pathway through cleavage of the BH3-only protein Bid to tBid, which induces mitochondrial outer membrane permeabilization (MOMP) [5].
The intrinsic pathway activates in response to diverse intracellular stresses including DNA damage, oxidative stress, and growth factor deprivation [3]. These stimuli trigger MOMP, resulting in cytochrome c release from mitochondria [3]. Cytochrome c binds to Apoptotic Protease-Activating Factor 1 (APAF-1), promoting formation of the heptameric apoptosome complex [3] [1]. The apoptosome recruits and activates initiator caspase-9 through CARD-CARD interactions, initiating a caspase cascade that leads to cell death [3].
Once activated, initiator caspases cleave and activate the executioner caspases-3, -6, and -7 [5]. These executioners then cleave hundreds of cellular substrates, resulting in the characteristic morphological changes of apoptosis, including chromatin condensation, DNA fragmentation, membrane blebbing, and formation of apoptotic bodies [5] [1]. Importantly, active executioner caspases can enhance MOMP and activate initiator caspases, forming a positive feedback loop that ensures rapid and complete activation of the apoptotic program [5].
The following diagram illustrates the major caspase activation pathways in apoptosis and pyroptosis:
Caspase Activation Pathways in Cell Death
Inflammatory Caspase Activation
Inflammatory caspases (caspase-1, -4, -5, -11, -12) primarily function in innate immune responses and drive inflammatory forms of cell death, particularly pyroptosis [6] [4]. These caspases are activated through macromolecular complexes known as inflammasomes, which form in response to pathogen-associated molecular patterns (PAMPs) or damage-associated molecular patterns (DAMPs) [6] [2].
The canonical inflammasome pathway involves caspase-1 activation through sensors such as NLRP3, NLRC4, AIM2, or Pyrin [6]. These sensors oligomerize upon ligand binding and recruit the adapter protein ASC, which then recruits and activates caspase-1 through CARD-CARD interactions [6] [2]. Active caspase-1 processes the pro-inflammatory cytokines IL-1β and IL-18 into their mature, bioactive forms and cleaves gasdermin D (GSDMD) [6]. The N-terminal fragment of GSDMD oligomerizes to form pores in the plasma membrane, leading to pyroptosis—a lytic, inflammatory cell death [6] [1].
The non-canonical inflammasome pathway involves caspase-4 and -5 in humans and caspase-11 in mice, which directly recognize intracellular lipopolysaccharide (LPS) from Gram-negative bacteria [6] [2]. This recognition leads to autocatalytic activation and subsequent cleavage of GSDMD, inducing pyroptosis independently of caspase-1 [6]. Additionally, non-canonical caspases can promote NLRP3-dependent caspase-1 activation through potassium efflux resulting from GSDMD pore formation [6].
Experimental Methodologies for Caspase Research
Key Research Reagents and Tools
Table: Essential Research Reagents for Caspase Studies
| Reagent/Category | Specific Examples | Function/Application | Experimental Notes |
|---|---|---|---|
| Caspase Inhibitors | Z-VAD-FMK (pan-caspase) [7], Ac-YVAD-CHO (caspase-1) [7], Ac-DEVD-CHO (caspase-3) [7], Q-VD-OPh (broad-spectrum) [7] | Inhibit caspase activity; determine caspase-specific functions | Q-VD-OPh shows enhanced permeability and reduced toxicity compared to earlier inhibitors [7] |
| Activity Assays | Fluorogenic substrates (e.g., DEVD-AFC for caspase-3) [7], FRET-based caspase sensors [5] | Measure caspase activation kinetics and specificity | FRET sensors enable live-cell imaging of caspase activation dynamics [5] |
| Genetic Models | Caspase knockout mice [3], RNAi/CRISPR-mediated knockdown [1] | Determine physiological functions of specific caspases | Caspase-9 and Apaf-1 knockouts show brain development defects [3] |
| Detection Antibodies | Anti-cleaved caspase-3, anti-active caspase-1, anti-GSDMD [6] [5] | Detect caspase activation and substrate cleavage | Essential for immunohistochemistry and Western blot analysis |
| Cell Death Inducers | Staurosporine (intrinsic pathway) [3], Anti-Fas antibodies (extrinsic pathway) [6], LPS (pyroptosis) [6] | Activate specific cell death pathways | Determine pathway specificity and caspase involvement |
Core Methodological Approaches
Structural Biology Techniques: X-ray crystallography and cryo-electron microscopy have been instrumental in elucidating the atomic structures of caspases and their activation complexes, including the apoptosome and inflammasome [2]. These approaches reveal how caspases interact with their substrates and regulatory proteins, providing insights for targeted drug development [2].
Live-Cell Imaging and FRET Sensors: Fluorescence Resonance Energy Transfer (FRET)-based caspase biosensors allow real-time monitoring of caspase activation kinetics in living cells [5]. These sensors have revealed that once initiated, executioner caspase activation peaks within 15 minutes, demonstrating the rapid, all-or-none nature of apoptotic commitment [5].
Genetic Manipulation Approaches: Gene targeting in mice has been essential for defining the physiological functions of individual caspases [3]. For example, caspase-9-deficient mice exhibit severe brain developmental defects due to reduced apoptosis, while caspase-8 deficiency is embryonic lethal due to impaired endothelial development [3].
The following diagram outlines a generalized experimental workflow for studying caspase functions:
Experimental Workflow for Caspase Research
Therapeutic Implications and Clinical Translation
Caspases represent promising therapeutic targets for a wide spectrum of diseases characterized by dysregulated cell death and inflammation [7]. In neurodegenerative diseases such as Alzheimer's disease, excessive caspase activation contributes to neuronal loss, suggesting that caspase inhibitors might protect against disease progression [4] [7]. Conversely, in cancer, insufficient apoptosis allows tumor survival, suggesting that caspase activators or IAP antagonists could restore cell death sensitivity [4] [7].
The development of caspase-targeted therapies has faced significant challenges, particularly regarding specificity, efficacy, and toxicity [7]. Early peptide-based inhibitors such as Z-VAD-FMK demonstrated poor pharmacokinetics and off-target effects [7]. Second-generation inhibitors including IDN-6556 (emricasan) and VX-740 (pralnacasan) showed promise in clinical trials for liver diseases and rheumatoid arthritis, respectively, but development was halted due to toxicity concerns or inadequate efficacy [7].
Recent advances have identified novel therapeutic opportunities, particularly for inflammatory caspases. Caspase-4/5 inhibitors are being explored for inflammatory bowel disease, hidradenitis suppurativa, and sepsis, as these caspases are uniquely positioned in epithelial and endothelial inflammation [8]. Structural biology approaches have enabled the development of allosteric inhibitors with improved specificity and potency profiles [8].
Emerging research has also revealed that cells can survive transient executioner caspase activation, a phenomenon termed "survival from executioner caspase activation" (SECA) [5]. This survival mechanism has implications for cancer recurrence and tissue regeneration, suggesting more nuanced therapeutic approaches may be needed [5].
The classification of caspases into initiator, executioner, and inflammatory categories provides a fundamental framework for understanding their roles in cell death and inflammation. While this classification system has proven valuable, emerging research reveals substantial crosstalk and multifunctionality between caspase family members, challenging rigid categorical boundaries [2] [9]. The hierarchical caspase activation cascade ensures precise regulation of life-and-death decisions, with executioner caspases serving as the ultimate effectors of apoptotic demolition.
Future research directions include elucidating the structural basis for caspase substrate specificity, understanding context-dependent caspase functions in different cell types, and developing more sophisticated therapeutic strategies that target specific caspases in particular pathological contexts. As understanding of caspase biology continues to evolve, so too will opportunities for therapeutic intervention in the numerous diseases characterized by dysregulated cell death.
Caspases, a family of cysteine-dependent aspartate-specific proteases, function as central regulators of programmed cell death (PCD), inflammation, and innate immunity [1] [10]. These enzymes are synthesized as inactive precursors known as zymogens (or procaspases) that require proteolytic activation to gain their full catalytic function [11] [5]. The structural mechanisms maintaining this latency and the subsequent activation processes represent critical control points in cellular fate decisions, with profound implications for health and disease. Within the context of caspase cascade activation and executioner functions, understanding procaspase structure provides the foundational knowledge required to decipher how cells regulate life-and-death decisions. For drug development professionals, these structural insights offer attractive therapeutic targets for conditions ranging from cancer and neurodegenerative disorders to autoimmune and inflammatory diseases [1] [12]. This review synthesizes current structural knowledge of procaspase zymogens, focusing on the molecular determinants of latency and the domain rearrangements that unleash catalytic potential, thereby framing these insights within the broader landscape of caspase cascade research.
Caspase Classification and Domain Architecture
Caspases are historically categorized based on their primary functions in apoptosis (initiators and executioners) and inflammation, though increasing evidence reveals significant functional overlap [2]. Table 1 summarizes the classification, domain architecture, and activation features of human caspases.
Table 1: Human Caspase Classification and Domain Organization
| Caspase | Primary Classification | Pro-Domain Type | Activation Cleavage Sites | Primary Functions |
|---|---|---|---|---|
| Caspase-1 | Inflammatory | CARD | Multiple aspartic sites | Pyroptosis, IL-1β/IL-18 maturation [11] [10] |
| Caspase-2 | Apoptotic Initiator | CARD | Inter-subunit linker | Cell cycle, DNA damage response, apoptosis [1] |
| Caspase-3 | Apoptotic Executioner | Short (∼30 aa) | Inter-subunit linker | Apoptosis execution, PARP cleavage, substrate proteolysis [5] |
| Caspase-4 | Inflammatory | CARD | Multiple aspartic sites | Non-canonical pyroptosis, GSDMD cleavage [2] |
| Caspase-5 | Inflammatory | CARD | Multiple aspartic sites | Non-canonical pyroptosis, GSDMD cleavage [2] |
| Caspase-6 | Apoptotic Executioner | Short (∼30 aa) | Inter-subunit linker | Apoptosis, lamin cleavage [1] |
| Caspase-7 | Apoptotic Executioner | Short (∼30 aa) | Inter-subunit linker | Apoptosis execution, PARP cleavage [5] |
| Caspase-8 | Apoptotic Initiator | DED | Inter-subunit linker | Extrinsic apoptosis, necroptosis regulation [1] [2] |
| Caspase-9 | Apoptotic Initiator | CARD | Inter-subunit linker | Intrinsic apoptosis, apoptosome formation [1] |
| Caspase-10 | Apoptotic Initiator | DED | Inter-subunit linker | Extrinsic apoptosis [1] |
All caspase zymogens share a conserved tripartite structure consisting of an N-terminal pro-domain, a large catalytic subunit (p20), and a small catalytic subunit (p10) [10] [5]. The pro-domain type represents a key differentiating feature: initiator and inflammatory caspases possess long pro-domains containing protein-protein interaction motifs such as the Caspase Activation and Recruitment Domain (CARD) or Death Effector Domain (DED) that facilitate recruitment to activation platforms [10]. In contrast, executioner caspases typically contain short pro-domains (less than 30 amino acids) without recognizable interaction motifs [5]. The catalytic domain, composed of the large and small subunits, adopts a caspase-hemoglobinase fold that forms the protease core [10].
Figure 1: Domain Architecture of Procaspase Zymogens. Initiator and inflammatory caspases feature long pro-domains (CARD) for recruitment to activation platforms, while executioner caspases have short pro-domains. Both share conserved large (p20) and small (p10) catalytic subunits.
Structural Basis of Zymogen Latency
The latent state of procaspases is maintained through specific structural constraints that prevent unauthorized proteolytic activity. Structural studies have revealed that procaspases exist as stable, inactive monomers or dimers, with their active sites incompletely formed [11]. The catalytic domain of all caspases consists of large and small catalytic subunits that form a caspase-hemoglobinase fold, characterized by a central β-sheet core surrounded by α-helices [10]. In the zymogen state, flexible loops and the inter-domain linker maintain the enzyme in an inactive conformation.
Key to maintaining latency is the arrangement of active site loops. The L1, L2, L3, and L4 loops surrounding the active site adopt orientations that preclude efficient substrate binding and catalysis [11]. Particularly important is the L2 loop (residues 314-316 in caspase-1), which in procaspase-1 occupies the active site cleft, effectively blocking substrate access [11]. This autoinhibitory configuration is stabilized by specific intramolecular interactions that must be disrupted during activation. The crystal structure of the procaspase-1 zymogen domain (solved at 2.05 Å resolution) revealed that although the isolated domain is monomeric in solution, it forms dimers in crystals, providing insight into the first autoproteolytic events during activation by oligomerization [11] [13].
Table 2: Structural Features Maintaining Zymogen Latency in Characterized Procaspases
| Procaspase | Quaternary Structure | Key Latency Features | Activation Trigger |
|---|---|---|---|
| Procaspase-1 | Monomeric (solution) | L2 loop blocks active site; incomplete active site formation | Inflammasome oligomerization [11] |
| Procaspase-7 | Dimeric | Inactive conformation with disordered active site loops | Cleavage by initiator caspases [11] |
| Procaspase-9 | Monomeric | Inactive conformation requiring apoptosome binding | Apoptosome-mediated dimerization [1] |
| DRONC (Drosophila caspase-9 ortholog) | Monomeric | CARD domain inhibits catalytic activity | Dimerization on activation platforms [11] |
For executioner caspases like procaspase-3 and procaspase-7, the zymogens exist as pre-formed dimers but remain catalytically incompetent due to the conformation of the inter-domain linker and active site loops [5]. Proteolytic processing at specific aspartic acid residues within the linker region triggers conformational changes that reorganize the active site into a catalytically competent state. The structural basis for this latency-activation switch varies among caspase subfamilies, reflecting their specialized roles in distinct cell death pathways.
Molecular Mechanisms of Procaspase Activation
Oligomerization-Induced Activation
Initiator and inflammatory caspases undergo activation through induced proximity and oligomerization on specific activation platforms. For inflammatory caspase-1, this occurs through inflammasome formation, where pattern recognition receptors (such as NLRP1 or NLRP3) recruit the adaptor protein ASC and procaspase-1 via CARD-CARD interactions [2]. This recruitment leads to procaspase-1 oligomerization, which facilitates auto-proteolytic cleavage at specific aspartic acid residues [11] [10].
The crystal structure of procaspase-1's zymogen domain revealed critical insights into this process. Although monomeric in solution, the protein formed dimers in crystals, with the loop arrangements in these dimers providing insight into the first autoproteolytic events [11]. Unlike other caspases, autoproteolysis at the second cleavage site (Asp316 in caspase-1) is necessary for conversion to a stable dimer in solution [11] [13]. This dimer stabilization is concurrent with a 130-fold increase in kcat, representing the sole contributing kinetic factor to an activated and efficient inflammatory mediator [11].
Figure 2: Procaspase Activation Pathway. Procaspase zymogens are recruited to activation platforms (1), where oligomerization (2) induces autoproteolytic cleavage (3), generating active caspases that cleave cellular substrates (4).
Proteolytic Activation by Upstream Caspases
Executioner caspases (caspase-3, -6, and -7) are primarily activated through proteolytic cleavage by upstream initiator caspases [5]. These executioner procaspases exist as pre-formed dimers in their zymogen state, with cleavage at specific inter-domain linkers triggering conformational changes that activate the enzyme. For example, initiator caspase-8 (activated by death receptors) or caspase-9 (activated by the apoptosome) cleaves executioner procaspase-3 at specific aspartate residues, resulting in rearrangement of the active site loops into a catalytically competent conformation [5].
This activation mechanism creates a proteolytic cascade that amplifies the initial apoptotic signal, ensuring rapid and efficient dismantling of the cell during apoptosis. Once activated, executioner caspases can process additional procaspase molecules, creating a positive feedback loop that ensures complete commitment to the cell death program [5].
Non-lethal Caspase Activation in Cellular Remodeling
Beyond their roles in cell death, caspases can be activated in sublethal contexts to participate in cellular remodeling and differentiation [14] [5]. In Drosophila olfactory receptor neurons, for example, the executioner caspase Drice is maintained in an inactive proform proximal to cell membrane proteins, including the cell adhesion molecule Fasciclin 3 (Fas3) [14]. This localization restricts caspase activation to specific subcellular compartments, enabling participation in neuronal functional modulation without triggering cell death [14].
This non-lethal activation requires precise regulation of caspase activity through subcellular compartmentalization, interaction with regulatory proteins, and controlled degradation. The identification of caspase-proximal proteins through techniques like TurboID has revealed how caspases are sequestered and regulated in specific cellular locations to facilitate their non-apoptotic functions [14].
Quantitative Analysis of Caspase Activation Parameters
Biochemical studies of caspase activation have yielded quantitative parameters that characterize the transition from zymogen to active enzyme. Table 3 summarizes key kinetic and structural parameters for representative caspases.
Table 3: Quantitative Parameters of Caspase Zymogen Activation
| Caspase | Activation Method | Key Cleavage Sites | Rate Enhancement (kcat increase) | Quaternary Structure Change |
|---|---|---|---|---|
| Caspase-1 | Inflammasome oligomerization | Multiple sites including Asp316 | 130-fold after dimer stabilization [11] | Monomer → Stable dimer [11] |
| Caspase-3 | Cleavage by initiator caspases | Asp175, Asp9, etc. | Not specified in results | Dimer → Active dimer [5] |
| Caspase-7 | Cleavage by initiator caspases | Multiple inter-subunit sites | Not specified in results | Dimer → Active dimer [11] |
| Caspase-9 | Apoptosome-mediated dimerization | Not specified in results | Not specified in results | Monomer → Active dimer [1] |
The activation of caspase zymogens involves significant structural rearrangements that can be quantified through biophysical methods. For procaspase-1, removal of the caspase recruitment domain (CARD) and crystallization of the zymogen domain allowed for detailed structural analysis of the latency mechanism [11]. The structure revealed that proteolysis at Asp316 is necessary for formation of a stable dimer in solution, with dimer stabilization directly correlating with the dramatic increase in catalytic efficiency [11] [13].
Experimental Approaches for Studying Procaspase Structure and Function
Structural Biology Methods
X-ray Crystallography: The crystal structure of procaspase-1's zymogen domain (without its CARD domain) was solved to 2.05 Å resolution, providing atomic-level insight into inflammatory caspase autoactivation [11]. This approach revealed how loop arrangements in the dimer facilitate the first autoproteolytic events during activation by oligomerization.
Cryo-Electron Microscopy (cryo-EM): While not directly applied to procaspases in the available search results, cryo-EM has been used to study related cell death machinery, such as the structure of the apoptotic scramblase Xkr4 [15]. This technique is increasingly valuable for studying large caspase activation complexes like inflammasomes and apoptosomes.
Biochemical and Biophysical Assays
Size Exclusion Chromatography with Multi-Angle Light Scattering (SEC-MALS): This method was used to analyze procaspase-1 C285A processing and dimerization, demonstrating that autoproteolysis at the second cleavage site is necessary for conversion to a stable dimer in solution [11].
TurboID Proximity Labeling: A proximity-dependent biotinylation technique used to identify proteins proximal to executioner caspases in Drosophila brains [14]. This method revealed that the executioner caspase Drice is proximal to cell membrane proteins, including Fasciclin 3, while in its inactive proform.
Fluorescence Resonance Energy Transfer (FRET) Sensors: These sensors enable live monitoring of executioner caspase activation during apoptosis, revealing that once initiated, activation peaks within 15 minutes [5].
Molecular Biology and Protein Engineering
Site-Directed Mutagenesis: Used to validate the functional importance of specific residues in caspase activation. For example, mutation of the catalytic cysteine (C285A) in caspase-1 facilitated structural studies of the zymogen without auto-processing [11].
Recombinant Protein Expression in E. coli: Wild-type human caspase-1 (residues 104-404) and various constructs were cloned into pRSET T7 expression vectors and expressed in BL21Star(DE3) cells for purification and structural studies [11].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Procaspase Studies
| Reagent / Method | Application | Key Features / Function |
|---|---|---|
| pRSET T7 Expression Vector | Recombinant caspase expression | N-terminal Unizyme tag for purification [11] |
| BL21Star(DE3) E. coli cells | Protein expression | Co-transformed with pRARE2 for rare codon supplementation [11] |
| HisTrap HP Column | Protein purification | Immobilized metal affinity chromatography for His-tagged proteins [11] |
| SEC-MALS (Size Exclusion with MALS) | Oligomerization state analysis | Determines molecular weight and oligomeric state in solution [11] |
| TurboID | Proximity-dependent labeling | Identifies proteins proximal to caspases in living cells [14] |
| FRET-based caspase sensors | Live-cell activity monitoring | Real-time detection of caspase activation kinetics [5] |
| Caspase inhibitors (Z-VAD, VX-765) | Functional validation | Pan-caspase inhibitors to confirm caspase-dependent phenotypes [12] |
Implications for Therapeutic Development
The structural insights into procaspase latency and activation have significant implications for therapeutic development across multiple disease areas. Excessive caspase-1 activity drives pathologies in autoimmune and inflammatory diseases such as septic shock, inflammatory bowel disease, familial cold autoinflammatory syndrome, rheumatoid arthritis, and gout [11]. Similarly, dysregulated apoptotic caspases contribute to cancer, neurodegenerative disorders, and ischemic injuries [1] [12].
Understanding the precise molecular mechanisms of zymogen activation has revealed novel targeting strategies beyond active site inhibition. Allosteric inhibitors that prevent procaspase activation by stabilizing the latent conformation represent a promising therapeutic approach [11] [12]. For example, the structural insights from procaspase-1 revealed critical elements of secondary structure that explain why a dimeric protein is favored after proteolysis, suggesting opportunities for dimerization inhibitors [11].
The development of specific caspase inhibitors faces challenges due to conservation among caspase family members, but the unique features of zymogen structures and activation mechanisms offer potential for achieving selectivity. As our structural understanding of procaspases continues to advance, so too will opportunities for therapeutic intervention in the numerous diseases characterized by dysregulated caspase activity.
The structural biology of procaspase zymogens has revealed sophisticated molecular mechanisms that maintain caspase latency and control their activation. Through specific domain architectures, autoinhibitory conformations, and regulated oligomerization, cells precisely control the potent proteolytic activity of caspases until needed. The insights gained from crystal structures, biochemical analyses, and innovative experimental approaches have not only advanced our fundamental understanding of caspase biology but have also opened new avenues for therapeutic intervention in diseases characterized by dysregulated cell death and inflammation. As research continues to elucidate the subtleties of procaspase regulation across different biological contexts and caspase family members, our ability to precisely modulate these pathways for therapeutic benefit will continue to grow, ultimately contributing to improved treatments for cancer, neurodegenerative disorders, autoimmune conditions, and infectious diseases.
Caspases, or cysteine-dependent aspartate-specific proteases, are central regulators of programmed cell death and inflammation [2]. Their activation triggers and executes critical biological processes, most notably apoptosis. A fundamental principle in caspase biology is the existence of a two-tiered cascade where upstream initiator caspases activate downstream executioner caspases [16]. However, these two groups employ fundamentally distinct molecular mechanisms for their activation: initiator caspases are activated through induced proximity-induced dimerization, while executioner caspases require proteolytic cleavage between their large and small subunits [17] [16]. This mechanistic dichotomy represents a sophisticated evolutionary adaptation that ensures precise control over life-and-death cellular decisions. Understanding these distinct activation pathways is essential for researchers investigating basic cell biology mechanisms and drug development professionals targeting caspase pathways in diseases such as cancer, neurodegenerative disorders, and inflammatory conditions [1].
Molecular Mechanisms of Initiator Caspase Activation
The Induced Proximity Model
Initiator caspases (caspase-2, -8, -9, and -10 in humans) exist within healthy cells as inactive monomers [17] [16]. Unlike executioner caspases, their activation does not require proteolytic cleavage. Instead, they are activated through dimerization brought about by their recruitment into specific signaling complexes [17]. This process is described by the "induced proximity" model, which posits that bringing multiple caspase monomers into close proximity drives their activation [17] [16].
The key structural feature enabling this mechanism is the presence of long prodomains in initiator caspases (approximately 150-200 amino acids) that contain protein-protein interaction domains such as death effector domains (DEDs) in caspases-8 and -10, or caspase activation and recruitment domains (CARDs) in caspases-9 and -2 [17] [2] [5]. These domains allow initiator caspases to interact with adapter proteins that dimerize or oligomerize, thereby bringing caspase monomers into close proximity [17].
Table 1: Key Features of Initiator Caspases in Humans
| Caspase | Prodomain Type | Primary Activation Complex | Main Pathway |
|---|---|---|---|
| Caspase-8 | Two DEDs | Death-Inducing Signaling Complex (DISC) | Extrinsic Apoptosis |
| Caspase-9 | CARD | Apoptosome | Intrinsic Apoptosis |
| Caspase-10 | Two DEDs | Death-Inducing Signaling Complex (DISC) | Extrinsic Apoptosis |
| Caspase-2 | CARD | PIDDosome | DNA Damage Response |
Structural Basis of Initiator Caspase Activation
The structural rearrangement during initiator caspase activation is remarkable. In the monomeric state, the catalytic site is not properly formed. Dimerization induces conformational changes that create a functional active site [17]. While cleavage between the large and small subunits is not required for the initial activation step, it does occur subsequently and serves to stabilize the active dimer,
particularly for caspases-2 and -8 [17]. This stabilization is biologically crucial, as non-cleavable mutants of caspase-8 can be activated by dimerization but do not efficiently promote apoptosis [17]. An exception to this rule is caspase-9, whose activity is not stabilized by cleavage but is instead regulated by the apoptosome complex [17].
Figure 1: Initiator Caspase Activation via Induced Proximity. Monomeric initiator caspases are recruited to adapter protein complexes, leading to dimerization and activation through induced proximity.
Molecular Mechanisms of Executioner Caspase Activation
Proteolytic Cleavage as the Activation Trigger
In stark contrast to initiator caspases, executioner caspases (caspase-3, -6, and -7 in humans) preexist in the cytosol of healthy cells as inactive dimers [17] [16] [5]. These zymogens contain only short prodomains (less than 30 amino acids) that lack protein-protein interaction domains [5]. Their activation requires proteolytic cleavage at specific aspartic acid residues located between the large and small subunits [17] [5].
In the inactive procaspase dimer, the catalytic dyads are not properly positioned to access the target aspartate in substrate proteins [17]. Cleavage of the inter-subunit linker allows dramatic conformational changes that snap the two active sites into their functional configuration [17]. Specifically, cleavage liberates the ends of the cleaved linkers, enabling them to interact with the opposite chain and stabilize a structure where the loops comprising the specificity pockets can assume their active positions [17].
Structural Consequences of Cleavage
The structural transformation during executioner caspase activation has been visualized through crystallographic studies of caspase-7 [17]. In the inactive procaspase-7 dimer, the central region is occupied by the linker segments between the large and small subunits. After cleavage, this space becomes available, allowing the "elbow" of the specificity loop to extend into the center of the dimer, thereby forming two functional active sites [17]. Once activated, executioner caspases can process hundreds or thousands of cellular substrates, leading to the characteristic morphological changes of apoptosis, including chromatin condensation, DNA fragmentation, and membrane blebbing [5].
Table 2: Key Features of Executioner Caspases in Humans
| Caspase | Prodomain Length | Primary Activator | Key Substrates |
|---|---|---|---|
| Caspase-3 | Short (<30 aa) | Caspase-8, -9, -10 | PARP, ICAD, USP48 |
| Caspase-7 | Short (<30 aa) | Caspase-8, -9, -10 | PARP, Gasdermins |
| Caspase-6 | Short (<30 aa) | Caspase-3, -7 | Lamin A/C |
Experimental Evidence and Methodologies
Key Experimental Evidence
The distinct activation mechanisms of initiator and executioner caspases have been demonstrated through multiple experimental approaches:
For initiator caspases, recombinant caspase-2, -8, or -9 that lack prodomains are enzymatically inactive when isolated. However, when salt conditions are altered to promote aggregation and dimerization, caspase activity rapidly appears even when cleavage sites between large and small subunits have been mutated [17]. This provides direct evidence that dimerization, not cleavage, drives initial activation. When the aggregating conditions are reversed, cleaved active dimers remain active, whereas uncleavable mutants lose activity, demonstrating the role of cleavage in stabilization rather than activation [17].
For executioner caspases, structural biology approaches have revealed the conformational changes associated with activation. Comparison of procaspase-7 structures before and after cleavage shows how cleavage permits the formation of the functional active site [17]. Biochemical studies demonstrate that executioner caspases can be activated in vitro by initiator caspases or other proteases like granzyme B, which is released by cytotoxic lymphocytes to eliminate virally infected or tumor cells [17].
Detailed Experimental Protocol: Initiator Caspase Dimerization Assay
Purpose: To demonstrate that initiator caspase activation occurs through dimerization rather than proteolytic cleavage.
Methodology:
- Protein Preparation: Express and purify recombinant initiator caspases (e.g., caspase-8) with truncated prodomains in Escherichia coli.
- Mutagenesis: Generate cleavage-site mutants by site-directed mutagenesis, replacing the aspartic acid residue at the cleavage site with alanine or glutamic acid.
- Low-Salt Conditions: Maintain caspases in low-salt buffer (e.g., 50 mM NaCl) to prevent spontaneous aggregation.
- Induced Dimerization: Increase salt concentration to 300-500 mM NaCl to promote caspase aggregation and dimerization.
- Activity Measurement: Monitor caspase activity using fluorogenic substrates (e.g., Ac-IETD-AFC for caspase-8) at excitation/emission wavelengths of 400/505 nm.
- Reversal Test: Gradually decrease salt concentration while continuously monitoring enzyme activity.
- Analysis: Compare activity profiles of wild-type and cleavage-site mutant caspases under different salt conditions.
Expected Results: Both wild-type and cleavage-site mutant caspases show rapid activity increases upon salt-induced dimerization. When salt concentration is decreased, wild-type caspases maintain activity while mutant caspases rapidly lose activity, demonstrating that cleavage stabilizes but does not initiate activity [17].
Detailed Experimental Protocol: Executioner Caspase Cleavage Assay
Purpose: To demonstrate that executioner caspase activation requires proteolytic cleavage between large and small subunits.
Methodology:
- Protein Preparation: Express and purify executioner procaspases (e.g., procaspase-3) as inactive dimers.
- Activation Conditions: Incubate procaspases with:
- Initiator caspases (e.g., active caspase-8 or -9)
- Granzyme B (as a positive control)
- Buffer alone (negative control)
- Cleavage Analysis: Monitor cleavage by:
- Western blotting using antibodies against the large and small subunits
- Size-exclusion chromatography to detect conformational changes
- Activity Assay: Measure caspase activity using fluorogenic substrates (e.g., Ac-DEVD-AFC for caspase-3).
- Mutagenesis: Test cleavage-site mutants to confirm the specificity of activation.
Expected Results: Only cleaved executioner caspases show significant proteolytic activity. Cleavage-site mutants remain inactive even when incubated with initiator caspases, confirming that inter-domain cleavage is essential for activation [17] [5].
Figure 2: The Caspase Activation Cascade. Death stimuli trigger the formation of adapter complexes that dimerize initiator caspases, which then cleave and activate executioner caspases, leading to apoptosis.
Research Reagent Solutions
Table 3: Essential Research Reagents for Caspase Activation Studies
| Reagent Category | Specific Examples | Research Application | Key Features |
|---|---|---|---|
| Fluorogenic Substrates | Ac-DEVD-AFC (Caspase-3), Ac-IETD-AFC (Caspase-8), Ac-LEHD-AFC (Caspase-9) | Activity measurement | Emit fluorescence upon cleavage; specific tetrapeptide recognition sequences |
| Active Recombinant Caspases | Active caspase-3, -8, -9 | In vitro cleavage assays; positive controls | Highly purified; validated activity |
| Caspase Inhibitors | Z-VAD-FMK (pan-caspase), Ac-DEVD-CHO (caspase-3 specific) | Specificity controls; therapeutic exploration | Irreversible (FMK) or reversible (CHO) inhibition mechanisms |
| Antibodies | Anti-cleaved caspase-3, anti-caspase-8, anti-PARP | Western blotting; immunohistochemistry | Detect activation-specific cleavage events |
| Cell Death Inducers | Staurosporine, Fas Ligand, TNF-α | Apoptosis induction in cell culture | Activate intrinsic or extrinsic pathways |
| Caspase Expression Plasmids | Wild-type and mutant constructs | Structure-function studies | Enable site-directed mutagenesis of cleavage sites |
Discussion: Biological Significance and Therapeutic Implications
The evolutionary conservation of distinct activation mechanisms for initiator and executioner caspases highlights their fundamental importance in maintaining precise control over programmed cell death. The induced proximity mechanism for initiator caspases allows the cell to integrate multiple death signals through various adapter proteins, providing signaling specificity [17] [16]. Meanwhile, the cleavage-based activation of executioner caspases creates a crucial amplification step, where a single active initiator caspase can activate numerous executioner caspases, ensuring rapid and complete commitment to cell death once the decision is made [5].
Recent research has revealed surprising complexity in these activation paradigms. For example, caspase-8 demonstrates remarkable functional plasticity, serving as a molecular switch between apoptosis, necroptosis, and pyroptosis depending on cellular context [1]. Additionally, non-apoptotic roles for caspases have been identified in processes such as neuronal function modification, where restricted, subcellular activation of executioner caspases occurs without triggering cell death [14]. In Drosophila olfactory receptor neurons, the executioner caspase Drice is proximal to cell membrane proteins like Fasciclin 3, which facilitates non-lethal caspase activation that modulates neuronal function rather than causing death [14].
From a therapeutic perspective, the distinct activation mechanisms offer unique opportunities for drug development. Targeting initiator caspase dimerization interfaces or their interactions with adapter proteins could provide greater specificity than targeting the conserved active sites of executioner caspases [1] [2]. Furthermore, understanding context-dependent caspase activation is crucial for developing treatments for cancer, neurodegenerative diseases, and inflammatory disorders where caspase regulation is disrupted [1] [18] [2]. For instance, in acute myeloid leukemia (AML), caspase-3 specifically cleaves ubiquitin-specific peptidase 48 (USP48) during drug-induced apoptosis, suggesting potential therapeutic strategies targeting this interaction [18] [19].
The continued elucidation of caspase activation mechanisms thus represents a critical frontier at the intersection of basic cell biology and therapeutic development, with implications for treating a wide spectrum of human diseases.
Apoptosis, a form of programmed cell death (PCD), is a crucial process in multicellular organisms for eliminating unwanted or damaged cells. This genetically controlled cell suicide mechanism is characterized by distinct morphological changes, including cell shrinkage, chromatin condensation, DNA fragmentation, and formation of apoptotic bodies that are rapidly phagocytosed without inducing inflammation [20]. Apoptosis occurs through the activation of a cascade of cysteine proteases known as caspases (cysteine-dependent aspartate-specific proteases), which cleave their substrates after aspartic acid residues [2] [21]. These enzymes serve as the central executioners of apoptotic cell death, systematically dismantling cellular structures through the cleavage of key protein substrates [1] [5].
The caspase family is broadly categorized into initiator and executioner caspases based on their position in the proteolytic cascade. Initiator caspases (caspase-2, -8, -9, -10) contain long pro-domains that enable them to respond to proximal apoptotic signals, while executioner caspases (caspase-3, -6, -7) possess short pro-domains and function downstream to directly mediate the terminal events of cell death [2] [5]. Activation of initiator caspases occurs through induced proximity at specific signaling platforms, whereas executioner caspases are activated through proteolytic cleavage by initiator caspases [22]. Once activated, executioner caspases cleave hundreds of cellular substrates, including structural proteins, DNA repair enzymes, and cell cycle regulators, leading to the characteristic biochemical and morphological hallmarks of apoptosis [5].
Table 1: Major Caspases in Apoptotic Pathways
| Caspase | Type | Primary Pathway | Key Functions and Substrates |
|---|---|---|---|
| Caspase-8 | Initiator | Extrinsic | Initiates extrinsic pathway; cleaves Bid, caspase-3, -6, -7 [1] [5] |
| Caspase-9 | Initiator | Intrinsic | Activated by apoptosome; cleaves caspase-3, -7 [2] [5] |
| Caspase-10 | Initiator | Extrinsic | Death receptor-mediated apoptosis; regulates caspase-8 [1] |
| Caspase-2 | Initiator | Intrinsic | DNA damage response; cleaves Bid [1] |
| Caspase-3 | Executioner | Both | Primary executioner; cleaves PARP, lamins, ICAD; activates GSDME [1] [2] [5] |
| Caspase-7 | Executioner | Both | Cleaves PARP; suppresses pyroptosis via GSDMD cleavage [1] [5] |
| Caspase-6 | Executioner | Both | Activates caspase-8; lamin cleavage [1] [5] |
This technical guide provides an in-depth analysis of the three principal apoptotic pathways—extrinsic, intrinsic, and granzyme B—focusing on their molecular mechanisms, regulatory networks, and experimental approaches for studying caspase cascade activation and executioner functions.
The Extrinsic Apoptotic Pathway
Molecular Mechanism
The extrinsic pathway, also known as the death receptor pathway, is initiated by the binding of extracellular death ligands to their corresponding cell surface death receptors. This pathway is primarily involved in eliminating cells in response to external signals, particularly in immune regulation and host defense [2]. Key death receptors include TNF receptor 1 (TNFR1), Fas (CD95), and TRAIL receptors (DR4 and DR5), which belong to the TNF receptor superfamily [20].
Upon ligand binding, death receptors undergo trimerization and conformational changes that enable the recruitment of adapter proteins through homotypic interactions between death domains (DD). For instance, Fas-associated death domain (FADD) is recruited to the activated Fas receptor, forming the death-inducing signaling complex (DISC) [2] [5]. The DISC then recruits initiator caspases, primarily caspase-8 and caspase-10, through interactions between death effector domains (DED), leading to their dimerization and activation [22] [2]. Once activated, caspase-8 directly cleaves and activates executioner caspases-3, -6, and -7, initiating the apoptotic execution phase [5].
Diagram 1: Extrinsic Apoptotic Pathway Activation via Death Receptors
Regulatory Networks and Crosstalk
The extrinsic pathway exhibits sophisticated regulatory mechanisms that determine cellular fate. A key regulatory molecule is cellular FLICE-inhibitory protein (c-FLIP), which structurally resembles caspase-8 but lacks proteolytic activity. c-FLIP competes with caspase-8 for binding to FADD at the DISC, thereby modulating caspase-8 activation [20]. Additionally, caspase-8-mediated cleavage of the Bcl-2 family protein Bid generates truncated Bid (tBid), which translocates to mitochondria and activates the intrinsic apoptotic pathway, creating a crucial amplification loop [5] [23].
The classification of cells into type I and type II based on their apoptotic signaling reflects this crosstalk. In type I cells, robust caspase-8 activation at the DISC directly activates executioner caspases sufficiently to induce apoptosis without mitochondrial amplification. In contrast, type II cells require caspase-8-mediated Bid cleavage and mitochondrial outer membrane permeabilization (MOMP) to fully activate the apoptotic cascade [22] [5]. This classification has important implications for cancer therapy resistance, as many cancer cells evolve toward type II signaling to evade death receptor-mediated apoptosis.
Experimental Analysis of Extrinsic Pathway
Live-cell imaging using FRET-based reporters has revealed the dynamic regulation of caspase activation in the extrinsic pathway. Specifically, caspase-8 activity is detected during the prolonged delay that precedes MOMP and effector caspase activation [22]. Experimental perturbation studies demonstrate that XIAP and proteasome-dependent degradation of effector caspases serve as critical restraints during this pre-MOMP period [22].
Table 2: Key Experiments in Extrinsic Pathway Analysis
| Experimental Approach | Methodology | Key Findings |
|---|---|---|
| Live-cell caspase activity monitoring | FRET-based reporters (IC-RP for initiator, EC-RP for effector caspases) | Initiator caspases active during variable delay before MOMP; effector activation is rapid (<15 min) [22] |
| DISC immunoprecipitation | Co-immunoprecipitation of FADD, caspase-8 from death receptor complexes | Identified composition and regulation of primary signaling complex [2] [5] |
| Type I/II cell classification | Caspase inhibition, Bid knockout, mitochondrial function assessment | Revealed mitochondrial amplification requirement in type II cells [22] [5] |
| Mathematical modeling | ODE-based models of caspase activation dynamics | Identified XIAP and proteasomal degradation as key regulators delaying effector activation [22] [23] |
The Intrinsic Apoptotic Pathway
Molecular Mechanism
The intrinsic pathway, also known as the mitochondrial pathway, is initiated in response to intracellular stress signals, including DNA damage, oxidative stress, growth factor withdrawal, and endoplasmic reticulum stress [23] [20]. These signals converge on mitochondria, leading to mitochondrial outer membrane permeabilization (MOMP), which represents a commitment point to cell death [23].
The Bcl-2 protein family serves as the central regulator of MOMP, comprising three functional subgroups: (1) Pro-apoptotic effector proteins (Bax and Bak) that directly mediate MOMP; (2) Anti-apoptotic proteins (Bcl-2, Bcl-xL, Mcl-1) that inhibit Bax/Bak activation; and (3) BH3-only proteins (Bid, Bim, Puma, Bad, Noxa) that sense cellular stress and regulate the balance between pro- and anti-apoptotic members [23]. In response to stress signals, activator BH3-only proteins (Bim, Bid, Puma) directly engage and activate Bax and Bak, while sensitizer BH3-only proteins (Bad, Noxa) neutralize anti-apoptotic Bcl-2 proteins [23].
Upon activation, Bax and Bak undergo conformational changes and oligomerize to form pores in the mitochondrial outer membrane, leading to the release of cytochrome c and other pro-apoptotic factors from the mitochondrial intermembrane space [23] [20]. Cytochrome c then binds to Apaf-1 in the cytosol, promoting ATP-dependent oligomerization into a wheel-like signaling platform known as the apoptosome. The apoptosome recruits and activates initiator caspase-9, which subsequently cleaves and activates executioner caspases-3 and -7 [2] [20].
Diagram 2: Intrinsic Apoptotic Pathway via Mitochondrial Signaling
Regulatory Networks and Amplification Loops
The intrinsic pathway features multiple regulatory checkpoints and amplification mechanisms that ensure precise control over cell fate decisions. Anti-apoptotic Bcl-2 proteins preserve mitochondrial integrity by sequestering activator BH3-only proteins and directly inhibiting Bax/Bak activation [23]. The balance between pro- and anti-apoptotic Bcl-2 family members functions as a rheostat for cellular susceptibility to apoptosis.
Following MOMP, additional mitochondrial proteins are released that modulate apoptosis. Second mitochondria-derived activator of caspases (Smac/DIABLO) neutralizes inhibitor of apoptosis proteins (IAPs), particularly XIAP, which would otherwise inhibit caspase-3, -7, and -9 activity [23] [20]. Simultaneously, Omi/HtrA2 serine protease also antagonizes IAPs and promotes apoptosis. This coordinated release of pro-apoptotic factors ensures efficient caspase activation following MOMP.
A critical positive feedback loop exists between executioner caspases and the intrinsic pathway. Active caspase-3 cleaves various substrates, including the anti-apoptotic protein Bcl-2, converting it into a pro-apoptotic fragment that further promotes MOMP [5]. Additionally, caspase-3-mediated activation of caspase-6 can generate additional caspase-8 through a feedback loop, further amplifying the apoptotic signal [22].
Experimental Analysis of Intrinsic Pathway
Mathematical modeling of Bcl-2 family interactions has revealed that MOMP operates as a rapid, switch-like response that is robust to variability in protein expression levels [23]. This switch-like behavior arises from the complex interplay of activation and inhibition within the Bcl-2 protein network.
Single-cell analysis using IMS-RP (intermembrane space reporter protein) has demonstrated that MOMP is completed within less than 5 minutes, though stimulus-specific differences in kinetics become apparent at second-scale resolution [22]. The release of mitochondrial proteins occurs as a sudden, all-or-none event at the single-cell level, explaining the commitment point characteristic of intrinsic apoptosis.
BH3 profiling represents a functional experimental approach to assess mitochondrial priming and apoptotic susceptibility by measuring the response of mitochondria to specific BH3-only peptides [23]. This technique has proven valuable for predicting cancer cell responses to chemotherapeutic agents and for identifying dependencies on specific anti-apoptotic Bcl-2 family members for survival.
The Granzyme B Pathway
Molecular Mechanism
The granzyme B pathway represents a crucial mechanism for immune-mediated elimination of virus-infected and cancerous cells by cytotoxic T lymphocytes (CTLs) and natural killer (NK) cells. This pathway bridges innate and adaptive immunity by enabling immune cells to directly induce apoptosis in target cells [2]. Granzyme B is a serine protease stored in the granules of cytotoxic lymphocytes and is delivered to target cells through perforin-mediated pores or receptor-mediated endocytosis.
Upon delivery into the target cell cytoplasm, granzyme B cleaves and activates multiple apoptotic substrates, functioning similarly to both initiator and executioner caspases. Granzyme B directly cleaves caspase-3, -6, -7, -8, and -10, bypassing the need for upstream signaling complexes and rapidly initiating the apoptotic cascade [2]. Additionally, granzyme B cleaves the BH3-only protein Bid to generate truncated Bid (tBid), which translocates to mitochondria and induces MOMP, thereby engaging the intrinsic pathway for signal amplification [5].
Beyond caspase activation, granzyme B directly cleaves key apoptotic substrates, including ICAD (inhibitor of caspase-activated DNase), leading to DNA fragmentation, and PARP [poly(ADP-ribose) polymerase], disrupting DNA repair mechanisms [2]. This multi-pronged approach ensures rapid and efficient destruction of target cells before viral replication or defensive responses can occur.
Regulatory Networks and Immune Surveillance
The granzyme B pathway operates under tight regulatory control to prevent inappropriate immune-mediated cell killing. Serpins (serine protease inhibitors), particularly proteinase inhibitor 9 (PI-9) in humans, inhibit granzyme B activity and protect cytotoxic lymphocytes from self-destruction [2]. The expression of PI-9 in certain tissues may provide protection against immune-mediated damage, while its upregulation in cancer cells represents a mechanism of immune evasion.
The efficiency of granzyme B-mediated apoptosis is influenced by the expression of IAP family proteins in target cells. XIAP directly inhibits caspase-3 and -7, potentially resisting granzyme B-induced apoptosis [5]. However, granzyme B can circumvent this inhibition through multiple mechanisms, including direct caspase processing and Bid-mediated MOMP leading to Smac/DIABLO release, which neutralizes XIAP [2] [20].
Experimental Analysis of Granzyme B Pathway
Studies utilizing granzyme B-deficient mice have revealed its essential role in controlling viral infections and tumor surveillance. These models demonstrate that while other granzymes (particularly granzyme A) can partially compensate, granzyme B is uniquely efficient at inducing rapid apoptosis in target cells [2].
In vitro reconstitution assays using purified granzyme B and perforin have been instrumental for identifying direct substrates and deciphering the hierarchy of apoptotic events. These studies confirmed that granzyme B can directly process executioner caspases-3 and -7, as well as initiate mitochondrial amplification through Bid cleavage [2].
Live-cell imaging of granzyme B-mediated killing has revealed remarkably rapid kinetics, with target cells displaying apoptotic morphology within minutes of exposure to activated cytotoxic lymphocytes. This rapid induction reflects the direct activation of executioner mechanisms without the need for complex upstream signaling events [2].
Execution Phase: Caspase Activation and Substrate Cleavage
Molecular Mechanisms of Caspase Activation
The execution phase of apoptosis represents the final common pathway where activated executioner caspases systematically dismantle cellular structures. Executioner caspases-3, -6, and -7 exist as inactive dimers (zymogens) in healthy cells, requiring proteolytic cleavage by initiator caspases for activation [5]. Cleavage occurs at specific aspartic acid residues, separating the pro-domain and generating separate large and small subunits that reassemble to form the active enzyme [21] [5].
Once activated, executioner caspases exhibit a >100-fold increase in proteolytic activity and function as the primary effectors of apoptotic cell death [22]. Caspase-3 serves as the major executioner caspase, with caspase-7 sharing overlapping substrates and functions. Caspase-6 has distinct substrates and additionally functions in feedback amplification by processing caspase-8 [1] [5]. The activation of executioner caspases follows an "all-or-none" pattern at the single-cell level, with activation peaking within 15 minutes of initiation [5].
Apoptotic Substrate Cleavage and Morphological Changes
Executioner caspases target hundreds of cellular proteins for limited proteolysis, resulting in the characteristic morphological and biochemical hallmarks of apoptosis [5]. Key substrate categories include:
- Nuclear proteins: Cleavage of ICAD (inhibitor of caspase-activated DNase) releases CAD, which executes DNA fragmentation between nucleosomes, creating the characteristic DNA ladder. Lamin cleavage disrupts the nuclear envelope, contributing to nuclear shrinkage and fragmentation [5] [20].
- Cytoskeletal proteins: Cleavage of cytoskeletal components (actin, fodrin, gelsolin) and regulatory proteins (FAK, p21-activated kinase 2) mediates membrane blebbing and cell shrinkage [5].
- DNA repair enzymes: Cleavage of PARP prevents DNA repair while conserving cellular ATP for the apoptotic process [21] [5].
- Cell cycle regulators: Cleavage of various cell cycle proteins ensures termination of proliferative signaling [5].
- Anti-apoptotic proteins: Cleavage of Bcl-2, Bcl-xL, and IAPs converts them into pro-apoptotic fragments, creating positive feedback loops that amplify the death signal [5].
Table 3: Key Executioner Caspase Substrates and Functions
| Substrate | Caspase | Functional Consequence of Cleavage |
|---|---|---|
| PARP | Caspase-3, -7 | Inactivates DNA repair; conserves ATP [21] [5] |
| ICAD | Caspase-3 | Releases CAD nuclease for DNA fragmentation [5] |
| Lamin A/C | Caspase-6 | Nuclear envelope disintegration [5] |
| GSDME | Caspase-3 | Generates N-terminal fragment that induces pyroptosis [1] [2] |
| Bcl-2 | Caspase-3 | Converts anti-apoptotic protein to pro-apoptotic form [5] |
| FAK | Caspase-3, -6 | Disrupts focal adhesions; contributes to cell detachment [5] |
| Rho-associated kinase | Caspase-3 | Regulates membrane blebbing [5] |
Alternative Cell Death Outcomes
Emerging evidence indicates that executioner caspase activation does not invariably lead to cell death. Cells can survive sublethal caspase activation through a process called anastasis, particularly in response to transient or low-intensity stress [5]. Survival from executioner caspase activation (SECA) has been documented in both physiological contexts (e.g., developmental processes) and pathological conditions (e.g., cancer therapy resistance) [5].
The consequences of SECA depend on cellular context and stress intensity. In some scenarios, SECA contributes to tissue regeneration and recovery, while in others it promotes genomic instability and oncogenesis due to incomplete DNA fragmentation and repair [5]. Cancer cells that survive caspase activation often exhibit enhanced stem cell-like properties and increased aggressiveness, representing a potential mechanism of therapy resistance [5].
Research Methods and Applications
Experimental Approaches for Apoptosis Detection
Advanced methodologies have been developed to detect and quantify apoptosis in real-time, providing insights into the dynamics of caspase activation and execution. Key technologies include:
- Fluorescence resonance energy transfer (FRET) reporters: Engineered constructs containing caspase cleavage sites between fluorophore pairs that exhibit FRET signal loss upon cleavage, enabling real-time monitoring of caspase activity in live cells [22].
- Annexin V staining: Detects phosphatidylserine externalization on the outer leaflet of the plasma membrane, an early event in apoptosis [24].
- Mitochondrial membrane potential sensors: Dyes like JC-1 and TMRM that detect the collapse of mitochondrial membrane potential associated with MOMP [22].
- IAP-based reporters: Constructs that monitor IAP activity or Smac release from mitochondria [22].
- High-throughput flow cytometry: Enables multiparameter analysis of apoptotic markers across large cell populations with single-cell resolution [24].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Apoptosis Studies
| Reagent/Category | Specific Examples | Function and Application |
|---|---|---|
| Caspase Activity Assays | Fluorogenic substrates (DEVD-AMC for caspase-3, IETD-AFC for caspase-8) | Quantitative measurement of specific caspase activities in cell lysates [21] [22] |
| Apoptosis Detection Kits | Annexin V-FITC/PI staining kits | Differentiation of live, early apoptotic, late apoptotic, and necrotic cells by flow cytometry [24] |
| Live-Cell Reporters | FRET-based caspase reporters (EC-RP, IC-RP), IMS-RP | Real-time monitoring of caspase activation and MOMP in living cells [22] |
| Caspase Inhibitors | Z-VAD-FMK (pan-caspase), Z-DEVD-FMK (caspase-3) | Pharmacological inhibition to establish caspase-dependence of cell death [21] |
| Antibodies for Western Blot | Anti-cleaved caspase-3, anti-PARP, anti-cytochrome c | Detection of specific proteolytic events and protein relocalization [22] [24] |
| BH3 Profiling Peptides | BIM, BAD, HRK-derived peptides | Functional assessment of mitochondrial priming and Bcl-2 family dependencies [23] |
Therapeutic Applications and Drug Development
The understanding of apoptotic pathways has enabled the development of targeted therapies, particularly for cancer treatment. Several therapeutic classes have emerged:
- BH3 mimetics: Small molecules (e.g., venetoclax/ABT-199) that specifically inhibit anti-apoptotic Bcl-2 proteins, promoting MOMP and apoptosis in cancer cells [23] [25].
- IAP antagonists: Compounds that mimic Smac/DIABLO to neutralize IAP-mediated caspase inhibition, sensitizing cells to apoptosis [23] [25].
- Death receptor agonists: Monoclonal antibodies that activate death receptors (e.g., TRAIL receptor agonists) to directly engage the extrinsic pathway [25].
- Caspase activators: Experimental compounds that directly promote caspase activation, though clinical development has proven challenging due to toxicity concerns [25].
The global apoptosis assay market, valued at USD 6.5 billion in 2024 and projected to reach USD 14.6 billion by 2034, reflects the growing importance of apoptosis research in drug discovery and development [24]. Technological advances including high-content screening, 3D cell culture compatibility, and AI-powered image analysis are enhancing the precision and throughput of apoptosis detection in both research and clinical applications [24].
Diagram 3: Apoptosis Research Applications and Therapeutic Development
The extrinsic, intrinsic, and granzyme B apoptotic pathways represent sophisticated molecular cascades that converge on caspase activation to execute programmed cell death. While each pathway initiates through distinct mechanisms—death receptor engagement, mitochondrial stress signaling, or immune-mediated protease delivery—they share common executioner caspases that systematically dismantle cellular structures through limited proteolysis of key substrates.
Recent advances in live-cell imaging, mathematical modeling, and single-cell analysis have revealed the dynamic regulation and systems-level properties of apoptotic signaling networks. The discovery of alternative cell fate outcomes, including survival from executioner caspase activation and non-apoptotic caspase functions, has added complexity to our understanding of these pathways. Furthermore, the crosstalk between apoptotic and other forms of regulated cell death, such as pyroptosis and necroptosis, highlights the integrated nature of cell death control [1] [2].
Ongoing research continues to elucidate the structural basis of caspase activation and substrate recognition, the systems-level properties emerging from protein interaction networks, and the therapeutic potential of modulating apoptotic pathways for cancer and other diseases. As detection technologies advance and our molecular understanding deepens, the manipulation of apoptotic pathways represents a promising frontier for targeted therapeutic interventions across a spectrum of human diseases.
Executioner caspases-3, -6, and -7 function as terminal effectors in the caspase cascade, responsible for the precise proteolytic cleavage of hundreds of cellular substrates to orchestrate apoptotic cell death. Their coordinated activity leads to the characteristic morphological changes of apoptosis, including DNA fragmentation, membrane blebbing, and formation of apoptotic bodies. Recent research has expanded their known substrate repertoire and revealed context-specific functions beyond core apoptosis. This whitepaper comprehensively details the validated substrate profiles, cleavage motifs, experimental methodologies for identification, and functional consequences of executioner caspase activity, providing a foundational resource for researchers investigating caspase biology and therapeutic applications.
Within the hierarchical framework of apoptotic signaling, executioner caspases-3, -6, and -7 occupy the terminal position, responsible for implementing the controlled demolition of cellular structures. Caspases (cysteine-aspartic proteases) are a family of proteases that cleave their substrates after specific aspartic acid residues within short tetrapeptide motifs [4]. The apoptotic caspase cascade is initiated by upstream signaling events that activate initiator caspases (such as caspase-8, -9, and -10), which subsequently cleave and activate the downstream executioner caspases-3, -6, and -7 [3] [5]. This amplification mechanism ensures rapid and irreversible commitment to cell death once the threshold for activation is surpassed.
Executioner caspases are synthesized as inactive zymogens (pro-caspases) that exist as dimers in healthy cells. They contain a short pro-domain (less than 30 amino acids) compared to the long pro-domains of initiator caspases [5]. Activation occurs through cleavage by initiator caspases at specific aspartic residues between the large and small subunits, resulting in conformational changes that form the active enzyme, typically a heterotetramer composed of two large and two small subunits [21] [3]. Once activated, a single executioner caspase can cleave and activate other executioner caspases, establishing an accelerated feedback loop that ensures complete activation [3].
The functional repertoire of executioner caspases extends beyond their classical role in apoptosis. Emerging evidence indicates that sublethal activation of these enzymes participates in diverse physiological processes including cellular differentiation, synaptic plasticity, and innate immunity [26]. This whitepaper focuses specifically on their canonical function as executioners of cell death, framing their substrate repertoire within the context of caspase cascade activation and the systematic dismantling of cellular architecture.
Substrate Repertoire of Executioner Caspases
Executioner caspases recognize and cleave a diverse array of cellular proteins, with current estimates exceeding 600 identified substrates [4]. The specific cleavage events disrupt key cellular processes and structures, leading to the orderly disintegration characteristic of apoptosis. While caspase-3 serves as the primary executioner with the broadest substrate profile, caspases-6 and -7 contribute complementary and unique cleavage activities.
Table 1: Key Validated Substrates of Executioner Caspases
| Substrate Category | Specific Substrate | Cleaving Caspase | Functional Consequence of Cleavage |
|---|---|---|---|
| DNA Repair & Maintenance | PARP (Poly(ADP-ribose) polymerase) | Caspase-3, -7 [27] | Inactivates DNA repair, conserves cellular ATP [27] |
| ICAD/DFF45 (DNA fragmentation factor) | Caspase-3 [5] | Releases CAD nuclease, enables DNA fragmentation [5] | |
| Nuclear Integrity | Lamin A | Caspase-6 [27] | Disassembles nuclear lamina [27] |
| Cytoskeletal Organization | α-Fodrin | Caspase-3 [28] | Disrupts membrane cytoskeleton, contributes to blebbing [28] |
| Gelsolin | Caspase-3 [5] | Generates active fragment that severs actin, aiding disassembly [5] | |
| Apoptosis Regulation | Beclin 1 | Caspase-3 [29] | Inactivates autophagy, promotes apoptosis [29] |
| USP48 (Ubiquitin-specific peptidase 48) | Caspase-3 [18] | Enhances drug-induced apoptosis in AML [18] | |
| Inflammatory Signaling | GSDME (Gasdermin E) | Caspase-3 [27] | Can induce secondary pyroptosis [27] |
| GSDMD (Gasdermin D) | Caspase-3, -7 [27] | Non-canonical cleavage at D87 suppresses pyroptosis [27] |
Caspase-3: The Primary Executioner
Caspase-3 possesses the most extensive substrate profile among the executioners and is often considered the primary effector of apoptotic morphology. Its activation is characterized by an "all-or-none" pattern, typically peaking within 15 minutes of initiation [5]. Caspase-3 recognizes the DEVD (Asp-Glu-Val-Asp) tetrapeptide motif, which forms the basis for many activity assays and inhibitors [28].
Key cleavage events mediated by caspase-3 include:
- Inactivation of DNA repair machinery through cleavage of PARP, preventing futile repair attempts and conserving cellular ATP for the apoptotic process [27].
- Activation of DNA fragmentation by cleaving ICAD/DFF45, which releases the CAD nuclease to execute internucleosomal DNA cleavage [5].
- Disruption of cytoskeletal integrity through cleavage of α-fodrin, gelsolin, and other structural proteins, leading to membrane blebbing and loss of cell shape [28] [5].
- Regulation of cross-talk between cell death pathways by cleaving Beclin 1 to inhibit autophagy and promote apoptosis [29], and processing gasdermin proteins which can modulate pyroptosis [27].
A recent 2025 study identified USP48 as a novel caspase-3 substrate, demonstrating cleavage at a specific DEQD motif (611-614) during drug-induced apoptosis in Acute Myeloid Leukemia (AML). This cleavage generates an N-terminal fragment that is destabilized, and knockdown experiments confirmed that USP48 inhibition promotes apoptosis and enhances chemotherapy efficacy, highlighting its potential as a therapeutic target [18].
Caspase-7: A Collaborator with Distinct Roles
Caspase-7 shares significant structural homology with caspase-3 and overlaps in some substrate specificities, including PARP cleavage [27]. However, emerging evidence reveals non-redundant functions. Caspase-7 plays a particularly important role in suppressing pyroptosis through non-canonical cleavage of GSDMD at Asp87, which prevents its oligomerization and pore-forming activity [27]. This illustrates how executioner caspases can actively inhibit alternative cell death pathways to ensure an immunologically silent apoptotic demise.
Caspase-6: The Laminase and Beyond
Caspase-6 exhibits a more restricted substrate profile but performs critical specialized functions. It is historically known as the primary laminase, responsible for cleaving nuclear lamin proteins to facilitate nuclear envelope disassembly [27]. Beyond this role, caspase-6 can activate caspase-8, creating a feedback amplification loop that enhances the apoptotic signal [27]. It also regulates GSDMB-mediated pyroptosis, further highlighting the complex interplay between different cell death modalities [27].
Table 2: Characteristic Cleavage Motifs and Activation Patterns
| Executioner Caspase | Characteristic Recognition Motif | Activation Mechanism | Temporal Activation Pattern |
|---|---|---|---|
| Caspase-3 | DEVD [28] | Cleavage by initiator caspases (8, 9, 10) [3] | Rapid, "all-or-none" peak within 15 min [5] |
| Caspase-6 | VEHD [27] | Cleavage by caspase-3, -7, -8 [27] | Delayed relative to caspase-3 [27] |
| Caspase-7 | DEVD [27] | Cleavage by initiator caspases [3] | Simultaneous or slightly delayed versus caspase-3 [5] |
Experimental Methodologies for Analyzing Executioner Caspase Activity
A diverse toolkit of biochemical, imaging, and proteomic approaches enables researchers to detect executioner caspase activation and identify novel substrates. The selection of appropriate methodologies depends on the specific research question, ranging from single-cell temporal dynamics to system-wide substrate identification.
Fluorescence-Based Detection Methods
Fluorescence Resonance Energy Transfer (FRET) sensors provide real-time, single-cell resolution monitoring of caspase activation dynamics. These genetically encoded reporters typically consist of two fluorescent proteins (e.g., CFP and YFP) linked by a short peptide containing the caspase-specific cleavage motif (e.g., DEVD for caspase-3). Upon cleavage, the separation of the fluorophores alters the FRET efficiency, allowing quantitative kinetic analysis [5]. This approach revealed that executioner caspase activation, once initiated, follows a rapid, switch-like behavior peaking within 15 minutes [5].
Surface Plasmon Resonance (SPR) imaging offers a label-free alternative for monitoring caspase activity. In one described platform, a chimeric GST:DEVD:EGFP fusion protein is immobilized on a chip surface. Caspase-3 cleavage at the DEVD sequence alters the surface properties, detectable as a change in the refractive index, allowing sensitive and quantitative activity measurements [28].
Proteomic Approaches for Substrate Identification
Systematic identification of caspase substrates requires proteomic strategies:
- Western Blot Analysis: The foundational method for detecting substrate cleavage by observing characteristic proteolytic fragments and their dependence on caspase activity, often using pan-caspase inhibitors like Z-VAD-fmk or caspase-specific inhibitors [29].
- Mass Spectrometry (MS)-Based Proteomics: Modern approaches involve comparing protein profiles from apoptotic versus normal cells, often coupled with enrichment strategies for neo-N-terminal peptides generated by caspase cleavage. This allows unbiased, global mapping of the caspase substrate repertoire.
Functional Validation Experiments
Following the identification of potential substrates, rigorous validation is required:
- In Vitro Cleavage Assays: Incubating recombinant candidate substrates with active recombinant caspases to confirm direct cleavage.
- Site-Directed Mutagenesis: Mutating the predicted P1 aspartic acid residue to alanine to abrogate cleavage, providing definitive evidence for a specific cleavage site.
- Cellular Knockdown/Knockout: Utilizing siRNA, shRNA [18], or CRISPR-Cas9 to deplete the target protein and assess the functional impact on apoptotic phenotypes, as demonstrated in the USP48 study [18].
Research Reagent Solutions Toolkit
Table 3: Essential Reagents for Executioner Caspase Research
| Reagent Category | Specific Example | Research Application | Key Function |
|---|---|---|---|
| Caspase Inhibitors | Z-VAD-fmk (pan-caspase) [29] | Inhibiting caspase activity broadly | Irreversible inhibitor, confirms caspase-dependent processes |
| Z-DEVD-fmk (caspase-3/7 specific) | Specific caspase-3/7 inhibition | Validating involvement of specific executioners | |
| Activity Assays | Fluorogenic substrates (e.g., Ac-DEVD-AFC) | Quantifying enzymatic activity | Releases fluorescent AFC upon cleavage |
| FRET-based biosensors (e.g., CFP-DEVD-YFP) [5] | Live-cell imaging of activation kinetics | Real-time, single-cell dynamics | |
| Detection Antibodies | Anti-cleaved caspase-3 | IHC, WB detection of active caspase | Marker for apoptotic cells in tissues and lysates |
| Anti-PARP (cleaved) | WB detection of caspase activity | Validated readout for executioner caspase function | |
| Anti-cleaved Lamin A | WB detection of caspase-6 activity | Specific marker for caspase-6 function | |
| Expression Plasmids | pGST:DEVD:EGFP [28] | SPR-based activity sensing | Immobilized substrate for biosensor applications |
| Mutant substrates (D→A) | Cleavage site validation | Confirming specific cleavage residues |
Visualization of Executioner Caspase Pathways and Assays
Executioner Caspase Activation Pathway
Diagram 1: Executioner caspase activation and feedback.
Substrate Cleavage and Functional Consequences
Diagram 2: Key substrates and cleavage outcomes.
Experimental Workflow for Substrate Identification
Diagram 3: Substrate identification and validation workflow.
The executioner caspases-3, -6, and -7 represent the terminal effectors in the apoptotic cascade, coordinating the systematic dismantling of cellular structures through precisely targeted proteolysis. While they share common activation mechanisms and some functional redundancy, each possesses a unique substrate repertoire that contributes to the overall efficiency and completeness of apoptotic cell death. The expanding catalog of validated substrates, including recently identified targets like USP48, continues to reveal novel regulatory networks and potential therapeutic targets, particularly in oncology.
Future research directions will likely focus on quantifying the kinetic parameters of specific cleavage events, understanding the functional significance of non-apoptotic roles at sublethal activation levels, and exploiting the unique substrate specificities of these enzymes for targeted therapeutic interventions. The experimental methodologies and reagents detailed in this whitepaper provide the essential toolkit for advancing these investigations, offering researchers multiple entry points for probing the complex functions of these critical mediators of cell fate.
From Bench to Bedside: Techniques and Therapeutic Applications in Caspase Research
Caspases, a family of cysteine-aspartate proteases, serve as master regulators of programmed cell death (PCD), critically balancing cellular survival and death. These enzymes coordinate multiple cell death pathways, including apoptosis, pyroptosis, and necroptosis, through intricate proteolytic cascades [1] [27]. Research utilizing caspase-deficient models has revealed that their functions extend beyond cell death execution to encompass roles in inflammation, innate immunity, cellular homeostasis, and tissue regeneration [30] [2]. The strategic application of caspase-deficient mice and cell lines has become indispensable for dissecting the complexity of caspase networks, revealing unexpected redundancies, feedback mechanisms, and non-apoptotic functions. This technical guide synthesizes current methodologies and findings from caspase manipulation studies, providing researchers with a framework for investigating caspase cascade activation and executioner functions within broader cell death research.
Caspase Classification and Molecular Mechanisms
Domain Architecture and Historical Classification
Caspases are traditionally classified based on phylogenetic relationship, proteolytic specificity, and function. Structurally, they contain an N-terminal pro-domain followed by large (p20) and small (p10) catalytic subunits. Based on pro-domain length and structure, caspases are categorized as:
- CARD-domain containing: caspase-1, -2, -4, -5, -9, -11, -12
- DED-domain containing: caspase-8, -10
- Short/no pro-domain: caspase-3, -6, -7 [1] [12]
Historically, caspases were functionally divided into inflammatory caspases (caspase-1, -4, -5, -11) that process pro-inflammatory cytokines and apoptotic caspases, further subdivided into initiators (caspase-2, -8, -9, -10) and executioners (caspase-3, -6, -7) [2]. However, research using deficient models has demonstrated significant functional crossover, challenging this rigid classification.
Caspase Activation Pathways and Cross-Talk
Caspases operate within hierarchical yet interconnected activation networks. The diagram below illustrates the core caspase activation pathways and their functional relationships identified through studies in deficient models.
Figure 1: Caspase Signaling Network and Cross-Talk. Caspase activation occurs through hierarchical yet interconnected pathways. Key regulatory interactions identified through deficient models include caspase-8 inhibition of necroptosis and effector caspase feedback amplification. [1] [31] [27]
Caspase-Deficient Mouse Models: Phenotypes and Applications
Genetically engineered mouse models with targeted caspase deletions have revealed tissue-specific functions, developmental requirements, and disease connections. The table below summarizes key phenotypic characteristics of caspase-deficient mouse models.
Table 1: Phenotypic Characteristics of Caspase-Deficient Mouse Models
| Caspase | Viability | Key Phenotypes | Aging/Homeostasis Traits | Therapeutic Implications |
|---|---|---|---|---|
| Caspase-2 | Viable | Enhanced aging-related traits: shortened maximum lifespan, impaired hair growth, increased bone loss, reduced body fat [32] | Higher levels of oxidized proteins in liver; compromised clearance of damaged cells [32] | Potential role in age-related degeneration |
| Caspase-8 | Embryonic lethal (E10.5-11.5) [33] | Endothelial cell death, circulatory failure; preventable by Ripk1 or Ripk3 co-deletion [33] | Chronic RIPK1-dependent inflammatory gene activation independent of RIPK3 [33] | Inflammation control; necroptosis regulation |
| Caspase-3/7 Double KO | Perinatal lethal [31] | Disorganized heart development; profound resistance to apoptotic stimuli [31] | Essential for feedback amplification in apoptotic cascades [31] | Chemotherapy resistance mechanisms |
| Executioner Caspases | Viable (conditional) | Sublethal activation promotes liver regeneration via JAK/STAT3 pathway [30] | Hepatocytes with ECA survive and proliferate during regeneration [30] | Tissue regeneration and repair |
Specialized Methodologies for Mouse Studies
Lineage Tracing of Caspase Activation
The mCasExpress system enables precise tracking of cells that have experienced executioner caspase activation (ECA). This transgenic approach utilizes:
- Genetic construct: CAG-loxP-STOP-loxP-rtTA × TRE-Lyn11-NES-DEVD-FLP × CAG-FRT-STOP-FRT-ZsGreen
- Activation mechanism: Caspase-mediated cleavage releases FLP recombinase from membrane tethering
- Detection: Nuclear FLP triggers permanent ZsGreen expression upon ECA [30]
Application workflow:
- Cross mCasExpress mice with tissue-specific Cre drivers (e.g., Sox2-Cre for epiblast-derived tissues)
- Induce LN-DEVD-FLP expression with doxycycline (5 mg/kg via tail vein)
- Monitor ZsGreen expression over time (peak detection at 7 days post-induction)
- Validate specificity using caspase-3/7 double knockout controls [30]
This system identified sublethal ECA in hepatocytes during liver regeneration, revealing non-apoptotic roles for executioner caspases in proliferation.
Cell-Type Specific Deletion Strategies
Cell-type specific caspase deletion reveals compartment-specific functions:
- Endothelial deletion: Tie1-Cre × Casp8fl/fl mice show inflammatory gene upregulation
- Hepatocyte deletion: Albumin-Cre causes mild inflammatory activation
- Myelomonocytic deletion: LysM-Cre shows minimal inflammatory changes [33]
Protocol for phenotypic analysis:
- Generate Casp8fl/fl Ripk3-/- mice with cell-type specific Cre
- Assess embryonic tissues at E16.5 for inflammatory gene expression
- Isolate specific cell populations (CD45-CD31+ endothelial cells) by FACS
- Quantify inflammatory mediators (CXCL10, CCL5, TNF) in embryonic sera by ELISA [33]
Caspase-Deficient Cell Lines: Signaling Insights and Technical Approaches
CRISPR-Cas9 Generation of Caspase-Deficient Lines
CRISPR-Cas9 methodology enables systematic analysis of caspase requirements in human cells:
Experimental workflow for effector caspase dissection:
- Vector design: Utilize LentiCRISPR vectors with sgRNAs targeting caspase-3 (mCherry), caspase-7 (eGFP), and caspase-6 (RFP657)
- Cell transduction: Transduce human leukemia cells (NALM6, 658w, Jurkat) with caspase-targeting vectors
- Clone isolation: Single-cell sorting and expansion of clonal populations
- Validation: Western blot verification of specific caspase deletion
- Functional screening: Treat with extrinsic (Birinapant/TNF) and intrinsic (ABT263) apoptotic stimuli
- Viability assessment: Measure cell death using 7-AAD staining and flow cytometry [31]
Key Findings from Caspase-Deficient Cell Models
Table 2: Functional Redundancy and Specialization in Caspase-Deficient Cell Lines
| Caspase Deficiency | Extrinsic Apoptosis Response | Intrinsic Apoptosis Response | Upstream Cascade Effects | Functional Interpretation |
|---|---|---|---|---|
| Caspase-3-/- | Normal cell death [31] | Normal cell death [31] | Normal initiator caspase activation | Functional redundancy in single knockouts |
| Caspase-7-/- | Normal cell death [31] | Normal cell death [31] | Normal initiator caspase activation | Functional redundancy in single knockouts |
| Caspase-3/7-/- | Profound resistance [31] | Profound resistance [31] | Defective caspase-8/-9 activation; decreased mitochondrial depolarization [31] | Essential feedback amplification role |
| Caspase-6-/- | Normal cell death [31] | Normal cell death [31] | No significant effect alone or in combination | Limited role in apoptosis execution |
| Caspase-8-/- | Resistant [31] | Normal response [31] | Blocks extrinsic pathway only | Specific initiator function |
| Caspase-9-/- | Normal response [31] | Resistant [31] | Blocks intrinsic pathway only | Specific initiator function |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Caspase Deficiency Research
| Reagent/Cell Line | Specific Application | Key Findings Enabled | Technical Considerations |
|---|---|---|---|
| mCasExpress mice | Lineage tracing of cells with executioner caspase activation | Identification of sublethal caspase activation in liver regeneration [30] | Requires Cre driver and doxycycline induction; optimal detection 7 days post-induction |
| Caspase-2-/- mice | Study of apoptosis in aging processes | Caspase-2 deficiency enhances aging traits and reduces maximum lifespan [32] | Normal development with late-onset phenotypes; requires aging cohorts |
| Casp3/7-/- MEFs | Analysis of effector caspase redundancy | Caspase-3/7 double knockout required for apoptosis resistance [31] | Perinatal lethality in mice requires embryonic derivation |
| SH-SY5Y cells (Casp8-/-) | Study of alternative death pathways | TLR3 activation switches to lysosomal cell death in caspase-8 absence [34] | Endogenously caspase-8 and RIPK3 deficient; requires IFN-1 to restore TLR3 expression |
| LentiCRISPR system | Generation of caspase-deficient cell lines | Revealed caspase-3/7 feedback amplification of upstream signals [31] | Enables multiplex targeting; requires validation of clonal populations |
| Pan-caspase inhibitor zVAD | Caspase activity blockade | Confirmed caspase-independent death in SH-SY5Y cells [34] | Can have off-target effects; use with appropriate controls |
Advanced Signaling Concepts Revealed by Deficient Models
Feedback Amplification in Apoptotic Cascades
Studies in caspase-3/7 double-deficient cells revealed a critical feedback mechanism wherein these effector caspases amplify upstream apoptotic signaling. This creates a switch-like commitment to cell death:
Molecular mechanism:
- Effector caspases enhance mitochondrial depolarization and cytochrome c release
- Caspase-3/7 activity promotes further activation of caspase-8 and -9
- This positive feedback ensures rapid, complete apoptosis commitment [31]
Experimental evidence:
- Casp3/7-/- cells show defective caspase-8/-9 activation despite apoptotic stimuli
- Mitochondrial depolarization is delayed and reduced in Casp3/7-/- cells
- Single caspase-3 or -7 deletion produces minimal effect, demonstrating functional redundancy [31]
Non-Apoptotic Functions and Sublethal Activation
The mCasExpress system revealed that executioner caspase activation (ECA) can occur at sublethal levels and promote proliferation rather than death:
Liver regeneration findings:
- Hepatocytes with ECA expand after partial hepatectomy or CCl4 treatment
- Most hepatocytes with ECA survive and proliferate during regeneration
- Optimal regeneration requires precise control of ECA at sublethal levels [30]
Molecular pathway:
- Sublethal ECA promotes hepatocyte proliferation through JAK/STAT3 activation
- Inhibition of ECA reduces hepatocyte proliferation and impairs regeneration
- Excessive ECA causing hepatocyte death also impedes regeneration [30]
Context-Dependent Caspase Switching Between Death Pathways
Caspase-8 deficiency demonstrates how cells switch between death modalities based on caspase activity:
Necroptosis induction:
- Caspase-8 normally cleaves RIPK1 and RIPK3 to inhibit necroptosis
- Caspase-8 deficiency permits RIPK1/RIPK3/MLKL-mediated necroptosis [33] [27]
Alternative death pathways:
- In neuroblastoma cells, caspase-8 deficiency switches TLR3-induced apoptosis to lysosomal cell death
- This alternative death involves lysosomal permeabilization and cathepsin release
- Cell death proceeds independently of caspase activity and RIPK3 [34]
Caspase-deficient models have transformed our understanding of cell death from linear hierarchical models to complex networks with redundancy, feedback, and context-dependent outcomes. The experimental approaches outlined here provide researchers with robust methodologies for dissecting caspase functions in specific biological contexts. As research progresses, emerging technologies including more sophisticated lineage tracing, inducible systems, and human organoid models will further refine our understanding of caspase networks in development, homeostasis, and disease.
Caspases, or cysteine-aspartic proteases, are a family of evolutionarily conserved enzymes that function as central regulators of programmed cell death (apoptosis) and inflammation [35] [5]. These proteases cleave their substrates after specific aspartic acid residues and are synthesized as inactive zymogens that require proteolytic activation during apoptotic signaling [17] [35]. Based on their functions, caspases are categorized into initiator caspases (caspase-2, -8, -9, -10) that initiate apoptotic pathways, executioner caspases (caspase-3, -6, -7) that carry out the apoptotic program, and inflammatory caspases (caspase-1, -4, -5, -11, -12, -14) that mediate inflammatory responses [35]. The activation of executioner caspases represents a critical commitment point in apoptosis, leading to the cleavage of hundreds or thousands of cellular substrates and the characteristic morphological changes of cell death, including chromatin condensation, DNA fragmentation, and membrane blebbing [17] [5]. While historically considered a "point of no return," recent research has revealed that cells can survive executioner caspase activation under certain conditions, with significant implications for tissue regeneration and cancer therapy resistance [5]. This technical guide provides comprehensive methodologies for detecting caspase activity, focusing on Western blotting for cleavage detection and modern activity-based probes, framed within contemporary research on caspase cascade activation and executioner functions.
Caspase Activation Pathways and Molecular Mechanisms
Biochemical Basis of Caspase Activation
Initiator and executioner caspases undergo distinct activation mechanisms. Executioner caspases exist in healthy cells as inactive homodimers, where cleavage by initiator caspases between the large and small subunits induces a conformational change that activates them [17] [5]. In contrast, initiator caspases exist as inactive monomers that are activated through dimerization at multi-protein signaling complexes via adapter proteins containing death folds such as death effector domains (DEDs) or caspase activation and recruitment domains (CARDs) [17] [35]. This "induced proximity" model explains how initiator caspases such as caspase-8 and -9 become activated without requiring prior cleavage, though cleavage does serve to stabilize the active dimer [17].
Caspase Activation Pathways
Caspase activation occurs through two primary pathways: the extrinsic (death receptor) pathway and the intrinsic (mitochondrial) pathway [35]. The extrinsic pathway is triggered by external signals that interact with surface death receptors like Fas and TNF receptors, leading to the formation of the death-inducing signaling complex (DISC) and initiation of caspase-8 [36] [35]. The intrinsic pathway is activated by internal cellular stress signals that cause mitochondrial outer membrane permeabilization (MOMP), leading to the formation of the apoptosome complex and activation of caspase-9 [35] [5]. Cross-talk between these pathways occurs through caspase-8-mediated cleavage of the BH3-only protein Bid, which connects extrinsic signaling to mitochondrial amplification of the death signal [5].
Diagram Title: Caspase Activation Pathways in Apoptosis
Western Blotting for Caspase Cleavage Detection
Principles and Methodological Framework
Western blotting remains a foundational technique for detecting caspase activation through cleavage-specific antibodies that recognize the processed forms of caspases [37]. The technique involves electrophoretic separation of proteins, transfer to a membrane, and detection using antibodies specific to caspase subunits or cleavage sites [37]. Quantitative fluorescent Western blotting (QFWB) has emerged as a superior approach compared to traditional chemiluminescent methods, providing a linear detection profile that enables accurate comparative expression analysis [37]. This linearity is particularly important when measuring subtle differences in expression levels that can lead to inaccurate measurements with saturation-prone ECL techniques [37].
Detailed Protocol for Caspase Detection via Western Blotting
Sample Preparation:
- Homogenize tissue samples in RIPA buffer (25 mM Tris-HCl [pH 7.6], 150 mM NaCl, 1% NP-40, 1% sodium deoxycholate, 0.1% SDS) containing protease inhibitors at approximately 1:10 w/v (tissue weight/buffer volume) [37].
- Centrifuge homogenates at 20,000 × g for 20 minutes at 4°C and collect supernatant containing solubilized proteins [37].
- Determine protein concentration using BCA or Bradford assays, ensuring a coefficient of determination (R²) ≥ 0.99 for accuracy [37].
- Prepare samples by mixing protein lysate with loading buffer, heating at 98°C for 2 minutes, and loading 15-30 μg per well for neuronal or cell line samples [37].
Electrophoresis and Transfer:
- Use 4-12% Bis-Tris gradient gels for optimal protein separation across broad molecular weight ranges [37].
- Employ MES running buffer for proteins between 3.5-160 kDa or MOPS buffer for high molecular weight proteins above 200 kDa [37].
- Conduct electrophoresis at 80V for 4 minutes initially, then increase to 180V for approximately 50 minutes [37].
- Transfer proteins to nitrocellulose or PVDF membranes using optimized transfer systems [37].
Immunodetection:
- Block membranes with appropriate blocking solutions (e.g., 5% milk or BSA in TBST) [36].
- Incubate with primary antibodies specific for caspase cleavage forms: anti-caspase-3 (cleaved), anti-caspase-8 (cleaved), or anti-PARP (cleaved) as a downstream caspase substrate [36] [37].
- Use fluorescently-labeled secondary antibodies (e.g., IRDye 800CW or Alexa Fluor 680) for quantitative detection [37].
- Image blots using laser-scanning imaging systems such as LI-COR Odyssey, which provides direct linear quantification of protein abundance [37].
Controls and Validation:
- Include positive controls such as recombinant active caspases or apoptosis-induced cell lysates [37].
- Implement loading controls using housekeeping proteins (actin, GAPDH) or total protein stains [37].
- Validate antibody specificity through knockout cell lines or siRNA-mediated knockdown where possible [37].
Diagram Title: Western Blot Workflow for Caspase Detection
Activity-Based Probes and Advanced Detection Methodologies
Modern Imaging Approaches for Caspase Activity
Recent advancements in caspase detection have enabled real-time monitoring of caspase dynamics in live cells using fluorescent reporters and biosensors [38]. Genetically-encoded caspase sensors utilize cleavage-specific motifs (such as DEVD for caspases-3/7) linked to fluorescent proteins that undergo fluorescence activation upon caspase-mediated cleavage [38]. The ZipGFP-based caspase-3/7 reporter represents a cutting-edge example, employing a split-GFP architecture where caspase cleavage separates β-strands, allowing spontaneous refolding into fluorescent GFP [38]. This system provides high specificity, minimal background fluorescence, and irreversible signal accumulation that enables persistent marking of apoptotic events at single-cell resolution [38].
Protocol for Live-Cell Caspase Imaging:
- Generate stable cell lines expressing lentiviral-delivered caspase reporters (ZipGFP-DEVD-mCherry) [38].
- Plate cells in optical-grade plates and treat with apoptosis-inducing agents (e.g., carfilzomib, oxaliplatin) [38].
- Conduct time-lapse imaging using live-cell microscopy systems (e.g., IncuCyte) over 24-120 hours [38].
- Include controls with pan-caspase inhibitors (zVAD-FMK) to confirm caspase-specific signaling [38].
- Quantify fluorescence intensity normalized to constitutive markers (mCherry) to account for cell presence [38].
Multiplexed Detection in Complex Model Systems
Modern caspase detection platforms have been adapted for 3D culture systems including spheroids and patient-derived organoids, providing physiological relevance for therapeutic studies [38]. These systems enable researchers to monitor caspase activation within heterogeneous tissue-like structures and investigate complex processes such as apoptosis-induced proliferation (AIP) and immunogenic cell death (ICD) [38]. For ICD detection, endpoint measurements of surface calreticulin exposure can be combined with real-time caspase monitoring via flow cytometry, enabling multidimensional analysis of cell death mechanisms [38].
Comparative Analysis of Caspase Detection Methods
Table 1: Comparison of Major Caspase Detection Methodologies
| Method | Principle | Sensitivity | Temporal Resolution | Applications | Key Advantages |
|---|---|---|---|---|---|
| Western Blotting | Cleavage-specific antibodies | Moderate | Endpoint | Bulk protein analysis, validation | Quantifiable, specific, widely accessible |
| Fluorescent Western | Fluorescent secondary antibodies | High | Endpoint | Quantitative comparison, subtle expression changes | Linear detection, broad dynamic range [37] |
| Live-Cell Imaging (ZipGFP) | Caspase-activated GFP reconstitution | Very High | Real-time (minutes) | Single-cell dynamics, kinetics, heterogeneity | Spatiotemporal resolution, irreversible marking [38] |
| FRET Sensors | Cleavage-dependent energy transfer | High | Real-time (minutes) | Rapid kinetics, intracellular localization | Ratiometric measurement, subcellular targeting |
| Activity-Based Probes | Covalent binding to active site | High | Near-real-time | Enzyme kinetics, inhibitor profiling | Active enzyme specific, functional assessment |
Table 2: Caspase-Specific Antibodies for Western Blot Analysis
| Target | Clone/Source | Dilution | Application | Expected Band Sizes |
|---|---|---|---|---|
| Caspase-3 | Rabbit polyclonal (Cell Signaling #9662) | 1:2,000 | Cleaved caspase-3 detection | 17/19 kDa (cleaved) [36] |
| Caspase-8 | Mouse monoclonal (clone C15) | 1:20 | DISC analysis, cleavage detection | 18/41 kDa (cleaved) [36] |
| Caspase-10 | Mouse monoclonal (MBL #M059-3) | 1:1,000 | Initiator caspase detection | 17/21 kDa (cleaved) [36] |
| PARP-1 | Rabbit polyclonal (Cell Signaling #9542) | 1:1,000 | Executioner caspase substrate | 89 kDa (cleaved) [36] |
| FADD | Mouse monoclonal (clone 1C4) | 1:10 | DISC immunoprecipitation | 23 kDa [36] |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Caspase Detection Experiments
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Cell Lines | HeLa-CD95, HT29, MCF-7 (caspase-3 deficient) | Model systems for apoptosis induction [36] [38] |
| Apoptosis Inducers | CD95L, carfilzomib, oxaliplatin | Activation of extrinsic and intrinsic pathways [36] [38] |
| Caspase Inhibitors | zVAD-FMK (pan-caspase) | Specificity controls, mechanistic studies [38] |
| Lysis Buffers | RIPA, NP-40, Tris-Triton | Protein extraction for Western blotting [37] |
| Detection Antibodies | Anti-caspase-3 (#9662), anti-PARP (#9542) | Cleavage detection in Western blot [36] |
| Fluorescent Reporters | ZipGFP-DEVD-mCherry construct | Real-time caspase-3/7 activity monitoring [38] |
| Molecular Weight Markers | Pre-stained protein standards | Size determination in gel electrophoresis [37] |
| Fluorescent Secondaries | IRDye 800CW, Alexa Fluor 680 | Quantitative fluorescent Western blotting [37] |
Technical Considerations and Research Applications
Methodological Optimization and Troubleshooting
Successful caspase detection requires careful optimization of several technical parameters. For Western blotting, protein load must be optimized to maintain linear detection ranges, typically 15-30 μg for cell line extracts [37]. Antibody validation is crucial, particularly for cleavage-specific antibodies, using positive controls such as recombinant proteins or apoptosis-induced cell lysates [37]. In live-cell imaging, reporter expression levels must be balanced to avoid artificial caspase activation from overexpression, while ensuring sufficient signal-to-noise ratio for detection [38]. For 3D models, imaging depth and light penetration must be considered, often requiring confocal microscopy or optical clearing techniques [38].
Research Applications in Drug Discovery and Mechanistic Studies
Detection of caspase activity has become indispensable in pharmaceutical development and basic research. In cancer drug discovery, caspase activation serves as a key pharmacodynamic marker for assessing therapeutic efficacy of chemotherapeutic agents [35] [38]. High-content screening platforms integrating caspase reporters enable mechanistic dissection of cell death pathways and identification of novel modulators of apoptosis [38]. In translational research, caspase detection in patient-derived organoids provides clinically relevant models for predicting therapeutic responses and understanding resistance mechanisms [38]. Furthermore, the combination of caspase activity monitoring with immunogenic cell death markers facilitates the development of combinatorial regimens that enhance antitumor immunity [38].
The comprehensive detection of caspase activity through Western blotting for cleavage fragments and activity-based probes provides critical insights into the regulation and execution of apoptotic pathways. While Western blotting remains a fundamental tool for quantitative, endpoint analysis of caspase activation, modern fluorescent reporters and live-cell imaging platforms enable unprecedented spatial and temporal resolution of caspase dynamics in physiologically relevant model systems. The integration of these complementary approaches, along with emerging technologies such as mass spectrometry-based substrate identification and high-content screening, continues to advance our understanding of caspase functions in both cell death and survival. As research increasingly reveals the complex roles of caspases in disease pathogenesis and treatment responses, these detection methodologies will remain essential tools for basic research and therapeutic development.
Apoptosis, or programmed cell death, is a fundamental biological process critical for development, tissue homeostasis, and disease pathogenesis. Its execution is orchestrated by a family of cysteine proteases known as caspases (cysteine-dependent aspartate-specific proteases), which cleave their substrates after aspartic acid residues [3] [21]. Caspases are synthesized as inactive zymogens (procaspases) and become activated through proximity-induced dimerization (initiator caspases) or proteolytic cleavage (executioner caspases) [3]. The core apoptotic machinery consists of two primary pathways. The extrinsic pathway is initiated by extracellular death ligands (e.g., FasL, TRAIL) binding to cell surface receptors, leading to the formation of the Death-Inducing Signaling Complex (DISC) and activation of caspase-8 [3] [27]. The intrinsic pathway, triggered by internal stresses like DNA damage, involves mitochondrial outer membrane permeabilization and release of cytochrome c, which promotes the formation of the apoptosome and activation of caspase-9 [3] [27]. Both pathways converge on the activation of executioner caspases (caspase-3, -6, and -7), which systematically dismantle the cell by cleaving hundreds of cellular substrates [3] [12]. Profiling the apoptotic proteome—the complete set of proteins involved and modified during this process—is therefore essential for understanding the mechanistic underpinnings of cell death. This guide details the two predominant technologies for such profiling: antibody microarrays and mass spectrometry.
Antibody Microarray Technology
Principle and Workflow
The antibody microarray is a multiplexed immunoassay technology that allows for the parallel analysis of numerous proteins from a single sample. The concept is built on immobilizing hundreds of specific antibodies in a predefined array pattern onto a solid surface [39].
A typical workflow involves the following steps:
- Antibody Immobilization: Antibodies are printed onto a chemically functionalized surface, such as a glass slide or membrane.
- Blocking: The remaining reactive groups on the surface are blocked to prevent non-specific binding.
- Sample Incubation: A fluorescently labelled protein sample (e.g., cell lysate from apoptotic cells) is incubated on the array. Target proteins are captured by their cognate antibodies.
- Washing and Detection: Unbound proteins are washed away, and the resulting binding events are detected by measuring the fluorescence intensity at each spot, which correlates with the abundance of the captured protein [39].
Key Applications in Apoptosis Research
Antibody microarrays are particularly suited for apoptosis research due to their ability to simultaneously monitor the abundance and post-translational modifications of key signaling molecules.
- Signaling Pathway Analysis: Researchers have used antibody arrays to investigate changes in cell death pathways. For instance, one study utilizing antibody microarrays identified significant alterations in MAPK signaling and apoptotic markers in a mouse model of Alzheimer's disease, findings that were subsequently validated by immunohistochemistry [39].
- Biomarker Discovery: In clinical and basic research, antibody microarrays are frequently used as an initial discovery tool to identify protein signatures that differentiate healthy from diseased states, such as cancer [39] [40]. For example, the RayBio Human Apoptosis Antibody Array can screen the relative levels of 43 apoptosis-related proteins, including Bcl-2 family members, IAPs, and caspases [40].
- Post-Translational Modification Profiling: Specialized arrays with antibodies targeting phosphorylated epitopes can dissect kinase-driven regulatory events in apoptosis. One study employed a phospho-explorer antibody microarray to uncover mTOR pathway upregulation in a knock-out model, revealing a novel feedback mechanism [39].
Advantages and Limitations
Advantages:
- High-throughput: Can analyze dozens to hundreds of proteins in a single experiment.
- Speed: The entire assay, from sample preparation to data interpretation, can be completed in less than 24 hours.
- Sensitivity: Capable of detecting low-abundance proteins, often surpassing traditional Western blotting.
- Small Sample Volume: Requires minimal sample material, a critical advantage for precious clinical specimens [39].
Limitations:
- Cross-reactivity: A primary challenge is the potential for antibodies to bind off-target proteins, which can compromise specificity.
- Limited Scope: The technique is inherently limited to proteins for which specific antibodies are available on the array.
- Validation Required: Discoveries from antibody microarray screens typically require confirmation using orthogonal methods like Western blot or ELISA [39].
Mass Spectrometry-Based Proteomics
Principle and Workflow
Mass spectrometry (MS) is a powerful, unbiased technology for identifying and quantifying proteins on a global scale. It does not rely on predefined antibodies but rather separates and detects proteins or peptides based on their mass-to-charge ratio (m/z).
A standard workflow for apoptotic proteome analysis includes:
- Protein Separation and Digestion: Complex protein mixtures from apoptotic cells are separated, often by one-dimensional or two-dimensional gel electrophoresis (2DGE). Proteins of interest are excised and digested with a protease (e.g., trypsin) to generate peptides [41].
- Liquid Chromatography: The peptide mixture is fractionated by liquid chromatography (LC) to reduce complexity before introduction to the mass spectrometer [42].
- Mass Spectrometry Analysis: Peptides are ionized and analyzed by the mass spectrometer. Tandem MS (MS/MS) fragments selected peptides, generating spectra that reveal their amino acid sequence [41].
- Data Analysis: Computational tools search the MS/MS spectra against protein databases to identify the proteins present in the original sample. Quantification is achieved by comparing signal intensities between samples [41] [42].
Key Applications in Apoptosis Research
MS-based proteomics has been instrumental in providing a systems-level view of the apoptotic process.
- Discovery of Protein Alterations: Classical proteomics using 2DGE and MS has enabled the identification of over 100 proteins that are altered during apoptosis, providing functional data on protein degradation, synthesis, and post-translational modification [41].
- Analysis of Specific Complexes: Targeted MS approaches have been designed to characterize key apoptotic components, such as the Death-Inducing Signaling Complex (DISC), mitochondrial-releasing factors, and proteins interacting with Inhibitor of Apoptosis (IAP) proteins. These studies have significantly advanced the elucidation of apoptotic signaling concepts [41].
- Targeted Metabolomics and Proteomics: Recent applications extend beyond proteins to include metabolites. For instance, a 2024 study used liquid chromatography-tandem mass spectrometry (LC-MS/MS) to quantitatively profile relevant metabolites within apoptotic bodies, opening new avenues for understanding the metabolic consequences of cell death [42].
Advantages and Limitations
Advantages:
- Comprehensiveness: Offers an unbiased, global view of the proteome without being limited to predetermined targets.
- Detailed Characterization: Can identify novel proteins, precise cleavage sites (e.g., caspase substrates), and a wide range of post-translational modifications.
- High Specificity: Provides definitive protein identification based on amino acid sequence.
Limitations:
- Throughput and Speed: The process is generally slower and more complex than antibody array workflows.
- Cost and Expertise: Requires expensive instrumentation and significant bioinformatics expertise for data analysis.
- Dynamic Range: Can struggle to detect very low-abundance proteins in complex mixtures compared to antibody-based methods.
Comparative Analysis: Antibody Arrays vs. Mass Spectrometry
Table 1: A direct comparison of antibody microarray and mass spectrometry approaches for apoptotic proteome profiling.
| Feature | Antibody Microarray | Mass Spectrometry |
|---|---|---|
| Principle | Protein capture by immobilized antibodies | Detection of peptides based on mass-to-charge ratio |
| Throughput | High (multiplexed) | Moderate to High (comprehensive) |
| Scope | Targeted (limited by antibody panel) | Global / Unbiased |
| Assay Time | Fast (< 24 hours) [39] | Slower (days) |
| Sample Volume | Small | Moderate to Large |
| Primary Application | Targeted screening and hypothesis generation | Discovery and system-wide analysis |
| Key Strength | Ease of use, speed, sensitivity | Comprehensiveness, discovery power |
| Main Weakness | Cross-reactivity, limited target scope | Cost, complexity, data analysis burden |
Table 2: A selection of key research reagents and tools for apoptotic proteome profiling, as identified from the literature.
| Resource / Assay | Key Function | Example Use in Apoptosis Research |
|---|---|---|
| RayBio Human Apoptosis Antibody Array [40] | Simultaneously detects relative levels of 43 apoptotic biomarkers (e.g., Bcl-2 family, IAPs, caspases). | Screening apoptosis-related protein expression in cell or tissue lysates. |
| Proteome Profiler Human Apoptosis Array [43] | Antibody array kit for identifying key apoptotic proteins from cell lysates. | Proteome analysis to identify targeted proteins in breast cancer cell lines. |
| Phospho-Specific Antibody Microarrays [39] | Profiling of phosphorylation-driven signaling pathways. | Dissecting kinase activity and signaling feedback loops in cell death. |
| Caspase Activity Assays [40] | Functional assays to measure the enzymatic activity of specific caspases. | Determining the point of caspase cascade activation. |
| LC-MS/MS with Q-Orbitrap Systems [42] | High-resolution, accurate mass measurement for targeted metabolomics and proteomics. | Quantitative analysis of metabolites in apoptotic bodies. |
Experimental Protocol: Profiling Apoptosis with an Antibody Array
The following is a generalized protocol based on methodologies described in the search results [39] [43]:
Sample Preparation:
- Induce apoptosis in cultured cells (e.g., MCF-7, MDA-MB-231) using a relevant stimulus (e.g., UV radiation, chemotherapeutic agent).
- Lyse cells at a specific time point post-induction using an appropriate lysis buffer.
- Determine the total protein concentration of the lysates using a standardized method like the Bradford assay.
Array Processing:
- Incubate the array membrane or slide with a blocking buffer to minimize non-specific binding.
- Add a predetermined amount of protein lysate to the array and incubate for several hours to allow protein-antibody binding.
- Wash the array thoroughly to remove unbound proteins.
- Incubate with a cocktail of biotinylated detection antibodies.
- Incubate with a streptavidin-conjugated fluorophore or horseradish peroxidase (HRP) for chemiluminescent detection.
Data Acquisition and Analysis:
- Scan the membrane or slide using an appropriate imaging system (e.g., ChemiDoc MP Imaging System).
- Analyze the spot intensities using dedicated image analysis software (e.g., Image Lab).
- Normalize the data to internal controls and compare signal intensities between treated and control samples to identify differentially expressed apoptotic proteins.
Visualizing Apoptotic Signaling and Experimental Workflow
The following diagrams illustrate the core apoptotic pathways and the technical workflows for profiling them.
Diagram 1: Core Apoptotic Caspase Cascade. This diagram illustrates the extrinsic and intrinsic pathways of apoptosis, which converge on the activation of executioner caspases that dismantle the cell. Proteins in yellow represent inactive zymogens, while red, green, and blue indicate activated caspases in their respective pathways [3] [27].
Diagram 2: Antibody Microarray Workflow. The key steps involve preparing a labeled protein sample from apoptotic cells, incubating it on the array to allow specific binding, and then detecting the captured proteins to generate a quantitative profile [39].
The comprehensive profiling of apoptotic proteomes is indispensable for deciphering the complex regulatory networks of cell death. Both antibody microarrays and mass spectrometry offer powerful, yet complementary, approaches for this task. Antibody microarrays provide a rapid, sensitive, and accessible platform for targeted screening of known apoptosis regulators, making them ideal for hypothesis-driven research and initial biomarker discovery. In contrast, mass spectrometry offers an unbiased discovery tool for mapping the global proteome, identifying novel caspase substrates, and characterizing specific apoptotic complexes in unparalleled detail. The choice between these technologies should be guided by the specific research question, available resources, and desired depth of analysis. Integrating both methods often yields the most robust and comprehensive insights, driving forward our understanding of caspase biology and its implications for human health and disease.
Caspases (cysteine-dependent aspartate-specific proteases) are a family of evolutionarily conserved enzymes that function as central regulators of programmed cell death (PCD) and inflammation [2] [1]. In the context of cancer, the apoptotic function of caspases is of paramount importance, as malignant cells frequently exhibit evasion of apoptosis, a hallmark of cancer that enables uncontrolled proliferation and tumor development [44]. Caspases are synthesized as inactive zymogens (procaspases) that undergo proteolytic activation in response to specific death signals. Based on their apoptotic functions, caspases are broadly classified into initiator caspases (caspase-2, -8, -9, -10) and executioner caspases (caspase-3, -6, -7) [3] [5]. Initiator caspases contain long prodomains with protein-protein interaction motifs such as the death effector domain (DED) or caspase activation and recruitment domain (CARD), which enable their recruitment to and activation within multiprotein signaling complexes [3]. Executioner caspases possess short prodomains and are activated through cleavage by initiator caspases; they subsequently mediate the proteolytic dismantling of cellular structures during apoptosis [5].
The caspase activation cascade can be triggered through two principal apoptotic pathways: the extrinsic (death receptor) pathway and the intrinsic (mitochondrial) pathway [44] [1]. The extrinsic pathway is initiated by the binding of extracellular death ligands (e.g., FasL, TRAIL) to their cognate death receptors on the cell surface, leading to the assembly of the death-inducing signaling complex (DISC) and activation of caspase-8 [3]. The intrinsic pathway is activated in response to intracellular stress signals (e.g., DNA damage, oxidative stress), resulting in mitochondrial outer membrane permeabilization (MOMP), cytochrome c release, formation of the apoptosome complex, and activation of caspase-9 [3] [45]. Both pathways converge on the activation of executioner caspases (primarily caspase-3, -6, and -7), which orchestrate the controlled demolition of the cell through cleavage of hundreds of cellular substrates [5]. In cancer therapy, the strategic reactivation of these dormant apoptotic pathways represents a promising approach to eliminate malignant cells.
Table 1: Caspase Classification and Functions in Apoptosis
| Caspase Type | Members | Activation Mechanism | Primary Functions in Apoptosis |
|---|---|---|---|
| Initiator | Caspase-8, -9, -10 | Induced proximity/dimerization in multiprotein complexes (DISC, apoptosome) | Initiate apoptotic signaling; cleave and activate executioner caspases |
| Executioner | Caspase-3, -6, -7 | Proteolytic cleavage by initiator caspases | Mediate proteolytic demolition of cellular structures; cleave key substrates (e.g., PARP, lamins) |
Therapeutic Strategies Targeting Caspase Activation
The development of pro-apoptotic agonists for cancer therapy focuses on overcoming the anti-apoptotic defenses of cancer cells by directly or indirectly activating caspase cascades. Key therapeutic classes include SMAC mimetics, BH3 mimetics, MDM2 inhibitors, and TRAIL receptor agonists, each targeting specific nodes in the apoptotic regulatory network [44].
SMAC Mimetics
Second mitochondria-derived activator of caspase (SMAC)/DIABLO is an endogenous protein released from mitochondria during apoptosis that antagonizes inhibitor of apoptosis proteins (IAPs) [44]. IAPs, including XIAP, cIAP1, and cIAP2, suppress apoptosis by directly inhibiting caspase activity, particularly caspases-3, -7, and -9 [7]. SMAC mimetics are small molecule compounds designed to mimic the N-terminal tetrapeptide of SMAC, which binds to and neutralizes IAPs [44]. By antagonizing IAPs, SMAC mimetics promote caspase activation and apoptosis. Notably, SMAC mimetics also induce the auto-ubiquitination and proteasomal degradation of cIAP1 and cIAP2, leading to non-canonical NF-κB activation and production of pro-survival cytokines in some contexts, which can represent a resistance mechanism [44].
BH3 Mimetics
The B-cell lymphoma 2 (BCL-2) family of proteins governs mitochondrial outer membrane permeabilization (MOMP), a critical step in the intrinsic apoptotic pathway [45]. Anti-apoptotic BCL-2 family members (e.g., BCL-2, BCL-XL, MCL-1) sequester pro-apoptotic proteins like BAX and BAK, preventing mitochondrial cytochrome c release. BH3 mimetics are small molecule inhibitors that bind to the hydrophobic groove of anti-apoptotic BCL-2 proteins, displacing pro-apoptotic proteins and triggering MOMP, cytochrome c release, apoptosome formation, and caspase-9 activation [44] [45]. Venetoclax (ABT-199), a selective BCL-2 inhibitor, has demonstrated clinical success in hematological malignancies [45].
MDM2 Inhibitors
The tumor suppressor p53 is a master regulator of the intrinsic apoptotic pathway, transcriptionally activating pro-apoptotic genes in response to cellular stress. In many cancers, p53 is inactivated, often through overexpression of its negative regulator, MDM2 [44]. MDM2 inhibitors (e.g., nutlins) block the p53-MDM2 interaction, stabilizing p53 and restoring its ability to induce cell cycle arrest and apoptosis [44]. The therapeutic efficacy of MDM2 inhibitors is contingent upon functional p53, limiting their application to tumors retaining wild-type p53.
TRAIL Receptor Agonists
The extrinsic apoptotic pathway can be selectively activated in cancer cells using agonists of TNF-related apoptosis-inducing ligand (TRAIL) receptors (DR4 and DR5) [44]. Recombinant TRAIL and monoclonal antibodies against DR4/DR5 have been developed to trigger DISC assembly and caspase-8 activation. A key advantage of this approach is the potential for selective tumor cell killing, as many cancer cells exhibit greater sensitivity to TRAIL-induced apoptosis than normal cells [44]. However, resistance mechanisms, including downregulation of death receptors or high expression of anti-apoptotic proteins, can limit efficacy.
Table 2: Pro-Apoptotic Agonists in Cancer Therapy
| Therapeutic Class | Molecular Target | Mechanism of Action | Representative Agents | Development Status/Challenges |
|---|---|---|---|---|
| SMAC Mimetics | IAP proteins (XIAP, cIAP1/2) | Antagonize IAP-mediated caspase inhibition; promote cIAP degradation | LCL161, Birinapant, GDC-0152 | Clinical trials; resistance via NF-κB-mediated cytokine production |
| BH3 Mimetics | Anti-apoptotic BCL-2 proteins (BCL-2, BCL-XL, MCL-1) | Displace pro-apoptotic proteins to induce MOMP | Venetoclax, Navitoclax, S63845 | Venetoclax approved for CLL; on-target thrombocytopenia (Navitoclax) |
| MDM2 Inhibitors | MDM2-p53 interaction | Stabilize p53 to activate intrinsic apoptosis | Nutlins, Idasanutlin, RG7388 | Clinical trials; effective only in wild-type p53 tumors |
| TRAIL Receptor Agonists | Death receptors DR4/DR5 | Activate extrinsic apoptosis pathway | Recombinant TRAIL, Conatumumab, Mapatumumab | Clinical trials; resistance due to low receptor expression or high c-FLIP |
Experimental Models and Methodologies for Caspase-Targeted Drug Evaluation
In Vitro Assessment of Caspase Activation and Apoptosis
Protocol 1: Measuring Caspase Activity Using Fluorogenic Substrates Caspase enzymatic activity is routinely quantified in cell lysates or live cells using synthetic tetrapeptide substrates conjugated to fluorescent reporters (e.g., 7-amino-4-methylcoumarin, AMC) [7]. Upon caspase-mediated cleavage, the fluorophore is released, generating a measurable signal.
- Cell Treatment and Lysis: Seed cancer cells in 96-well plates and treat with the pro-apoptotic agonist for 6-24 hours. Harvest cells and lyse in appropriate buffer.
- Reaction Setup: Incubate cell lysates with caspase-specific fluorogenic substrates:
- Caspase-8: Ac-IETD-AFC
- Caspase-9: Ac-LEHD-AFC
- Caspase-3/7: Ac-DEVD-AFC [7]
- Fluorescence Measurement: Monitor fluorescence emission (e.g., AFC: Ex~400 nm, Em~505 nm) over 60-120 minutes using a plate reader.
- Data Analysis: Calculate fold-change in caspase activity relative to untreated controls. Normalize to protein concentration.
Protocol 2: Western Blot Analysis of Caspase Cleavage Immunoblotting detects proteolytic processing of caspases and cleavage of endogenous substrates.
- Protein Extraction: Prepare whole-cell lysates from treated and control cells using RIPA buffer containing protease inhibitors.
- Gel Electrophoresis and Transfer: Separate proteins via SDS-PAGE (12-15% gels) and transfer to PVDF membranes.
- Antibody Probing: Incubate membranes with primary antibodies against:
- Procaspase-8 (inactive, ~55 kDa) and cleaved caspase-8 (active, ~43/18 kDa)
- Procaspase-3 (~35 kDa) and cleaved caspase-3 (~17/19 kDa)
- PARP (full-length: ~116 kDa; cleaved: ~89 kDa) [5]
- Detection: Use HRP-conjugated secondary antibodies and chemiluminescence substrate for visualization. Cleavage fragments confirm caspase activation.
Protocol 3: Live-Cell Imaging of Caspase Activation Fluorescence Resonance Energy Transfer (FRET)-based biosensors enable real-time, single-cell kinetic analysis of caspase activation [5].
- Biosensor Transfection: Transfect cells with a FRET-based caspase sensor (e.g., SCAT3 for caspase-3), which contains a linker with a DEVD cleavage sequence between CFP and YFP.
- Treatment and Imaging: Treat transfected cells with the pro-apoptotic agonist and image using a confocal microscope equipped with environmental control.
- FRET Quantification: Before caspase activation, CFP excitation leads to YFP emission (FRET). Upon caspase-3 cleavage, FRET decreases while CFP emission increases. Calculate the CFP/YFP emission ratio over time. The rapid, "all-or-none" activation kinetics of executioner caspases can be observed, typically peaking within 15 minutes of initiation [5].
In Vivo Evaluation of Antitumor Efficacy
Protocol 4: Xenograft Mouse Models Subcutaneous or orthotopic xenograft models using human cancer cell lines are standard for evaluating the efficacy of pro-apoptotic agonists in vivo.
- Tumor Implantation: Inject luciferase-tagged human cancer cells into the flanks of immunodeficient mice (e.g., NOD/SCID).
- Drug Administration: Once tumors reach a measurable volume (e.g., 100-150 mm³), randomize mice into treatment groups. Administer the pro-apoptotic agonist or vehicle control via oral gavage or intraperitoneal injection.
- Tumor Monitoring: Measure tumor dimensions regularly with calipers. Calculate tumor volume using the formula: V = (length × width²) / 2.
- Terminal Analysis: At the study endpoint, harvest tumors and analyze for indicators of apoptosis (e.g., TUNEL staining, immunohistochemistry for cleaved caspase-3) and proliferation (e.g., Ki-67 staining).
Diagram 1: Caspase Activation Pathways and Therapeutic Targeting Strategies. This diagram illustrates the extrinsic and intrinsic apoptotic pathways, their convergence on executioner caspase activation, and the molecular targets of pro-apoptotic agonists.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Studying Caspase-Targeted Therapies
| Reagent Category | Specific Examples | Research Application | Key Features |
|---|---|---|---|
| Caspase Activity Assays | Fluorogenic substrates (Ac-DEVD-AFC for caspase-3/7), Luminescent Caspase-Glo Assays | Quantify caspase activity in cell lysates or live cells | Sensitive, quantitative, compatible with high-throughput screening |
| Apoptosis Detection Kits | Annexin V-FITC/PI staining, TUNEL assay, M30 CytoDeath antibody | Detect early and late apoptotic markers; measure DNA fragmentation | Flow cytometry or microscopy readout; distinguish apoptosis from necrosis |
| Caspase Inhibitors | Q-VD-OPh (pan-caspase inhibitor), Z-VAD-FMK, Ac-DEVD-CHO (caspase-3 inhibitor) | Confirm caspase-dependent apoptosis; control experiments | Cell-permeable, broad-spectrum or specific; Q-VD-OPh is less toxic [7] |
| IAP Antagonists | Birinapant, LCL161 (SMAC mimetics) | Investigate IAP-dependent caspase regulation | Induce cIAP1/2 degradation; sensitize to TNFα-induced apoptosis |
| BH3 Mimetics | Venetoclax (BCL-2 inhibitor), A-1331852 (BCL-XL inhibitor), S63845 (MCL-1 inhibitor) | Study mitochondrial apoptosis priming and MOMP | Target specific anti-apoptotic BCL-2 proteins; used as single agents or in combinations |
| Antibodies for Immunoblotting | Anti-cleaved caspase-3, anti-cleaved PARP, anti-BID, anti-BAX/BAK | Detect caspase activation and apoptotic signaling by Western blot | Distinguish cleaved (active) from full-length (inactive) forms |
| Live-Cell Apoptosis Reporters | FRET-based SCAT3, CellEvent Caspase-3/7 Green Detection Reagent | Real-time imaging of caspase activation kinetics in live cells | Enables single-cell analysis and temporal dynamics of apoptosis |
Diagram 2: Experimental Workflow for Evaluating Pro-Apoptotic Agonists. This flowchart outlines a standardized research pipeline from initial in vitro screening to in vivo validation of caspase-targeting therapeutics.
Targeting caspase activation pathways with pro-apoptotic agonists represents a rationally designed strategy to reactivate the innate cell death program in cancer cells. While significant progress has been made with agents like BH3 mimetics and SMAC mimetics, several challenges remain, including drug resistance, tumor heterogeneity, and on-target toxicities [44] [7]. Future directions in the field will likely focus on biomarker-driven patient selection, rational combination therapies (e.g., BH3 mimetics with conventional chemotherapy or targeted agents), and the development of novel protein degradation approaches such as PROTACs that target anti-apoptotic proteins for ubiquitin-mediated degradation [45]. Furthermore, emerging understanding of death pathway plasticity—whereby tumors shift between apoptotic and non-apoptotic cell death mechanisms under therapeutic pressure—highlights the need for polypharmacology approaches that simultaneously engage multiple nodes within the cell death regulatory network [44] [2]. As our knowledge of caspase biology and its intricate regulation continues to expand, so too will our ability to design more effective and selective pro-apoptotic therapies for cancer treatment.
This whitepaper examines the therapeutic potential of isoginkgetin (IGG), a natural biflavonoid, for targeting caspase cascade activation in cancer cells. We explore IGG's multifaceted mechanisms of action, focusing on its ability to induce apoptosis through JNK-mediated caspase activation, inhibit proteasome function, and modulate key signaling pathways. The analysis synthesizes current research findings from in vitro studies across various cancer types, including oral squamous cell carcinoma, melanoma, and hepatocellular carcinoma, providing a comprehensive technical resource for researchers and drug development professionals working on caspase-directed therapeutics.
Caspases (cysteine-dependent aspartate-specific proteases) are central regulators of programmed cell death (PCD), functioning as critical executioners in both apoptotic and inflammatory cell death pathways [2] [1]. These enzymes exist as inactive zymogens in cells and undergo proteolytic activation in response to specific death signals. Caspases can be broadly categorized as initiators (caspase-2, -8, -9, -10) that launch the death signal and executioners (caspase-3, -6, -7) that dismantle cellular structures [16] [2]. The activation mechanism differs between these categories: initiator caspases are activated by dimerization induced by proximity in multiprotein complexes, while executioner caspases require proteolytic cleavage by initiator caspases for activation [16].
The extrinsic apoptosis pathway begins with caspase-8 activation at the death-inducing signaling complex (DISC), while the intrinsic pathway involves caspase-9 activation through the Apaf-1 apoptosome complex following mitochondrial cytochrome c release [16] [1]. Both pathways converge on the activation of executioner caspases-3 and -7, which cleave numerous cellular substrates including PARP, lamins, and cytoskeletal proteins, leading to the characteristic morphological changes of apoptosis [1]. Beyond their traditional roles in apoptosis, recent evidence indicates caspases participate in crosstalk between various PCD pathways, including pyroptosis and PANoptosis, highlighting their complex regulatory networks in cellular homeostasis and disease pathogenesis [12] [2].
Isoginkgetin: Source, Structure, and Known Bioactivities
Isoginkgetin is a naturally occurring biflavonoid originally isolated from the leaves of Ginkgo biloba and other medicinal plants such as Metasequoia glyptostroboides [46] [47]. As a biflavonoid, IGG consists of two linked flavone subunits, which contributes to its enhanced bioactivity compared to monomeric flavonoids [48]. This compound has demonstrated diverse pharmacological properties including anti-inflammatory, anti-bacterial, anti-fungal, and notably, broad-spectrum anti-cancer activities [48] [47].
Previous research has identified multiple mechanisms contributing to IGG's anti-cancer effects. It functions as an effective inhibitor of pre-mRNA splicing and transcription elongation, disrupting essential cellular processes in cancer cells [46]. Additionally, IGG has been shown to inhibit matrix metalloproteinase-9 (MMP-9) production, thereby reducing tumor invasion and metastasis potential [46] [49]. More recently, IGG was identified as a natural proteasome inhibitor, directly inhibiting the chymotrypsin-like, trypsin-like, and caspase-like activities of the 20S proteasome core particle [47]. This proteasome inhibition leads to accumulation of polyubiquitinated proteins, endoplasmic reticulum stress, and ultimately apoptosis through disrupted protein homeostasis [47].
Molecular Mechanisms of Isoginkgetin-Induced Caspase Activation
JNK-Dependent Apoptosis in Oral Squamous Cell Carcinoma
Recent investigations have elucidated the specific molecular pathways through which IGG activates caspase cascades. In oral squamous cell carcinoma (OSCC) cell lines (HSC-3 and SCC-9), IGG treatment significantly diminished cell viability and induced apoptotic cell death in a dose-dependent manner [46]. The anti-apoptotic proteins cellular inhibitor of apoptosis 1 (cIAP-1) and X-linked inhibitor of apoptosis protein (XIAP) were decreased in IGG-treated cells, accompanied by increased cleavage and activation of caspases [46].
A pivotal finding was that IGG-induced caspase activation occurs primarily through the JNK signaling pathway. When OSCC cells were treated with IGG alongside a specific JNK kinase inhibitor (JNK-IN-8), the activation of caspase cascades was significantly reduced, establishing a functional connection between JNK activity and caspase activation during IGG-induced apoptosis [46]. This JNK-dependent mechanism represents a targeted approach to caspase cascade induction in cancer cells.
MAPK/ERK Activation in Melanoma Cells
In A375 melanoma cells, IGG exposure resulted in concentration-dependent decreases in cell viability and induced characteristic apoptotic morphology [49]. Western blot analysis confirmed PARP cleavage, a hallmark of caspase activity, at all concentrations tested (25-100 μM), with more pronounced cleavage observed at higher concentrations [49]. Mechanistic investigation revealed that IGG treatment induced phosphorylation of ERK, suggesting potential involvement of the MAPK signaling pathway in IGG-mediated apoptosis [49]. The phosphorylated ERK was detected at 12 hours post-treatment and enhanced after 24 hours, indicating delayed activation that correlates with the timing of apoptotic induction rather than survival signaling [49].
Proteasome Inhibition and Protein Homeostasis Disruption
IGG functions as a natural proteasome inhibitor, directly binding to and inhibiting the chymotrypsin-like, trypsin-like, and caspase-like activities of the 20S proteasome core particle [47]. This inhibition leads to accumulation of polyubiquitinated protein aggregates that colocalize with the adaptor protein p62 and components of the endoplasmic reticulum-associated degradation (ERAD) pathway [47]. The resulting disruption of protein homeostasis places considerable burden on lysosomal and autophagic machinery, ultimately leading to cancer cell death [47]. IGG treatment also activates TFEB, a master regulator of lysosome biogenesis, suggesting broader impacts on cellular catabolic processes beyond direct caspase activation [47].
Quantitative Analysis of Isoginkgetin Efficacy Across Cancer Models
Cytotoxicity Profiles
Table 1: Isoginkgetin Cytotoxicity Across Cancer Cell Lines
| Cancer Type | Cell Line | IC50 Value | Treatment Duration | Assay Method | Reference |
|---|---|---|---|---|---|
| Oral Squamous Cell Carcinoma | HSC-3 | ~40 μM | 24 hours | MTT | [46] |
| Oral Squamous Cell Carcinoma | SCC-9 | ~40 μM | 24 hours | MTT | [46] |
| Melanoma | A375 | 50 μM | 48 hours | XTT | [49] |
| Cervical Cancer | HeLa | <10 μM | 24 hours | Multiple | [47] [49] |
Apoptosis Induction Metrics
Table 2: Apoptotic Markers Activated by Isoginkgetin Treatment
| Apoptotic Marker | Effect of IGG | Experimental System | Detection Method | Reference |
|---|---|---|---|---|
| PARP Cleavage | Increased cleavage (89 kDa fragment) | A375 melanoma cells | Western Blot | [49] |
| Caspase-3 Cleavage | Increased activation | HeLa cells, OSCC cells | Western Blot | [46] [47] |
| Annexin V Positivity | Increased early apoptosis | OSCC cells | Flow Cytometry | [46] |
| cIAP-1/XIAP | Decreased expression | OSCC cells | Apoptosis Array, Western Blot | [46] |
| JNK Phosphorylation | Increased activation | OSCC cells | Western Blot with JNK inhibition | [46] |
| ERK Phosphorylation | Delayed activation (12-24h) | A375 melanoma cells | Western Blot | [49] |
Experimental Methodologies for Assessing Caspase Activation
Cell Viability and Cytotoxicity Assays
MTT/XTT Colorimetric Assays: Cells are cultured in the presence of IGG at various concentrations (typically 5-80 μM) for 24-48 hours. MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide) or XTT solution is added to cells and incubated for several hours. The formazan product yield is spectrophotometrically measured at 563 nm (MTT) or 450 nm (XTT), with viability calculated relative to untreated controls [46] [49].
Flow Cytometric Analysis of Apoptosis: Cells exposed to various IGG concentrations are assessed for phosphatidylserine externalization using FITC-labeled Annexin V and propidium iodide (PI) staining. The proportions of Annexin V+/PI- (early apoptotic) and Annexin V+/PI+ (late apoptotic/necrotic) cells are quantified using flow cytometry [46].
Protein Analysis Techniques
Western Blotting for Caspase Activation: Protein lysates from IGG-treated and control cells are separated by SDS-PAGE and transferred to membranes. Specific primary antibodies detect cleaved caspase-3, cleaved caspase-8, cleaved caspase-9, PARP cleavage, and phosphorylation status of JNK, ERK, and other signaling molecules. β-actin serves as a loading control. Densitometric analysis quantifies protein expression changes [46] [49].
Apoptosis Proteome Profiling: The Proteome Profiler Human Apoptosis Array Kit enables simultaneous detection of 35 apoptosis-related proteins. Membrane arrays are incubated with cell lysates, followed by chemiluminescent detection. Pixel density for apoptotic markers is normalized to reference spots to identify significantly altered proteins in response to IGG treatment [46].
Immunofluorescence Staining: Cells grown on coverslips are treated with IGG, fixed, permeabilized, and stained with primary antibodies against cleaved caspase-3 followed by fluorescence-labeled secondary antibodies. Imaging by fluorescence microscopy visualizes caspase activation at the single-cell level [46].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Studying Isoginkgetin Mechanisms
| Reagent/Category | Specific Examples | Research Application | Function in Experimental Design |
|---|---|---|---|
| IGG Source | Sigma-Aldrich (≥98% purity HPLC grade) | All studies | Standardized compound for treatment experiments |
| Cell Lines | HSC-3, SCC-9 (OSCC); A375 (melanoma); HeLa (cervical cancer) | In vitro models | Representative cancer models for efficacy testing |
| Viability Assays | MTT, XTT, CCK-8 | Cytotoxicity screening | Quantify dose-response and IC50 values |
| Apoptosis Detection | FITC Annexin V/PI Kit (BD Biosciences) | Flow cytometry | Distinguish apoptotic vs. necrotic cell death |
| Pathway Inhibitors | JNK-IN-8 (JNK inhibitor); U0126 (MEK inhibitor); SB203580 (p38 inhibitor) | Mechanistic studies | Establish signaling pathway dependencies |
| Antibody Panels | Anti-cleaved caspase-3, -8, -9; Anti-PARP; Anti-phospho-JNK, ERK, p38 | Western blot, immunofluorescence | Detect caspase activation and signaling events |
| Apoptosis Arrays | Proteome Profiler Human Apoptosis Array (R&D Systems) | Multiplex protein screening | Simultaneously monitor 35 apoptosis-related proteins |
| Proteasome Activity | Proteasome-Glo Assay System | Enzymatic activity measurement | Quantify chymotrypsin-like, trypsin-like, and caspase-like proteasome activities |
Isoginkgetin represents a promising natural compound for targeted caspase cascade activation in cancer therapy. Its ability to induce apoptosis through multiple mechanisms—JNK-dependent caspase activation in OSCC, ERK-mediated apoptosis in melanoma, and proteasome inhibition across various cancer types—highlights its potential as a multi-modal therapeutic agent. The concentration-dependent and time-dependent effects observed across studies provide important insights for dosage considerations in future therapeutic development.
Further research should focus on optimizing IGG's bioavailability, evaluating synergistic combinations with conventional chemotherapeutic agents, and validating efficacy in in vivo models. Additionally, structural analogs of IGG may offer opportunities for enhanced potency and selectivity. As natural compounds continue to provide valuable scaffolds for drug discovery, isoginkgetin stands as a compelling candidate for advancing caspase-targeted cancer therapeutics.
Navigating Experimental and Biological Hurdles in Caspase Signaling
Radiotherapy (RT) is a cornerstone of cancer treatment, with its efficacy primarily attributed to the induction of lethal DNA damage in tumor cells. A central executor of this radiation-induced cell death is the caspase family of cysteine proteases, traditionally recognized for their role in orchestrating programmed cell death pathways, notably apoptosis [4] [1]. However, emerging research reveals a paradoxical function: caspase activity can also initiate potent pro-survival signaling that paradoxically contributes to radioresistance [50]. This phenomenon represents a significant adaptive mechanism in tumors, where sublethal caspase activation, rather than culminating in cell death, triggers reparative and proliferative responses. This review, framed within broader research on caspase cascade activation, delineates the mechanisms of this paradox and explores experimental approaches to exploit it for therapeutic benefit, aiming to provide researchers and drug development professionals with a strategic framework to overcome this challenge in oncology.
Mechanistic Insights: How Caspase Signaling Promotes Survival
The paradoxical pro-survival signaling emanating from caspase activation manifests through several key molecular mechanisms. These pathways allow cancer cells to not only survive the cytotoxic insult of radiotherapy but potentially emerge with a more aggressive phenotype.
- Apoptosis-Induced Proliferation (AIP): A critically documented phenomenon where cells undergoing apoptosis secrete mitogenic factors that stimulate the proliferation of neighboring, surviving cells. Real-time imaging using stable fluorescent reporter systems has dynamically captured this compensatory proliferation following apoptotic events, identifying the release of growth factors like epidermal growth factors (EGF) and interleukin-6 (IL-6) as key mediators. This process is increasingly recognized as a driver of tumor repopulation following cytotoxic therapies like radiotherapy [38].
- Suppression of Immunogenic Cell Death: In nasopharyngeal carcinoma (NPC), the DNA repair protein RAD51 has been demonstrated to promote radioresistance by directly suppressing Caspase-8-mediated pyroptosis. Pyroptosis is a highly inflammatory form of cell death that can stimulate robust anti-tumor immunity. By inhibiting this Caspase-8-dependent pathway, RAD51 allows cells to evade this immunogenic fate, thereby sustaining tumor survival post-radiation. Inhibition of RAD51 was shown to reduce cell viability and re-sensitize cells to radiation through the reinstatement of this pyroptotic pathway [50].
- Modulation of Other Programmed Cell Death Pathways: Caspases can act as molecular switches between different cell death modalities. For instance, Caspase-8 is known to cleave and inhibit key components of the necroptosis pathway, such as RIPK1 and RIPK3, thereby shutting down this alternative cell death pathway [1]. Furthermore, caspases-3 and -7 can cleave gasdermin D (GSDMD) at a non-canonical site, preventing its oligomerization and subsequent execution of pyroptosis [1]. This hierarchical control allows a cell that has initiated a caspase response to avoid more inflammatory death outcomes, which could be detrimental to the tumor microenvironment in the short term, but may ultimately contribute to survival and resistance.
Table 1: Key Caspases Implicated in Pro-Survival Signaling and Radioresistance
| Caspase | Primary Context | Pro-Survival Mechanism | Experimental Evidence |
|---|---|---|---|
| Caspase-8 | Nasopharyngeal Carcinoma | Inhibition of pyroptotic cell death; Suppression of necroptosis [1] [50]. | RAD51 inhibits Caspase-8-mediated pyroptosis; Caspase-8 cleaves RIPK1/RIPK3 [50] [1]. |
| Caspase-3/-7 | General Apoptosis | Cleavage and inactivation of GSDMD, suppressing pyroptosis; Potential role in AIP [1] [38]. | Non-canonical cleavage of GSDMD at D87; Real-time imaging of AIP [1] [38]. |
| Initiator Caspases (e.g., -9) | DNA Damage Response | Activation of effector caspases at sublethal thresholds, potentially triggering repair responses [51] [52]. | Association with DNA damage repair pathways and cell cycle checkpoints [51] [52]. |
Experimental Approaches and Methodologies
Investigating the paradoxical roles of caspases requires a combination of live-cell imaging, precise molecular inhibition, and assessment of cell death modalities. Below are detailed protocols for key methodologies cited in recent literature.
Real-Time Tracking of Caspase Activation and Apoptosis-Induced Proliferation
The development of stable fluorescent reporter cell systems enables the dynamic visualization of caspase activity and its downstream consequences at single-cell resolution [38].
Protocol:
- Reporter System Generation: Stably transduce cells of interest with a lentiviral construct encoding a caspase-3/7 biosensor (e.g., a ZipGFP-based reporter where GFP fluorescence is reconstituted upon DEVD cleavage) alongside a constitutive fluorescent marker (e.g., mCherry) for cell presence normalization [38].
- Model Establishment: Adapt the reporter cells to physiologically relevant 2D and 3D culture systems, including patient-derived organoids (PDOs) or spheroids embedded in Cultrex or similar matrices [38].
- Treatment and Live-Cell Imaging:
- Induce apoptosis using a relevant stimulus (e.g., chemotherapeutic agent like carfilzomib or radiation).
- Use time-lapse live-cell imaging (e.g., over 80-120 hours) to track GFP fluorescence (caspase-3/7 activation) and mCherry (cell presence) simultaneously.
- To confirm caspase dependence, include a control group co-treated with a pan-caspase inhibitor like zVAD-FMK (20-50 µM) [38].
- Detecting Apoptosis-Induced Proliferation (AIP):
- Following treatment and imaging, add a fluorescent proliferation dye (e.g., CellTrace) to the culture medium.
- Continue live-cell imaging to monitor dye dilution in the surviving, non-apoptotic (GFP-negative) cell population. Proliferating cells will show a decrease in fluorescence intensity, indicating AIP [38].
Dissecting Caspase-8-Mediated Pyroptosis in Radioresistance
This protocol outlines the methodology to investigate the link between DNA repair, caspase-8, and pyroptosis, as demonstrated in nasopharyngeal carcinoma [50].
Protocol:
- Cell Culture and Grouping:
- Utilize a radioresistant cancer cell line (e.g., CNE2 for NPC).
- Divide cells into multiple experimental groups:
- Control (vehicle)
- Recombinant human RAD51 protein (e.g., 200 ng/mL) to enhance DNA repair
- RAD51 inhibitor (B02, e.g., 20 µM)
- Caspase-8 inhibitor (Z-IETD-FMK, e.g., 40 µM)
- Combination groups (e.g., rhRAD51 + Z-IETD-FMK; B02 + Z-IETD-FMK) [50].
- Viability and Cytotoxicity Assay:
- After 24 hours of treatment, assess cell viability using a Cell Counting Kit-8 (CCK-8). Add 10 µL of CCK-8 solution per well in a 96-well plate, incubate for 2 hours, and measure the optical density at 450 nm [50].
- Quantify cytotoxicity by measuring Lactate Dehydrogenase (LDH) release into the culture supernatant, a marker of pyroptotic membrane rupture [50].
- Molecular Analysis:
- Perform Western blot analysis on cell lysates to probe for key proteins:
- Cleaved Caspase-8 (indicative of activation)
- Cleaved GSDMD (the active fragment executing pyroptosis)
- Full-length and cleaved IL-1β (a pro-inflammatory cytokine processed during pyroptosis) [50].
- The expected result of RAD51 overexpression is reduced levels of cleaved Caspase-8, cleaved GSDMD, and cleaved IL-1β, which can be rescued by RAD51 inhibition.
- Perform Western blot analysis on cell lysates to probe for key proteins:
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for Investigating Caspase-Mediated Radioresistance
| Reagent / Tool | Function / Specificity | Example Application |
|---|---|---|
| ZipGFP Caspase-3/7 Reporter | Irreversible, fluorescent biosensor activated upon DEVD cleavage. Minimizes background in live cells [38]. | Real-time tracking of apoptosis kinetics and AIP in 2D/3D models [38]. |
| Caspase-8 Inhibitor (Z-IETD-FMK) | Potent, cell-permeable, and irreversible inhibitor of Caspase-8 [50]. | Probing the role of Caspase-8 in extrinsic apoptosis and its cross-talk with pyroptosis [50]. |
| RAD51 Inhibitor (B02) | Small-molecule inhibitor that disrupts RAD51 nucleoprotein filament formation, impeding homologous recombination [50]. | Sensitizing tumor cells to radiotherapy by blocking DNA repair and promoting Caspase-8-dependent pyroptosis [50]. |
| Pan-Caspase Inhibitor (zVAD-FMK) | Broad-spectrum, cell-permeable caspase inhibitor. | Confirming the caspase-dependence of an observed cell death phenotype [38]. |
| Recombinant RAD51 Protein | Active protein used to enhance homologous recombination repair in cells [50]. | Studying the effect of enhanced DNA repair on cell death modality switching and radioresistance [50]. |
| GSK484 | Potent and selective inhibitor of PAD4-mediated neutrophil extracellular trap formation (NETosis) [53]. | Investigating the role of GSDMD-mediated NETosis in pathological models like thoracic aortic dissection [53]. |
Visualizing the Paradox: Caspase Signaling Networks in Radioresistance
The following diagram synthesizes the complex signaling network through which caspase activation can lead to both cell death and pro-survival outcomes, contributing to radioresistance.
Caspase-Mediated Survival Signaling Network: This diagram illustrates the core paradox in radioresistance. Ionizing radiation causes DNA damage, which can trigger sublethal caspase activation. Instead of leading to death, this activation promotes survival via two major axes: 1) Apoptosis-Induced Proliferation (AIP), where dying cells secrete mitogens that stimulate neighboring cell growth, and 2) Suppression of Alternative Cell Death, exemplified by RAD51-mediated inhibition of Caspase-8-driven pyroptosis, thereby preventing immunogenic cell death.
A hallmark of cancer is the ability of malignant cells to evade programmed cell death, or apoptosis. This evasion is a fundamental contributor to both tumorigenesis and resistance to anti-cancer therapies [54] [55]. The apoptotic process is primarily executed by a cascade of proteolytic enzymes known as caspases. However, their activity is tightly regulated by two key protein families: the B-cell lymphoma 2 (Bcl-2) family and the Inhibitor of Apoptosis Proteins (IAPs) [1] [56]. These proteins act as critical gatekeepers of cell survival, and their dysregulation represents a common mechanism by which cancer cells avoid destruction. Understanding the intricate balance between pro-survival and pro-death signals is essential for developing novel therapeutic strategies to overcome apoptosis evasion. This review examines the roles of IAPs and Bcl-2 family proteins within the broader context of caspase cascade activation, detailing their mechanisms of action and the promising targeted therapies designed to counteract their pro-survival functions.
The Caspase Cascade: Core Executor of Apoptosis
Caspases are cysteine-aspartic proteases that serve as the central executioners of apoptosis. They are synthesized as inactive zymogens (pro-caspases) and become activated through proteolytic cleavage, initiating a cascade that leads to the controlled dismantling of the cell [1]. This process occurs through two principal pathways.
The extrinsic pathway is triggered by extracellular death ligands binding to cell surface death receptors, leading to the assembly of the Death-Inducing Signaling Complex (DISC) and activation of initiator caspases-8 and -10 [1] [57]. The intrinsic pathway, also known as the mitochondrial pathway, is activated by internal cellular stresses. This pathway is regulated by the Bcl-2 protein family and results in mitochondrial outer membrane permeabilization (MOMP), releasing cytochrome c into the cytosol [54] [58]. Cytochrome c then facilitates the formation of the apoptosome, a complex that activates initiator caspase-9 [1]. Both pathways converge on the activation of executioner caspases-3, -6, and -7, which cleave a wide array of cellular substrates, culminating in the characteristic morphological changes of apoptosis, including cell shrinkage, chromatin condensation, and formation of apoptotic bodies [1].
Recent research has revealed that caspase activation is not always a binary switch for death. Sublethal executioner caspase activation (ECA) can occur, promoting processes such as cellular proliferation and regeneration without triggering apoptosis [30] [14]. For instance, in liver regeneration following partial hepatectomy, sublethal ECA in hepatocytes promotes proliferation through the JAK/STAT3 pathway rather than cell death [30]. Similarly, in Drosophila olfactory receptor neurons, the executioner caspase Drice can be activated non-lethally when sequestered near the plasma membrane by the cell adhesion protein Fasciclin 3, leading to functional neuronal modulation without apoptosis [14]. These non-apoptotic roles add a layer of complexity to the regulation of caspase activity and its functional outcomes.
The following diagram illustrates the core caspase cascade and its intersection with key regulatory systems.
The Bcl-2 Protein Family: Regulators of Mitochondrial Apoptosis
The Bcl-2 protein family is the primary regulator of the intrinsic apoptotic pathway. These proteins control mitochondrial outer membrane permeabilization (MOMP), the critical step that commits a cell to death [58] [55]. The family is defined by the presence of Bcl-2 Homology (BH) domains and is categorized into three functional groups based on their structure and activity.
- Anti-apoptotic proteins: These include BCL-2, BCL-XL, BCL-W, MCL-1, and BFL-1. They possess four BH domains (BH1-BH4) and function to promote cell survival by preventing MOMP [54] [55]. They act as guardians by binding and neutralizing their pro-apoptotic counterparts.
- Pro-apoptotic effector proteins: This group, primarily BAX and BAK, contains multiple BH domains. In response to apoptotic signals, they undergo conformational changes, oligomerize, and form pores in the mitochondrial outer membrane, leading to MOMP and the release of cytochrome c and other pro-apoptotic factors [58] [1].
- BH3-only proteins: These are pro-apoptotic sensors (e.g., BIM, BID, PUMA, BAD, NOXA) that share only the BH3 domain. They are activated by various cellular stresses and transmit death signals by either neutralizing anti-apoptotic proteins or directly activating BAX and BAK, depending on the model [58] [55].
The prevailing "indirect activation" model posits that the balance between these factions determines cellular fate. In healthy cells, anti-apoptotic proteins bind and restrain the pro-apoptotic effectors BAX and BAK. Upon stress, BH3-only proteins are activated and bind to the anti-apoptotic proteins, displacing BAX/BAK and allowing them to initiate MOMP [58]. The release of cytochrome c promotes apoptosome formation and caspase-9 activation, while SMAC/DIABLO is released to counteract IAPs [55] [56].
Table 1: Core Members of the Bcl-2 Protein Family
| Subfamily Group | Protein Name | Structural Domains | Primary Function |
|---|---|---|---|
| Anti-apoptotic | BCL-2 | BH1, BH2, BH3, BH4 | Binds and inhibits pro-apoptotic BAX/BAK; inhibits caspase activity [54] |
| BCL-XL | BH1, BH2, BH3, BH4 | Promotes cell survival; high expression in cancer linked to therapy resistance [54] [55] | |
| MCL-1 | BH1, BH2, BH3 | Rapidly turned over; critical for survival of many cancers [55] | |
| Pro-apoptotic Effectors | BAX | BH1, BH2, BH3 | Upon activation, oligomerizes to permeabilize mitochondrial membrane [58] [1] |
| BAK | BH1, BH2, BH3 | Similar function to BAX; constitutively located at mitochondria [58] | |
| BH3-only Proteins | BIM, PUMA, tBID | BH3 | "Activators" that bind and inhibit all anti-apoptotic proteins; potent inducers of apoptosis [58] |
| BAD, NOXA | BH3 | "Sensitizers" that selectively inhibit subsets of anti-apoptotic proteins (e.g., BAD targets BCL-2, BCL-XL) [58] |
Inhibitor of Apoptosis Proteins (IAPs): Direct Caspase Suppressors
IAPs are a family of proteins characterized by the presence of at least one Baculoviral IAP Repeat (BIR) domain, which facilitates protein-protein interactions [56]. Their primary role is to directly suppress the caspase cascade, acting as a final barrier to apoptosis execution. The most clinically significant members include XIAP, cIAP1, cIAP2, and survivin [56] [59].
- XIAP is the most potent direct caspase inhibitor. It binds to and suppresses the activity of executioner caspases-3 and -7, as well as initiator caspase-9, through its BIR2 and BIR3 domains, effectively halting the apoptotic process [56] [59].
- cIAP1 and cIAP2 function differently from XIAP. They primarily act as E3 ubiquitin ligases, regulating cell survival and inflammatory signaling pathways, most notably the NF-κB pathway. By ubiquitinating key components in the TNFR1 signaling complex, they promote pro-survival gene expression and prevent the formation of pro-apoptotic complexes containing caspase-8 [56].
- Survivin is highly expressed in most cancers and is associated with poor prognosis. It inhibits apoptosis by binding to and stabilizing XIAP, preventing its degradation, and may also directly interfere with caspase activity, particularly caspase-9 [59].
A critical endogenous antagonist of IAPs is the mitochondrial protein SMAC/DIABLO. Upon MOMP, SMAC is released into the cytosol where it binds to the BIR domains of IAPs, displacing them from caspases and thereby relieving the inhibition and permitting apoptosis to proceed [56]. This natural antagonism has become a key therapeutic target.
Table 2: Key Members of the Inhibitor of Apoptosis (IAP) Family
| IAP Member | Key Domains | Mechanism of Action | Role in Cancer |
|---|---|---|---|
| XIAP | BIR2, BIR3, RING | Directly binds and inhibits caspases-3, -7, and -9 [56] [59] | Confers resistance to chemotherapy; prognostic marker in AML and renal cancer [56] |
| cIAP1/cIAP2 | BIR, RING (E3 ligase) | Regulates NF-κB signaling via RIPK1 ubiquitination; suppresses caspase-8 activation [56] | Amplified in cancers; promotes cell survival and resistance to death ligands [56] |
| Survivin | BIR | Forms complex with XIAP to stabilize it; may inhibit caspase-9 [59] | Overexpressed in nearly all cancers; correlates with poor prognosis [59] |
| BRUCE (Apollon) | BIR, RING (E3 ligase) | Ubiquitinates and degrades caspase-9; inhibits SMAC/DIABLO [59] | Large IAP; overexpression linked to therapy resistance [59] |
Therapeutic Targeting: BH3-Mimetics and SMAC-Mimetics
The pivotal role of Bcl-2 and IAPs in apoptosis evasion makes them attractive therapeutic targets. The development of small-molecule inhibitors that mimic the function of endogenous pro-apoptotic proteins has emerged as a promising anti-cancer strategy.
BH3-Mimetics
BH3-mimetics are designed to mimic the BH3 domain of pro-apoptotic proteins. By binding to the hydrophobic groove of anti-apoptotic Bcl-2 proteins, they disrupt their interaction with pro-apoptotic effectors, thereby unleashing apoptosis [54] [55].
- Venetoclax (ABT-199): This first-in-class, highly selective BCL-2 inhibitor has transformed the treatment of hematological malignancies. It potently displaces pro-apoptotic proteins from BCL-2, leading to BAX/BAK activation and apoptosis [54] [55]. It is approved for chronic lymphocytic leukemia (CLL) and acute myeloid leukemia (AML).
- Navitoclax (ABT-263): An earlier inhibitor that targets BCL-2, BCL-XL, and BCL-W. Its clinical development was limited by on-target thrombocytopenia caused by BCL-XL inhibition, which is essential for platelet survival [55].
- Next-Generation Inhibitors: Targeting MCL-1 and BCL-XL specifically remains an active area of research. However, development is challenging due to on-target toxicities: cardiac toxicity for MCL-1 inhibitors and thrombocytopenia for BCL-XL inhibitors. Novel approaches like PROTACs (Proteolysis Targeting Chimeras) and antibody-drug conjugates are being explored to achieve tumor-specific inhibition [55].
SMAC-Mimetics
SMAC-mimetics are synthetic compounds that mimic the N-terminal tetrapeptide of endogenous SMAC. They bind to the BIR domains of IAPs, primarily cIAP1/2 and XIAP, triggering several pro-apoptotic events [56] [59].
- They induce the auto-ubiquitination and rapid proteasomal degradation of cIAP1 and cIAP2 [56].
- By degrading cIAPs, they block NF-κB activation and facilitate the formation of a pro-apoptotic complex (ripoptosome) containing RIPK1 and caspase-8, leading to caspase-8 activation [56].
- They antagonize XIAP's inhibition of caspases, thereby restoring caspase activity and allowing apoptosis to proceed [56].
Several SMAC-mimetics (e.g., LCL161, Debio 1143, birinapant) have entered clinical trials. While their efficacy as single agents has been limited, they show significant promise in combination with other therapies, such as immune checkpoint blockade, due to their immuno-modulatory properties [56].
The following diagram summarizes the mechanisms of these targeted therapies.
Experimental Approaches and Research Tools
Studying the complex interactions within apoptotic pathways requires sophisticated experimental models and reagents. Below is a summary of key methodologies and tools used in this field.
Key Experimental Protocols
- Monitoring Executioner Caspase Activation (ECA) In Vivo: The mCasExpress system is a transgenic mouse lineage tracing model used to identify and track cells that have experienced ECA. In this system, a membrane-tethered FLP recombinase is fused to a caspase cleavage site (DEVD). Upon caspase activation, FLP is released, translocates to the nucleus, and triggers permanent expression of a reporter gene (e.g., ZsGreen). This allows for the sensitive detection and fate mapping of cells with sublethal or lethal caspase activity in tissues like the regenerating liver [30].
- Proximity Labeling for Caspase-Interacting Proteins: TurboID is an engineered biotin ligase that biotinylates proximal proteins in vivo. By generating CRISPR knock-in flies or mice where TurboID is fused to the C-terminus of an executioner caspase (e.g., Drice in Drosophila), researchers can identify the caspase's interactome and proximal proteins under normal and stress conditions. This method revealed that the pro-form of Drice is proximal to cell membrane proteins like Fasciclin 3, providing insight into how caspases can be activated in a subcellularly restricted manner for non-lethal functions [14].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Apoptosis and Caspase Research
| Reagent / Tool | Function and Application | Experimental Example |
|---|---|---|
| mCasExpress Mice | Lineage tracing system for in vivo detection of cells that have experienced executioner caspase activation [30] | Identifying hepatocytes with sublethal ECA during liver regeneration after partial hepatectomy [30] |
| Caspase::TurboID lines | Proximity-dependent biotinylation to map the interactome and microenvironment of caspases in vivo [14] | Identifying Fasciclin 3 as a proximal protein to executioner caspase Drice in Drosophila brains [14] |
| BH3-Mimetics (Venetoclax) | Selective small-molecule inhibitor of BCL-2; used to probe BCL-2 dependency and induce apoptosis in cancer models [54] [55] | In vitro and in vivo studies to trigger intrinsic apoptosis in BCL-2-dependent leukemia and lymphoma cells [55] |
| SMAC-Mimetics (Birinapant) | Small-molecule antagonists of IAPs; used to sensitize cancer cells to apoptosis induced by TNFα or chemotherapeutics [56] | In vitro assays to demonstrate ripoptosome formation and caspase-8 activation in SM-treated cancer cell lines [56] |
| XIAP Inhibitors | Compounds that specifically target the BIR domain of XIAP to relieve caspase inhibition [56] | Restoring caspase-3 and -7 activity in cell-free systems or cultured cells with high XIAP expression [59] |
The evasion of apoptosis is a critical step in oncogenesis and therapy resistance, largely governed by the intricate interplay between the Bcl-2 family, IAPs, and the caspase cascade. The Bcl-2 family acts as the primary decision-maker for mitochondrial apoptosis, while IAPs function as direct suppressors of the caspase executioners. The successful clinical translation of venetoclax validates the therapeutic potential of reactivating the intrinsic apoptotic pathway. Ongoing efforts to target MCL-1 and BCL-XL, alongside the development of SMAC-mimetics to counteract IAP-mediated resistance, highlight the dynamic nature of this field. Furthermore, the discovery of non-lethal caspase functions underscores the complexity of this regulatory network. A deep understanding of these mechanisms, coupled with advanced research tools, continues to drive the development of novel and effective pro-apoptotic cancer therapies, offering hope for overcoming the formidable challenge of apoptosis evasion.
Executioner caspases-3 and -7 have long been considered functionally redundant proteases with overlapping roles in apoptotic cell death. However, emerging evidence from genetic knockout models reveals a more complex relationship characterized by both redundant and unique physiological functions. This whitepaper synthesizes findings from key studies utilizing caspase-3, caspase-7, and double knockout models to delineate the extent and limitations of their functional redundancy. We examine quantitative data on embryonic viability, tissue-specific phenotypes, and biochemical specificity alongside methodological protocols for generating and analyzing these models. The integration of structural analyses, substrate profiling, and phenotypic characterization provides a framework for understanding how these executioner caspases coordinate cell death execution while maintaining specialized roles in development, homeostasis, and disease pathogenesis. This comprehensive analysis informs targeted therapeutic strategies aimed at modulating caspase activity in cancer, inflammatory disorders, and neurodegenerative conditions.
Caspase-3 and caspase-7 are homologous cysteine aspartic proteases traditionally classified as executioner caspases that proteolytically dismantle cells during apoptosis [60] [2]. These enzymes share significant structural similarity and are both activated by initiator caspases (caspase-8, -9, -10) through the extrinsic and intrinsic apoptotic pathways [61] [62]. They recognize similar tetrapeptide sequences (DEXD) and cleave hundreds of cellular substrates, leading to the characteristic morphological changes of apoptosis [63] [2].
The concept of functional redundancy between caspase-3 and caspase-7 emerged from their coordinated activation during apoptosis and overlapping substrate specificity. However, detailed biochemical and genetic studies have revealed nuanced differences in their regulation, substrate preferences, and biological functions [63]. The generation and characterization of caspase-3 knockout (Casp3⁻/⁻), caspase-7 knockout (Casp7⁻/⁻), and caspase-3/7 double knockout (DKO) mice have been instrumental in deciphering the extent and limitations of this functional redundancy [63]. This whitepaper synthesizes current understanding of how these executioner caspases coordinate apoptotic execution while maintaining specialized functions in development and tissue homeostasis, providing critical insights for therapeutic targeting in human diseases.
Comparative Analysis of Knockout Model Phenotypes
Viability and Developmental Outcomes
Table 1: Viability and Developmental Characteristics of Caspase Knockout Models
| Genotype | Embryonic Viability | Postnatal Survival | Key Developmental Defects | References |
|---|---|---|---|---|
| Casp3⁻/⁻ | Viable | Normal lifespan | Brain overgrowth, neural precursor accumulation | [60] [63] |
| Casp7⁻/⁻ | Viable | Normal lifespan | Generally normal development | [63] |
| Casp3⁻/⁻;Casp7⁻/⁻ (DKO) | Lethal | Perinatal lethality | Cardiac malformations, defective heart development | [63] |
The viability patterns observed in caspase knockout models provide compelling evidence for both redundant and unique functions. While single knockout mice for either caspase-3 or caspase-7 are viable with normal lifespans, double knockout mice die shortly after birth due to profound developmental defects [63]. This genetic interaction demonstrates that caspase-3 and caspase-7 perform overlapping essential functions during embryogenesis, yet the viability of single knockouts indicates that either protease can sufficiently execute these critical processes.
Caspase-3 deficiency specifically disrupts brain development, resulting in notable brain overgrowth and accumulation of neural precursors due to impaired apoptosis during neurogenesis [60]. In contrast, caspase-7 knockout mice display generally normal development without prominent brain abnormalities, suggesting that caspase-3 bears primary responsibility for apoptosis in the developing nervous system [63]. The perinatal lethality observed in DKO mice highlights non-redundant functions in cardiac development, indicating that both caspases are indispensably required for proper heart formation, either through complementary functions or specific substrates that cannot be processed by either protease alone.
Tissue and Cell-Type Specific Apoptosis Deficiencies
Table 2: Tissue and Stimulus-Specific Apoptotic Defects in Knockout Models
| Cell Type/Tissue | Apoptotic Stimulus | Casp3⁻/⁻ Phenotype | Casp7⁻/⁻ Phenotype | DKO Phenotype | References |
|---|---|---|---|---|---|
| Thymocytes | FasL, TNF-α | Moderately resistant | Moderately resistant | Highly resistant (FasL); Variable resistance | [63] |
| Thymocytes | UV, staurosporine, etoposide | Moderately resistant | Moderately resistant | Highly resistant | [63] |
| Mouse Embryonic Fibroblasts (MEFs) | FasL | Mild resistance | Moderate resistance | Highly resistant | [63] |
| MEFs | UV radiation | Mild resistance | Moderate resistance | Highly resistant | [63] |
| Eye lens | Developmental | Anterior pole cataracts | Grossly normal | Severe cataracts | [63] |
The analysis of apoptotic competence across different cell types and stimuli reveals complex patterns of redundancy and specialization. In thymocytes, DKO mice show dramatically enhanced resistance to diverse apoptotic stimuli including death receptor activation (FasL, TNF-α) and genotoxic stress (UV radiation, etoposide) compared to single knockouts [63]. However, the preservation of some sensitivity to Fas-induced death in DKO thymocytes suggests the existence of alternative death mechanisms that operate independently of both executioner caspases.
Notable cell-type specific differences emerge when comparing fibroblast and thymocyte responses. While DKO thymocytes remain partially sensitive to Fas-induced apoptosis, DKO MEFs exhibit nearly complete resistance to the same stimulus [63]. This cell-type variation indicates that the requirement for executioner caspases is influenced by cell-intrinsic factors and alternative death pathways. The differential phenotype in eye development further underscores functional specialization, with caspase-3 being primarily responsible for lens fiber cell death and cataract formation, while caspase-7 deficiency alone does not produce this abnormality [63].
Molecular Mechanisms Underlying Redundancy and Specificity
Structural and Biochemical Differences
Despite their classification as executioner caspases with shared activation mechanisms, caspase-3 and caspase-7 exhibit distinct biochemical properties that contribute to their functional differences. Both proteases are synthesized as inactive zymogens containing an N-terminal prodomain followed by large (p20) and small (p11) subunits [60] [63]. Activation requires proteolytic cleavage at specific aspartic acid residues to generate the mature heterotetrameric enzyme [63].
Structural analyses reveal subtle but significant differences in their active sites and surface charges that influence substrate selection and catalytic efficiency [63]. Caspase-3 demonstrates broader substrate specificity and more potent catalytic activity toward many classical apoptosis substrates compared to caspase-7 [63]. This enhanced promiscuity may explain why caspase-3 deficiency produces more pronounced defects in certain apoptotic contexts, particularly in the development of the brain and eye.
Biochemical studies using recombinant enzymes and cell lysates have identified substrates with distinct cleavage preferences. For example, the cochaperone p23 is more efficiently cleaved by caspase-7, while other substrates including specific nuclear proteins show preference for caspase-3 [63]. These differential cleavage activities likely underlie the specialized functions observed in knockout models and contribute to the non-redundant requirements in specific developmental contexts.
Differential Regulation and Activation Mechanisms
Beyond intrinsic biochemical differences, caspase-3 and caspase-7 are subject to distinct regulatory mechanisms that influence their cellular functions. In inflammatory contexts, caspase-7 activation requires caspase-1 inflammasomes, while caspase-3 processing proceeds independently of caspase-1 [63]. This differential regulation is particularly relevant in macrophages exposed to bacterial pathogens or inflammatory stimuli, where caspase-7 plays specialized roles in restricting intracellular bacterial replication and promoting phagosome-lysosome fusion.
The transcriptional regulation of these caspases also differs significantly. The caspase-3 gene promoter contains several Sp1-like sequences and is regulated by transcription factors including Sp1, p73, HIF-1α, Stat3, FOXO1, and c-Jun:ATF2 [60]. Caspase-3 expression shows tissue-specific and age-dependent variation, with epigenetic mechanisms including DNA methylation and histone acetylation influencing its transcription in certain contexts [60]. In contrast, less is known about the specific transcriptional regulation of caspase-7, though differences in expression patterns have been documented.
Figure 1: Differential Activation and Functions of Caspase-3 and Caspase-7. Caspase-3 and caspase-7 share activation pathways through caspase-8 and -9 but show differential regulation in inflammatory contexts where caspase-7 can be activated by caspase-1. They execute overlapping apoptotic functions but maintain specialized roles in specific tissues and processes.
Experimental Approaches and Methodologies
Generation of Knockout Models
The genetic mouse models central to understanding caspase redundancy have been generated through standard gene targeting techniques in embryonic stem cells. The foundational approach involves replacing critical exons of the Caspx gene with a neomycin resistance cassette for positive selection [63]. For caspase-3 knockout mice, targeting typically disrupts exon 2-3, which contains essential catalytic residues [60]. Caspase-7 knockouts are generated by deleting exons encoding the active site cysteine [63]. Double knockout mice are produced through sequential breeding of single knockout lines and genotyping protocols include PCR amplification of tail DNA with primer sets distinguishing wild-type and targeted alleles.
Embryonic fibroblasts (MEFs) derived from these models provide essential tools for in vitro studies. Primary MEFs are isolated from E13.5-E14.5 embryos following standard protocols: dissected embryos are decapitated, eviscerated, trypsinized, and plated in DMEM supplemented with 10% FBS [63]. Early passage MEFs (passages 2-4) are utilized for apoptosis assays to maintain consistency and prevent senescence-related artifacts. Immortalized MEF lines may be established using SV40 large T antigen transduction for long-term studies.
Apoptosis Assessment Methodologies
Standardized apoptosis assays are critical for comparative analysis across knockout models. Key methodologies include:
DNA Fragmentation Analysis: Cells are treated with apoptotic stimuli (e.g., 1μM staurosporine, 100ng/mL anti-Fas antibody with cycloheximide, 20μM etoposide, or UV irradiation at 50-100 J/m²). After 6-24 hours, DNA is extracted and separated on 1.5-2% agarose gels to detect the characteristic oligonucleosomal ladder pattern [60] [64]. Caspase-3-deficient MCF-7 cells show impaired DNA fragmentation, a defect rescued by caspase-3 reconstitution [64].
Phosphatidylserine Externalization: Cells are stained with fluorescently labeled Annexin V in binding buffer and analyzed by flow cytometry. Propidium iodide exclusion distinguishes early apoptotic (Annexin V+/PI-) from late apoptotic/necrotic (Annexin V+/PI+) populations [60] [65].
Morphological Assessment: Apoptotic cells are identified by characteristic shrinkage, membrane blebbing, and nuclear condensation using phase-contrast or fluorescence microscopy after Hoechst 33342 or DAPI staining [64]. Caspase-3 deficiency specifically impairs cellular shrinkage and blebbing despite preservation of other death features [64].
Caspase Activity Assays: Fluorogenic substrates (DEVD-AFC for executioner caspases, IETD-AFC for initiator caspases) are used to measure caspase activity in cell lysates. Cleavage releases the fluorescent AFC moiety, quantified using a fluorometer [63].
Proteomic Approaches to Substrate Identification
Recent advances in proteomics have enabled comprehensive identification of caspase-specific substrates. Quantitative mass spectrometry analyses compare protein cleavage patterns in wild-type versus caspase-deficient cells under basal and stress conditions [65]. The standard workflow includes:
Cell Culture and Treatment: Wild-type, Casp3⁻/⁻, Casp7⁻/⁻, and DKO cells are treated with low-dose stress stimuli (e.g., 10μM cisplatin) or apoptotic doses (e.g., 50μM cisplatin) for 4-24 hours [65].
Protein Extraction and Digestion: Cells are lysed in denaturing buffer, proteins are reduced, alkylated, and digested with trypsin.
Peptide Labeling and Fractionation: Tandem mass tag (TMT) labeling enables multiplexed quantification, followed by high-pH reverse-phase fractionation to reduce complexity [65].
LC-MS/MS Analysis: Fractionated peptides are analyzed by liquid chromatography coupled to tandem mass spectrometry.
Data Processing: Proteome Discoverer or similar platforms identify proteins and quantify abundance changes. Cleavage events are detected through altered peptide intensity and the presence of novel cleavage site peptides [65].
This approach has revealed that caspase-3 and caspase-7 regulate distinct proteolytic landscapes, with approximately 92 proteins cleaved during mild stress conditions and 453 during apoptosis, with most events dependent on these executioner caspases [65].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Caspase Functional Studies
| Reagent Category | Specific Examples | Applications | Considerations |
|---|---|---|---|
| Knockout Models | Casp3⁻/⁻, Casp7⁻/⁻, DKO mice | In vivo development, tissue-specific apoptosis | C57BL/6 background shows milder phenotypes than other strains |
| Cell Lines | MCF-7 (caspase-3 deficient) | Structure-function studies, reconstitution experiments | Require verification of caspase-3 deficiency status |
| Chemical Inhibitors | Z-VAD-FMK (pan-caspase), DEVD-CHO (executioner) | Specific pathway inhibition, rescue experiments | Concentration optimization needed to avoid off-target effects |
| Activity Assays | Fluorogenic substrates (DEVD-AFC, IETD-AFC) | Enzyme kinetics, inhibitor screening | Measure initial velocity for accurate comparisons |
| Antibodies | Anti-cleaved caspase-3, anti-PARP, anti-caspase-7 | Western blot, immunohistochemistry | Validation in knockout cells essential for specificity |
| Apoptosis Inducers | Staurosporine, etoposide, FasL, TNF-α | Pathway-specific activation | Dose-response establishment critical for interpretation |
Implications for Therapeutic Development
The nuanced understanding of caspase redundancy and specificity has significant implications for therapeutic strategies targeting cell death pathways. In cancer, where apoptosis evasion is common, restoring caspase activity represents a promising approach. However, the functional redundancy between caspase-3 and caspase-7 suggests that targeting both executioner caspases may be necessary in certain contexts, while their specialized functions indicate tissue-specific considerations [63].
In inflammatory diseases, the distinct regulation of caspase-7 by inflammasomes positions it as a potential target for modulating inflammation without globally disrupting apoptosis [63]. Caspase-7 deficiency protects against LPS-induced lethality in endotoxemia models, while caspase-3 deficiency does not, highlighting the potential for selective therapeutic intervention [63].
Neurodegenerative conditions characterized by excessive apoptosis might benefit from caspase-3-specific inhibition, given its predominant role in neuronal cell death [60] [63]. However, the perinatal lethality of DKO mice suggests that complete executioner caspase inhibition would have severe consequences, emphasizing the need for carefully calibrated therapeutic approaches.
Figure 2: Experimental Framework for Studying Caspase Redundancy. This workflow outlines key considerations for designing and interpreting studies on caspase-3 and caspase-7 functional redundancy, from model selection to data interpretation.
The integration of data from caspase-3 and caspase-7 knockout models reveals a sophisticated relationship between these executioner caspases characterized by contextual redundancy and specialized functions. While they perform overlapping roles in many apoptotic contexts—evidenced by the perinatal lethality of DKO mice—each protease maintains unique responsibilities in specific developmental processes, tissue homeostasis, and stress responses.
Future research should focus on identifying the specific substrates that mediate the essential functions of these caspases during development, particularly through proteomic approaches in tissue-specific contexts. The development of conditional and inducible DKO models would enable bypassing of embryonic lethality and facilitate analysis of executioner caspase functions in adult tissues and disease models. Additionally, structural studies comparing caspase-3 and caspase-7 with their specific substrates may reveal the molecular basis for their differential selectivity, informing the design of targeted inhibitors.
As caspase-targeted therapies advance toward clinical application, the nuanced understanding of functional redundancy between these executioner caspases will be essential for developing effective and safe therapeutic strategies. The evidence from knockout models suggests that neither complete redundancy nor complete specificity adequately describes their relationship, but rather a sophisticated division of labor that has evolved to ensure both robust cell death execution and specialized regulation in specific biological contexts.
Caspases (cysteine-dependent aspartate-specific proteases) have been historically characterized as fundamental executioners of programmed cell death, particularly apoptosis. However, contemporary research has unveiled a complex landscape of non-apoptotic functions that extend far beyond their traditional cell death roles [26] [66]. This paradigm shift recognizes caspases as multifunctional regulators of critical physiological processes, including cellular differentiation, immune regulation, and inflammatory signaling [2]. The traditional classification of caspases into simplistic categories of "apoptotic" and "inflammatory" has proven insufficient to capture their functional diversity, necessitating a more nuanced understanding of their roles in cellular homeostasis [2] [26].
Within the broader context of caspase cascade activation and executioner functions research, it is now evident that caspases operate along a functional continuum, where the cellular outcome is determined by the spatiotemporal context, intensity, and duration of activation [26]. At sublethal activation levels, caspases mediate essential physiological processes without triggering cell death, representing a sophisticated regulatory mechanism that maintains cellular homeostasis while retaining the capacity to initiate death pathways when necessary [26] [30]. This whitepaper comprehensively examines the molecular mechanisms, experimental evidence, and therapeutic implications of non-apoptotic caspase functions in differentiation and inflammation, providing researchers and drug development professionals with a cutting-edge technical resource in this rapidly evolving field.
Molecular Mechanisms of Non-Apoptotic Caspase Activity
The Functional Continuum Model
The functional continuum model proposes that caspase activity exists along a dynamic gradient rather than functioning in a binary on/off state [26]. This model elegantly explains how the same proteases can mediate diverse cellular outcomes based on activation context:
- Homeostatic Functions: At basal activity levels, caspases regulate routine cellular processes including synaptic plasticity, cell cycle progression, and metabolic regulation [26].
- Defensive Functions: At intermediate activation levels, caspases participate in immune surveillance and inflammatory responses without immediately triggering cell death [26].
- Remodeling Functions: Approaching the apoptotic threshold, caspases execute structural remodeling including axon pruning and tissue reorganization [67] [26].
- Lethal Functions: Only when activation surpasses a critical threshold and becomes widespread do caspases initiate irreversible apoptotic or pyroptotic cell death [26].
This model fundamentally challenges the traditional view of caspases as mere "death executors" and reframes them as multifunctional integrators of cellular homeostasis whose functional output is determined by the precise interplay of activation intensity, spatial localization, and temporal dynamics [26].
Mechanisms of Caspase Confinement and Regulation
The restriction of caspase activity to non-lethal functions requires sophisticated regulatory mechanisms that prevent uncontrolled propagation of proteolytic signaling:
- Spatial Compartmentalization: Caspase activation is frequently confined to specific subcellular compartments, such as dendritic spines in neurons or specific mitochondrial domains, effectively limiting substrate accessibility [67]. For instance, during axon guidance, caspase-3 activation is restricted to growth cones, preventing propagation to the cell body and subsequent apoptosis [68].
- Inhibitor Proteins: Endogenous caspase inhibitors, particularly XIAP (X-linked Inhibitor of Apoptosis Protein), tightly regulate caspase activity by directly binding to and inhibiting caspases, establishing a threshold that must be overcome for full activation [67] [69].
- Limited Proteolysis: Unlike the widespread proteolysis characteristic of apoptosis, non-apoptotic caspase activity typically involves cleavage of a restricted subset of substrates, often with higher specificity than during cell death [26] [68].
- Feedback Loops: Auto-regulatory feedback mechanisms enable fine-tuning of caspase activity, allowing for precise control over the duration and intensity of signaling [5].
Structural Determinants of Caspase Function
Caspase functionality is intrinsically linked to structural features that determine activation mechanisms and substrate specificity:
- Pro-domain Architecture: Initiator caspases contain long pro-domains (either CARD or DED domains) that facilitate recruitment to and activation within multiprotein complexes, while executioner caspases have short pro-domains and are primarily activated by proteolytic cleavage [2] [27].
- Active Site and Exosite Interactions: Substrate recognition is mediated not only by the canonical active site that recognizes the P1 aspartic acid residue but also through exosite interactions that confer additional specificity [2].
- Tetrameric Assembly: Active caspases typically form tetramers consisting of two heterodimers, with the interface between subunits playing a crucial role in regulation and activation [2].
Caspases in Cellular Differentiation
Neuronal Differentiation and Circuit Refinement
The nervous system represents a paradigm for non-apoptotic caspase functions, with compelling evidence demonstrating essential roles in neuronal development, connectivity, and plasticity:
- Axon Guidance and Dendritogenesis: Caspase-3 and caspase-8 are required for NCAM-mediated neurite outgrowth, with caspase-3 mediating cytoskeletal remodeling through cleavage of proteins like spectrin and Gap43 [68]. Similarly, caspase-9 regulates axon routing through cleavage of semaphorin 7A, a protein essential for proper axonal pathfinding [68].
- Developmental Pruning: Caspase activity is essential for the elimination of excessive axons and dendrites during neural circuit refinement [67]. In Drosophila, the initiator caspase DRONC and effector caspases are required for dendritic pruning of class IV sensory neurons during metamorphosis [67]. In mammalian retinal ganglion cells, caspase-3 and caspase-6 mediate activity-dependent axon pruning to refine the eye-specific projection map [67].
- Synaptic Plasticity: Caspase-3 regulates dendritic spine remodeling through selective cleavage of the synaptic scaffold protein SynGAP1, while caspase-6 modulates synaptic function through cleavage of Drebrin within dendrites [26]. This localized caspase activity enables structural and functional plasticity without compromising neuronal survival.
Table 1: Caspase Functions in Neuronal Development and Plasticity
| Caspase | Neuronal Function | Molecular Substrates | Experimental Models |
|---|---|---|---|
| Caspase-3 | Axon guidance, spine remodeling | Spectrin, Gap43, SynGAP1 | Mouse hippocampal neurons, chick auditory brainstem [68] |
| Caspase-6 | Synaptic plasticity, axon pruning | Drebrin, undefined pruning substrates | Mouse RGCs, Drosophila sensory neurons [67] [26] |
| Caspase-8 | Neurite outgrowth | Cytoskeletal regulators | Mouse hippocampal neurons [68] |
| Caspase-9 | Axon routing | Semaphorin 7A | Mouse sensory neurons [68] |
| DRONC (Drosophila) | Dendritic pruning | Undefined dendrite-specific substrates | Drosophila class IV sensory neurons [67] |
Non-Neuronal Differentiation Programs
Beyond the nervous system, caspases regulate differentiation across diverse tissue types:
- Stem Cell Differentiation: Caspase-3 activation is required for efficient differentiation of embryonic stem cells, with sublethal activity facilitating the transition from pluripotency to committed lineages [26] [66].
- Keratinocyte Differentiation: Terminal differentiation of epidermal keratinocytes involves caspase-3-mediated cleavage of specific substrates that enable the structural transformations necessary for barrier function [67].
- Myoblast Differentiation: Skeletal muscle differentiation requires caspase-3 activity for the coordinated remodeling of the cytoskeleton and downregulation of proliferation signals [66].
- Erythroblast Differentiation: Erythrocyte maturation involves caspase-mediated enucleation and clearance of organelles, a specialized form of differentiation that shares mechanistic features with but is distinct from apoptosis [67].
The role of caspases in differentiation programs highlights their function as master regulators of cellular identity and tissue architecture, coordinating complex remodeling events that extend far beyond their traditional association with cell death.
Caspases in Inflammation and Immunity
Canonical and Non-Canonical Inflammatory Roles
While caspase-1, -4, -5, and -11 are traditionally classified as inflammatory caspases based on their roles in cytokine maturation and pyroptosis, emerging evidence demonstrates that apoptotic caspases also significantly contribute to inflammatory regulation:
- Cytokine Processing: Inflammatory caspases directly process pro-IL-1β and pro-IL-18 into their active forms through proteolytic cleavage within inflammasome complexes [2] [27]. Additionally, caspase-8 can contribute to cytokine maturation under specific conditions, particularly when canonical inflammasome signaling is compromised [2].
- Gasdermin-Mediated Pyroptosis: Inflammatory caspases (caspase-1, -4, -5, -11) and certain apoptotic caspases (caspase-3, -8) can cleave gasdermin family proteins to release their N-terminal pore-forming domains, executing pyroptotic cell death [2] [27]. The specific gasdermin family member cleaved varies by caspase, with caspase-1, -4, -5, and -11 targeting GSDMD, while caspase-3 cleaves GSDME [2] [27].
- Regulation of Immune Cell Function: Caspase-8 serves as a key regulator of T-cell activation and proliferation, with its enzymatic activity required for optimal immune responses [26]. Additionally, caspase-8 negatively regulates necroptosis in immune cells by cleaving RIPK1 and RIPK3, thereby maintaining inflammatory homeostasis [27] [69].
Novel Inflammatory Functions of Apoptotic Caspases
Traditional apoptotic caspases exhibit surprising inflammatory functions that blur the historical classification boundaries:
- Caspase-8 in Innate Immunity: Caspase-8 functions as a molecular scaffold in addition to its proteolytic function, regulating innate immune signaling complexes including the RIPoptosome and PANoptosome [2] [27]. It can directly cleave inflammatory substrates including IL-1β under specific conditions and serves as a critical regulator of NLRP3 inflammasome activation [2].
- Executioner Caspases in Immune Surveillance: Sublethal caspase-3 activation in the tumor microenvironment processes specific IL-18 fragments that translocate to the nucleus and activate immune surveillance signals, facilitating recognition and elimination of cancer cells [26].
- Caspase-6 in Inflammation: Previously considered primarily an apoptotic executioner, caspase-6 regulates GSDMB-mediated pyroptosis and contributes to inflammatory signaling in specific contexts [27].
Table 2: Inflammatory Functions of Caspase Family Members
| Caspase | Traditional Classification | Inflammatory Functions | Molecular Mechanisms |
|---|---|---|---|
| Caspase-1 | Inflammatory | Pyroptosis induction, cytokine maturation | Cleaves GSDMD, pro-IL-1β, pro-IL-18 within inflammasomes [2] [27] |
| Caspase-4/5/11 | Inflammatory | Non-canonical pyroptosis | Directly cleaves GSDMD in response to intracellular LPS [2] [27] |
| Caspase-8 | Apoptotic initiator | Cytokine processing, necroptosis regulation, PANoptosis | Cleaves GSDMC, IL-1β, RIPK1/RIPK3; scaffolds PANoptosomes [2] [27] |
| Caspase-3 | Apoptotic executioner | GSDME-mediated pyroptosis, immune surveillance | Cleaves GSDME at DMPD site; processes IL-18 fragments in TME [2] [26] |
| Caspase-6 | Apoptotic executioner | GSDMB regulation | Cleaves GSDMB at D91 to prevent pyroptotic activation during apoptosis [27] |
PANoptosis: Integrated Cell Death in Inflammation
PANoptosis represents an emerging concept in caspase biology, describing an integrated inflammatory cell death pathway that incorporates components from apoptosis, pyroptosis, and necroptosis [2]. This pathway is driven by multimeric protein complexes called PANoptosomes that simultaneously activate multiple caspases (including caspase-1, -3, -6, -7, and -8) alongside RIP kinases to execute inflammatory cell death [2]. PANoptosis exemplifies the functional convergence of caspases historically assigned to distinct pathways and highlights the limitations of rigid caspase classification systems.
Experimental Methodologies and Research Tools
Key Experimental Models and Approaches
The investigation of non-apoptotic caspase functions employs sophisticated experimental systems that enable precise monitoring and manipulation of caspase activity:
- Live-Cell Imaging and FRET Sensors: Fluorescence resonance energy transfer (FRET)-based caspase biosensors enable real-time monitoring of caspase activation dynamics in living cells, revealing the spatiotemporal regulation of non-apoptotic signaling [5]. These approaches have demonstrated that sublethal caspase activation occurs in discrete subcellular compartments with kinetics distinct from apoptotic activation.
- Genetic Lineage Tracing Systems: The mCasExpress transgenic mouse system enables permanent lineage tracing of cells that have experienced executioner caspase activation (ECA) through a FLP-recombinase-based genetic switch [30]. This system demonstrated that hepatocytes with ECA predominantly survive and proliferate during liver regeneration, providing direct evidence for non-lethal functions in mammalian tissue homeostasis.
- Compartmentalized Neuronal Cultures: Microfluidic chamber systems that physically separate neuronal cell bodies from axons enable the study of localized caspase activation during pruning and regeneration responses [67]. These models demonstrated that caspase activation restricted to axons is sufficient to mediate pruning without triggering somal apoptosis.
- Caspase Inhibition Strategies: Pharmacological inhibitors (zVAD-fmk, Q-VD-OPh), dominant-negative caspase mutants, and genetic knockout models enable functional dissection of specific caspases in complex biological processes [67] [30]. Importantly, the interpretation of these experiments requires consideration of potential compensatory mechanisms and caspase functional redundancy.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Studying Non-Apoptotic Caspase Functions
| Reagent / Tool | Function/Application | Key Features and Considerations |
|---|---|---|
| mCasExpress Mouse Model | Lineage tracing of cells with executioner caspase activation | Uses FLP-recombinase under control of DEVD caspase cleavage site; enables identification of cells that survive ECA [30] |
| FRET-Based Caspase Sensors | Real-time monitoring of caspase activity in live cells | SCAT3, SCAT8, and executioner caspase sensors; provide temporal resolution of activation kinetics [5] |
| Compartmentalized Microfluidic Chambers | Study of spatially restricted caspase activation in neurons | Enables separate manipulation of cell bodies and axons; crucial for pruning studies [67] |
| Caspase-Specific Inhibitors | Functional interrogation of specific caspases | zDEVD-fmk (caspase-3), zVEID-fmk (caspase-6), zIETD-fmk (caspase-8); require validation of specificity [67] |
| Caspase Cleavage-Specific Antibodies | Detection of activated caspases and cleaved substrates | Anti-cleaved caspase-3, anti-cleaved PARP; enable histological mapping of caspase activity [67] [30] |
| Photoactivatable Caspase Constructs | Spatiotemporally precise caspase activation | Allows targeted activation in specific subcellular compartments; establishes causality [68] |
Signaling Pathway Visualizations
Non-Apoptotic Caspase Signaling Pathways
Therapeutic Implications and Future Directions
Therapeutic Targeting Strategies
The expanding understanding of non-apoptotic caspase functions reveals novel therapeutic opportunities while highlighting potential challenges:
- Context-Dependent Caspase Modulation: Therapeutic strategies must account for the dual nature of caspases in survival and death signaling. In neurodegenerative diseases, selective inhibition of pathological caspase activation without disrupting homeostatic functions may require drugs that target specific caspase conformational states or subcellular localization [26].
- Conformation-Specific Inhibitors: The development of inhibitors that stabilize specific caspase conformations represents a promising approach for selective modulation. For caspase-6, conformation-specific inhibitors can block its pro-metastatic function while preserving neuroprotective activity [26].
- Tissue-Regenerative Applications: Enhancing sublethal caspase activity may promote regeneration in contexts like liver repair, where controlled caspase-3 activation stimulates hepatocyte proliferation through JAK/STAT3 signaling [30].
- Inflammatory Disease Modulation: Targeting the inflammatory functions of caspases, particularly in PANoptosis, may provide new avenues for treating autoinflammatory and autoimmune disorders [2].
Research Gaps and Future Perspectives
Despite significant advances, critical questions remain in the field of non-apoptotic caspase biology:
- Threshold Determination: The molecular mechanisms that establish the threshold between sublethal and lethal caspase activation remain incompletely understood [26] [5].
- Substrate Specificity Mechanisms: How caspases achieve functional specificity in different contexts, particularly how they select distinct substrate repertoires during homeostatic versus pathological signaling, requires further investigation [2] [26].
- Caspase Cross-Talk: The complex interactions between different caspase family members in integrated processes like PANoptosis necessitate more comprehensive models that account for functional redundancy and compensation [2].
- Single-Cell Dynamics: Advanced imaging and single-cell analysis techniques will be essential to fully resolve the spatiotemporal regulation of caspase activity in heterogeneous cellular populations [5].
The paradigm of caspase function has evolved dramatically from a narrow focus on cell death execution to a sophisticated understanding of their multifunctional roles in cellular homeostasis. Caspases function as versatile signaling molecules that coordinate critical processes in differentiation and inflammation through mechanisms that are precisely regulated in space, time, and intensity. The functional continuum model provides a valuable framework for understanding how these proteases can mediate diverse outcomes ranging from synaptic plasticity to inflammatory cell death. As research continues to unravel the complexity of non-apoptotic caspase functions, new therapeutic opportunities will emerge for manipulating these pathways in cancer, neurodegenerative diseases, inflammatory disorders, and regenerative medicine. The future of caspase research lies in developing context-specific modulators that can precisely target pathological signaling while preserving homeostatic functions, representing both a formidable challenge and extraordinary opportunity for translational innovation.
Caspases, cysteine-aspartate-specific proteases, are master regulators of programmed cell death (PCD) and inflammation, playing critical roles in development, homeostasis, and disease pathogenesis [1]. Therapeutically modulating caspase activity represents a promising approach for treating cancer, neurodegenerative disorders, inflammatory diseases, and infectious diseases [7] [70]. However, the development of clinically effective caspase inhibitors has faced significant challenges, primarily due to the high structural conservation among caspase family members and their multifaceted roles in diverse cellular processes [7]. A "one-size-fits-all" approach to caspase inhibition has proven inadequate, as broad-spectrum inhibitors often cause unintended side effects by simultaneously affecting multiple caspases with distinct functions [7]. This technical guide examines the molecular basis for the specificity challenge and outlines rational strategies for developing precisely targeted caspase therapeutics.
Caspase Classification and Functional Overlap
Evolving Classification Systems
Traditional caspase classification based solely on apoptotic versus inflammatory functions has become outdated as research reveals extensive functional overlap and crosstalk between cell death pathways [71] [2].
Table 1: Caspase Classification Systems
| Classification Basis | Categories | Member Caspases | Key Characteristics |
|---|---|---|---|
| Traditional Function | Inflammatory | Caspase-1, -4, -5, -11 | Activate cytokines; mediate pyroptosis |
| Apoptotic Initiators | Caspase-2, -8, -9, -10 | Initiate apoptosis through extrinsic/intrinsic pathways | |
| Apoptotic Executioners | Caspase-3, -6, -7 | Execute apoptosis by cleaving cellular substrates | |
| Pro-domain Structure | CARD-containing | Caspase-1, -2, -4, -5, -9, -11, -12 | Feature caspase activation and recruitment domains |
| DED-containing | Caspase-8, -10 | Contain death effector domains | |
| Short/No pro-domain | Caspase-3, -6, -7 | Executioner caspases with minimal pro-domains | |
| Substrate Specificity | Group I | Caspase-1, -4, -14 | Preference for (W/L/Y)EHD motif |
| Group II | Caspase-2, -3, -7 | Preference for DEXD motif | |
| Group III | Caspase-6, -8, -9, -10 | Preference for (L/V/I)EXD motif |
Molecular Cross-Talk and Pathway Interconnectivity
The discovery of PANoptosis, an inflammatory cell death pathway incorporating features of pyroptosis, apoptosis, and necroptosis, highlights the functional interconnectivity between caspase family members [72] [2]. Caspase-8 exemplifies this complexity, functioning as a molecular switch that can promote extrinsic apoptosis, inhibit necroptosis, and under certain conditions, drive inflammatory responses [72]. This multifaceted nature means that therapeutic inhibition of a single caspase may trigger compensatory or alternative cell death pathways, potentially limiting efficacy or causing unexpected side effects [7].
Figure 1: Caspase Pathway Interconnectivity. Caspases function within highly interconnected cell death networks. Inhibition of one pathway (e.g., caspase-8-mediated apoptosis) can activate alternative pathways (e.g., necroptosis), creating challenges for therapeutic targeting.
Structural Mechanisms of Caspase Activity and Inhibition
Molecular Architecture and Active Site Conservation
All caspases share a conserved structural fold comprising a large (p20) and small (p10) subunit that form a heterodimer, with the active site situated at the interface between these subunits [2]. The catalytic mechanism relies on a cysteine-histidine dyad that cleaves substrate proteins C-terminal to aspartic acid residues [1] [2]. This active site conservation across the caspase family presents the fundamental challenge for developing specific inhibitors, as the substrate-binding pocket shows limited structural variation between different caspases.
Exploiting Exosites for Enhanced Specificity
Beyond the conserved active site, emerging research reveals that exosites – secondary substrate-binding regions distant from the catalytic core – contribute significantly to substrate recognition and specificity [2]. These exosite interactions occur between distinct surface patches on caspases and complementary regions on substrates, providing a potential mechanism for achieving therapeutic specificity. For instance, the interaction between caspase-7 and GSDMB involves both active site cleavage and exosite binding, suggesting that targeting these secondary interaction sites could yield more specific inhibitors [2].
Current Therapeutic Landscape and Specificity Challenges
Classes of Caspase Inhibitors
Table 2: Caspase Inhibitor Classes and Specificity Profiles
| Inhibitor Class | Representative Compounds | Mechanism of Action | Specificity Challenges | Development Status |
|---|---|---|---|---|
| Peptide-based | Z-VAD-FMK (pan-caspase) | Irreversible binding to catalytic cysteine | Low specificity; off-target effects | Preclinical research |
| Ac-YVAD-CHO (caspase-1) | Reversible active site binding | Cross-reactivity with related caspases | Research tool | |
| Peptidomimetic | VX-740 (caspase-1) | Reversible transition state analog | Limited clinical efficacy | Phase II (terminated) |
| VX-765 (caspase-1) | Prodrug converted to active inhibitor | Liver toxicity at high doses | Phase II (terminated) | |
| IDN-6556 (pan-caspase) | Irreversible covalent binding | Narrow therapeutic window | Phase II (terminated) | |
| Non-peptidic | Isatin sulfonamides | Reversible active site binding | Moderate specificity for caspase-3 | Preclinical optimization |
| Natural Inhibitors | CrmA (viral) | Serpin family; inhibits caspase-1, -8 | Broad specificity across proteases | Research tool |
| p35 (baculovirus) | Substrate analog inhibits multiple caspases | Excludes caspase-9 | Research tool | |
| XIAP (cellular) | BIR domains inhibit caspase-3, -7, -9 | Regulated by SMAC/DIABLO | Therapeutic target |
Clinical Lessons from Failed Candidates
Several caspase inhibitors have advanced to clinical trials but failed due to specificity-related issues:
VX-740 (Pralnacasan): This caspase-1 inhibitor showed promise for rheumatoid arthritis but was terminated due to liver toxicity observed in animal models at high doses, possibly due to off-target effects [7].
VX-765 (Belnacasan): A second-generation caspase-1 inhibitor demonstrated efficacy in inflammatory conditions but similarly faced termination due to hepatic toxicity, highlighting the challenge of achieving sufficient specificity for chronic administration [7].
IDN-6556 (Emricasan): This pan-caspase inhibitor reached Phase II trials for liver diseases but encountered issues with inadequate efficacy and potential side effects from extended treatment, underscoring the limitations of broad-spectrum caspase inhibition [7].
These clinical failures demonstrate that achieving an optimal balance between specificity, efficacy, and safety remains the central challenge in caspase-targeted therapeutic development.
Strategic Approaches for Enhancing Specificity
Structure-Based Drug Design
Advanced structural biology techniques, including X-ray crystallography and cryo-electron microscopy, provide detailed atomic-level information about caspase-inhibitor complexes [2]. This structural information enables rational drug design strategies that exploit subtle differences in caspase active sites and exosite regions. For instance, the variation in S2 and S4 substrate-binding subsites across caspases offers opportunities for designing selective inhibitors that fit particular caspase active sites while excluding others [2].
Targeting Allosteric Sites and Protein-Protein Interactions
Rather than targeting the conserved active site, alternative approaches focus on:
Allosteric inhibition: Identifying and targeting unique regulatory sites distant from the active center that modulate caspase activity through conformational changes.
Protein-protein interaction disruptors: Developing molecules that interfere with specific caspase recruitment into multiprotein complexes like inflammasomes or death-inducing signaling complexes (DISCs) [72]. For example, compounds that disrupt the interaction between caspase-8 and its adaptor protein FADD could achieve greater specificity than active site-directed inhibitors [72].
Context-Dependent Activation and Prodrug Strategies
Smart therapeutic designs that leverage disease-specific microenvironments can enhance specificity:
Activity-based probes that only become activated in the presence of specific caspase activities
Prodrug approaches that are selectively activated by disease-associated enzymes or conditions
Dual-targeting agents that require simultaneous presence of two pathological features for full activity
Experimental Protocols for Specificity Profiling
Comprehensive Specificity Screening
Rigorous specificity assessment is essential for developing targeted caspase therapies:
Protocol: Tiered Specificity Profiling
Primary Screening:
- Use fluorogenic substrate libraries with recombinant caspases
- Measure IC50 values against caspase-1 through -9
- Employ optimized reaction buffers for each caspase (e.g., 50 mM HEPES, 100 mM NaCl, 0.1% CHAPS, 10% sucrose, 10 mM DTT, pH 7.2)
Secondary Validation:
- Perform counter-screening against related proteases (cathepsins, granzymes, calpains)
- Assess cellular activity in caspase-specific reporter assays
- Evaluate selectivity in cell models of specific death pathways (apoptosis, pyroptosis)
Structural Confirmation:
- Determine co-crystal structures of inhibitor-caspase complexes
- Identify specific binding interactions and confirm mechanism of inhibition
Functional Validation in Disease-Relevant Models
Protocol: Cellular Efficacy and Specificity Assessment
Model Selection:
- Choose disease-relevant cell types (e.g., hepatocytes for liver disease, lymphocytes for inflammatory conditions)
- Employ specific death inducters: TNF-α+CHX for extrinsic apoptosis, STS for intrinsic apoptosis, nigericin for pyroptosis
Specificity Readouts:
- Monitor multiple cell death pathways in parallel (apoptosis: caspase-3/7 activation; pyroptosis: LDH release, GSDMD cleavage)
- Assess cytokine profiles (IL-1β for inflammasome activity, IL-18 for caspase-1 function)
- Evaluate morphological changes characteristic of specific death pathways
Rescue Experiments:
- Use genetic approaches (siRNA, CRISPR) to validate on-target effects
- Demonstrate dose-dependent protection with selective vs. pan-caspase inhibitors
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Caspase Specificity Research
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Activity Reporters | MitoCasp3 (caspase-3 biosensor) | Real-time monitoring of specific caspase activation in live cells | Requires confocal microscopy; specific subcellular localization |
| NucView 488 (caspase-3 substrate) | Fluorogenic detection of caspase-3/7 activity | Membrane-permeable; suitable for high-throughput screening | |
| Genetic Tools | CASP3-/- CASP7-/- DKO cells | Validation of caspase-specific inhibitor effects | Confirm complete knockout to avoid compensatory mechanisms |
| Inducible caspase expression systems | Controlled activation of specific caspase pathways | Titrate inducer concentration to achieve physiological levels | |
| Specific Inhibitors | Z-DEVD-FMK (caspase-3 inhibitor) | Selective blockade of caspase-3-like activity | Irreversible inhibitor; use appropriate vehicle controls |
| Z-IETD-FMK (caspase-8 inhibitor) | Inhibition of initiator caspase-8 | Verify specificity across caspase family members | |
| Antibody Reagents | Anti-cleaved caspase-3 (Asp175) | Specific detection of activated caspase-3 | Distinguishes active from pro-form; ideal for immunohistochemistry |
| Anti-cleaved caspase-8 (Asp387) | Detection of active caspase-8 | Confirms specific pathway activation in death receptor signaling | |
| Proximity Labeling | TurboID-caspase fusion constructs | Mapping caspase-proximal protein networks [14] | Identifies novel regulatory interactions and potential exosites |
Future Directions and Emerging Technologies
Single-Cell Caspase Profiling
Advanced single-cell technologies enable unprecedented resolution for studying caspase activation:
Mass cytometry (CyTOF) with metal-tagged caspase antibodies allows simultaneous monitoring of multiple caspases and cell death markers
Single-cell RNA sequencing reveals caspase expression patterns and identifies cell-type-specific responses to inhibition
Microfluidic platforms enable tracking of caspase dynamics in individual cells over time
Targeted Protein Degradation
PROTAC (Proteolysis-Targeting Chimeras) technology offers an alternative to conventional inhibition by directing specific caspases for ubiquitination and degradation. This approach could achieve greater specificity through the recruitment of caspase-specific binders coupled to E3 ligase recruiters.
CRISPR Screening for Context-Specific Essentials
Genome-wide CRISPR screens in the presence of caspase inhibitors can identify:
- Synthetic lethal interactions that enhance caspase inhibitor efficacy
- Resistance mechanisms and potential compensatory pathways
- Cell-type-specific factors that influence inhibitor sensitivity
Achieving therapeutic specificity in caspase targeting remains a formidable but surmountable challenge. Success will require integrated approaches combining structural biology, chemical optimization, and systems-level understanding of caspase network biology. Rather than pursuing universal caspase inhibitors, the field must develop context-specific modulators that account for the complex interplay between different cell death pathways. The strategies outlined in this technical guide provide a roadmap for developing the next generation of caspase-targeted therapeutics with enhanced specificity and improved clinical potential.
Validation, Specificity, and Cross-Talk in Caspase-Mediated Pathways
Substrate Specificity and Functional Redundancy among Executioner Caspases
Within the caspase cascade that regulates programmed cell death, the executioner caspases-3, -6, and -7 function as the terminal effectors responsible for the controlled dismantling of the cell. These proteases are synthesized as inactive zymogens and become activated through proteolytic cleavage by upstream initiator caspases within apoptotic signaling pathways [61] [73]. Once activated, they mediate the demolition phase of apoptosis through restricted proteolysis of hundreds of cellular proteins, leading to the characteristic biochemical and morphological changes associated with apoptotic cell death [74] [73]. While historically viewed as functionally redundant enzymes due to their overlapping sequence specificities toward synthetic peptide substrates, emerging evidence reveals significant functional distinctions, particularly between the primary executioners caspase-3 and caspase-7 [74]. This technical guide examines the molecular basis of executioner caspase specificity, their functional redundancy and specialization, and the experimental approaches for their study, framed within the broader context of caspase cascade activation research.
Molecular Basis of Caspase Specificity and Classification
Biochemical Mechanism of Substrate Recognition
Caspases are cysteine-dependent aspartate-specific proteases that cleave peptide bonds carboxyl-terminal to aspartic acid residues. Their catalytic mechanism relies on a conserved cysteine-histidine dyad within the active site [73]. Table 1 summarizes the key components of caspase substrate recognition.
Table 1: Caspase Substrate Recognition Components
| Component | Description | Functional Significance |
|---|---|---|
| P1 Position | Mandatory aspartic acid residue | Absolute requirement for caspase recognition and cleavage |
| P4 Position | Key determinant of caspase specificity | Primary residue defining substrate specificity groups |
| Specificity Pocket | Contains arginine residue that coordinates aspartate | Binds and positions the P1 aspartate for catalysis |
| Exosites | Secondary substrate binding sites outside active site | Enhance specificity toward natural protein substrates [75] |
The Schechter and Berger nomenclature designates substrate residues as P4-P3-P2-P1↓P1', where cleavage occurs after the P1 aspartate residue. The P4 position serves as the primary determinant of specificity, while the P1' position can influence cleavage efficiency and the functional consequences of proteolysis [73].
Caspases are categorized into three primary groups according to their tetrapeptide substrate preferences:
- Group I (Caspase-1, -4, -5, -14): Prefer (W/L/Y)EHD sequences
- Group II (Caspase-2, -3, -7): Prefer DEXD sequences (where X is any amino acid)
- Group III (Caspase-6, -8, -9, -10): Prefer (L/V/I)EXD sequences [2]
Executioner caspases-3 and -7 both belong to Group II and display nearly indistinguishable activity toward synthetic DEVD-based substrates, which initially led to the presumption of functional redundancy [74].
Figure 1: Caspase classification based on substrate sequence preferences
Functional Distinctions Between Caspase-3 and Caspase-7
Differential Substrate Cleavage Efficiency
Despite their similar tetrapeptide preferences, caspase-3 and caspase-7 exhibit marked differences in processing natural protein substrates. Table 2 compares their efficiency toward well-characterized substrates.
Table 2: Substrate Preference Profiles of Caspase-3 and Caspase-7
| Protein Substrate | Caspase-3 Efficiency | Caspase-7 Efficiency | Functional Consequence of Cleavage |
|---|---|---|---|
| PARP | High | High | Inactivation of DNA repair [74] |
| RhoGDI | High | High | Cytoskeletal reorganization [74] |
| Bid | High | Low/None | Mitochondrial amplification [74] |
| XIAP | High | Low | Relief of caspase inhibition [74] |
| Gelsolin | High | Low | Cytoskeletal dismantling [74] |
| Caspase-6 | High | Low | Effector caspase activation [74] |
| Caspase-9 | High | Low | Initiator caspase feedback [74] |
| Cochaperone p23 | Low | High | Disruption of chaperone function [74] |
Caspase-3 demonstrates broader substrate promiscuity and significantly greater efficiency toward most apoptotic substrates compared to caspase-7. This positions caspase-3 as the principal executioner caspase during the demolition phase of apoptosis [74]. The exceptional case of cochaperone p23, which shows preference for caspase-7, indicates specialized non-redundant functions [74].
Structural and Mechanistic Basis for Functional Differences
Although caspase-3 and caspase-7 share 56% sequence identity and 73% similarity, their sequence divergence results in distinct interactions with natural protein substrates [74]. Several factors contribute to their functional differentiation:
- Exosite Interactions: Secondary binding sites outside the catalytic pocket influence specificity toward natural protein substrates [75]
- Structural Variations: Differences in surface residues affect substrate binding and cleavage efficiency
- Cellular Localization: Distinct subcellular distributions may determine substrate accessibility
Global proteomic analyses reveal that while caspase-3 and caspase-7 share many common substrates, their rates of cleavage can vary by over 500-fold for specific targets, with caspase-3 generally processing a broader repertoire of substrates [75].
Experimental Approaches for Studying Executioner Caspases
Proteomic Methods for Substrate Identification
Advanced proteomic techniques enable comprehensive identification of caspase substrates and their cleavage sites:
- N-terminal Terminomics: Specific labeling of protein N-terminal to globally identify proteolytic cleavage sites during apoptosis [75]
- Multiplex Substrate Profiling (MSP): Uses synthetic peptide libraries to determine caspase specificity profiles [75]
- Comparative Analysis of Caspase-3/Caspase-7 Double Knockout Cells: Reveals caspase-dependent cleavage events in stressed and apoptotic conditions [65]
These approaches have identified hundreds of caspase substrates, with the number varying widely among different caspases - from few dozen targets for caspases-4, -5, -9, and -14 to hundreds for caspases-1, -2, -3, -6, -7, and -8 [75].
Real-Time Imaging and Reporter Systems
Novel fluorescent reporter systems enable dynamic visualization of executioner caspase activity in live cells:
- DEVD-Based Biosensors: Contain caspase-3/7 cleavage sequence (DEVD) linked to fluorescent protein reconstitution [38]
- ZipGFP Technology: Utilizes split-GFP fragments connected via DEVD linker; caspase cleavage enables GFP reassembly and fluorescence [38]
- mCasExpress Mouse Model: Lineage tracing system that permanently marks cells experiencing executioner caspase activation using FLP recombinase mediated by caspase cleavage [30]
These systems allow real-time tracking of caspase activation at single-cell resolution in both 2D cultures and 3D organoid models, providing unprecedented insight into the spatiotemporal dynamics of caspase activity [38].
Figure 2: Experimental approaches for studying executioner caspase function
Non-Apoptotic Functions and Therapeutic Implications
Sublethal Caspase Activation in Cellular Physiology
Beyond their established role in apoptosis, executioner caspases participate in diverse non-lethal cellular processes:
- Cellular Remodeling: Caspase activity regulates differentiation of stem cells, spermatogenesis, and erythroid differentiation [75]
- Liver Regeneration: Sublethal executioner caspase activation in hepatocytes promotes liver regeneration through JAK/STAT3 pathway stimulation [30]
- Stress Adaptation: In non-lethal stress conditions, caspase-3 and caspase-7 mediate protective responses and adaptive modifications [65]
- Immune Defense: Executioner caspases directly target bacterial virulence factors during infection, inhibiting intracellular pathogen growth [76]
In these contexts, caspase activity is precisely controlled at sublethal levels, allowing limited proteolysis without triggering cell death. The mCasExpress mouse model has demonstrated that hepatocytes with executioner caspase activation can survive, proliferate, and contribute to tissue regeneration [30].
Therapeutic Targeting and Research Applications
The distinct substrate preferences and functions of executioner caspases present opportunities for therapeutic intervention:
- Selective Caspase Inhibition: Developing caspase-specific inhibitors for pathological cell death conditions
- Cancer Therapy Sensitization: Modulating caspase activity to enhance chemotherapy efficacy
- Regenerative Medicine Applications: Harnessing sublethal caspase signaling for tissue repair
Understanding the molecular basis of caspase specificity is crucial for developing targeted therapies that can modulate specific caspase functions without globally disrupting caspase-dependent processes.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Executioner Caspase Studies
| Reagent / Tool | Type | Primary Research Application | Key Features |
|---|---|---|---|
| DEVD-AFC | Synthetic fluorogenic substrate | In vitro caspase activity assays | Releases AFC upon cleavage; used for enzyme kinetics [74] |
| zVAD-FMK | Pan-caspase inhibitor | Specificity controls; apoptosis inhibition | Irreversible binding to active site cysteine [38] |
| Caspase-3/7 Reporter (ZipGFP) | Live-cell fluorescent biosensor | Real-time apoptosis imaging in 2D/3D cultures | Low background; irreversible signal upon activation [38] |
| mCasExpress Mouse Model | Transgenic lineage tracing system | In vivo detection of cells with caspase activation | Permanent labeling of cells experiencing ECA [30] |
| Active-site Titrated Enzymes | Recombinant purified caspases | Biochemical characterization | Precisely quantified active enzyme concentrations [74] |
| Caspase-3/7 DKO Cells | Genetic knockout cell lines | Substrate identification; function studies | HCT116 cells lacking caspase-3 and caspase-7 [65] |
Executioner caspases-3 and -7, while sharing similar recognition motifs for synthetic peptides, exhibit significant functional specialization in biological contexts. Caspase-3 serves as the primary executioner caspase with broader substrate promiscuity, while caspase-7 processes a more limited repertoire with potential unique functions. Their differential regulation, cellular localization, and exosite interactions contribute to this functional divergence. Advanced proteomic and live-cell imaging technologies continue to reveal novel functions for these proteases beyond apoptosis, including roles in cellular remodeling, tissue regeneration, and host defense. Understanding the molecular logic of substrate cleavage by executioner caspases remains essential for deciphering their roles in both physiological and pathological processes, with significant implications for therapeutic development across a spectrum of human diseases.
Initiator caspases are fundamental components of the apoptotic machinery, serving as the pivotal triggers for programmed cell death (PCD) pathways. This technical review provides a comprehensive analysis of caspase-8, -9, and -10, examining their distinct and overlapping roles in caspase cascade activation and executioner functions. We synthesize current structural, mechanistic, and functional data to elucidate how these proteases integrate diverse death signals through specialized adaptor complexes and activation mechanisms. The analysis extends beyond traditional apoptotic roles to explore their functions in inflammatory cell death pathways and non-apoptotic signaling, with implications for therapeutic targeting in cancer, neurodegenerative disorders, and inflammatory diseases. Experimental methodologies and key research reagents are detailed to facilitate continued investigation into caspase biology and regulation.
Caspases are evolutionarily conserved cysteine proteases that cleave substrate proteins at specific aspartic acid residues, playing central roles in programmed cell death (PCD) and inflammation [1] [27]. Based on their position in apoptotic signaling cascades, caspases are categorized as either initiators (apical caspases) or executioners (effector caspases). Initiator caspases, including caspase-8, -9, and -10, function as the initial triggers of PCD pathways, proteolytically activating downstream executioner caspases (e.g., caspase-3, -6, -7) that dismantle cellular structures [1] [77]. These initiator caspases exhibit distinct structural features, activation mechanisms, and biological functions despite their shared role as apoptosis triggers.
The regulation of programmed cell death is crucial for development, immune function, and tissue homeostasis, with caspase dysregulation contributing to cancer, autoimmune disorders, and neurodegenerative diseases [1] [77]. Caspase-8 primarily initiates extrinsic apoptosis triggered by death receptors, while caspase-9 activates the intrinsic pathway mediated by mitochondrial stress [77] [27]. Caspase-10, a paralog of caspase-8, plays more complex and sometimes opposing roles in death receptor signaling [78] [79]. Understanding the comparative biology of these initiator caspases provides critical insights for therapeutic manipulation of cell death pathways.
This review examines the structural characteristics, activation mechanisms, and functional diversity of caspase-8, -9, and -10 within the broader context of caspase cascade research. We integrate recent advances in caspase biology to elucidate how these enzymes coordinate PCD and maintain cellular homeostasis.
Structural Characteristics and Domain Architecture
Initiator caspases share a conserved modular structure but possess distinct protein interaction domains that determine their specific activation contexts and functional roles. All caspases contain a catalytic domain comprising large (~p20) and small (~p10) subunits, but initiator caspases feature additional protein-protein interaction domains that facilitate their recruitment to specific activation platforms.
Table 1: Comparative Structural Features of Initiator Caspases
| Caspase | Protein Interaction Domain | Catalytic Domain Features | Unique Structural Characteristics |
|---|---|---|---|
| Caspase-8 | Two Death Effector Domains (DEDs) | Contains catalytic cysteine residue essential for protease activity | Forms filaments through DED interactions; heterodimerizes with cFLIP [80] [81] |
| Caspase-9 | Caspase Activation and Recruitment Domain (CARD) | Features a long linker loop between large and small subunits | Active site conformation regulated by dimerization rather than cleavage [77] |
| Caspase-10 | Two Death Effector Domains (DEDs) | High sequence homology to caspase-8 but different substrate specificity | Multiple isoforms (A, B, D, G) with distinct functions [82] [78] |
Caspase-8 and -10 both contain N-terminal death effector domains (DEDs) that facilitate their recruitment to death receptor signaling complexes [80] [82]. These domains mediate homotypic interactions with adapter proteins such as FADD (Fas-associated death domain protein). In contrast, caspase-9 possesses a CARD (caspase activation and recruitment domain) that enables its interaction with Apaf-1 (apoptotic protease-activating factor 1) within the apoptosome complex [77]. These specialized interaction domains ensure that each initiator caspase is activated in response to specific cell death stimuli.
The catalytic domains of initiator caspases are characterized by conserved structural features that regulate their protease activity. Caspase-8 activation requires dimerization within oligomeric platforms, which overcomes the unfavorable dissociation constant for monomer association [81]. Similarly, caspase-9 gains catalytic competence through dimerization rather than proteolytic cleavage, though cleavage stabilizes the active enzyme [77]. Recent evolutionary analyses reveal that caspase-8 has undergone specific adaptations that enable heterotypic interactions with the pyrin domain (PYD) of ASC (apoptosis-associated speck-like protein containing a CARD), facilitating its role in inflammatory cell death complexes called PANoptosomes [80].
Activation Mechanisms and Signaling Pathways
Initiator caspases are activated through distinct molecular mechanisms that coordinate specific programmed cell death pathways. The assembly of multi-protein activation platforms enables caspase dimerization and proteolytic activity initiation.
Caspase-8 Activation at the Death-Inducing Signaling Complex (DISC)
Caspase-8 activation occurs at the DISC, a multi-protein complex nucleated by ligated death receptors such as CD95/Fas or TRAIL receptors [81] [82]. Upon receptor activation, the adapter protein FADD recruits caspase-8 via DED-DED interactions, facilitating caspase-8 dimerization and activation through proximity-induced dimerization [81] [83]. The "induced proximity" model posits that DISC assembly overcomes the unfavorable dissociation constant for caspase-8 monomer association by increasing local concentration [81]. Activated caspase-8 then proteolytically processes downstream effector caspases, including caspase-3 and -7, initiating the apoptotic cascade.
A critical regulator of caspase-8 activation is cFLIP (cellular FLICE-inhibitory protein), which shares DED domains with caspase-8 but lacks full protease activity [81]. cFLIP can heterodimerize with caspase-8, altering its substrate specificity. The caspase-8/cFLIP heterodimer exhibits restricted activity toward pro-apoptotic targets like caspase-3 and Bid but effectively cleaves components of the necroptosis pathway, thereby inhibiting RIPK1/RIPK3-mediated necroptotic cell death [81]. This mechanism enables caspase-8 to function as a molecular switch between apoptosis and necroptosis.
Figure 1: Caspase-8 Activation at the DISC and Regulation by cFLIP
Caspase-9 Activation at the Apoptosome
Caspase-9 activation occurs within the apoptosome, a wheel-like complex composed of seven Apaf-1 molecules [77]. Cytochrome c released from mitochondria during intrinsic apoptosis binds to Apaf-1, promoting ATP/dATP-dependent apoptosome assembly. The apoptosome then recruits caspase-9 via CARD-CARD interactions between Apaf-1 and caspase-9 [77]. Two models explain caspase-9 activation: the "induced conformation" model proposes that apoptosome binding alters caspase-9 conformation to enhance catalytic activity, while the "proximity-induced dimerization" model suggests the apoptosome serves primarily as a platform to concentrate caspase-9 monomers, facilitating dimer-driven activation [77].
Unlike caspase-8, caspase-9 dimerization alone is insufficient for full activation; the apoptosome functions as an allosteric regulator that enhances caspase-9 protease activity. Recent structural studies reveal that caspase-9 activation requires multiple interfaces between Apaf-1 and caspase-9 CARD domains, not merely the 1:1 interaction previously proposed [77]. Procaspase-9 exhibits higher affinity for the apoptosome than its cleaved form, and autoprocessing serves as a molecular timer that regulates apoptosome activity duration [77].
Caspase-10 Activation and Regulatory Roles
Caspase-10 activation occurs at the DISC through mechanisms similar to caspase-8, but with important functional distinctions [82] [78]. Caspase-10 is recruited to both CD95 and TRAIL DISCs in a FADD-dependent manner and undergoes proteolytic activation. However, unlike caspase-8, caspase-10 cannot compensate for caspase-8 deficiency in apoptosis initiation [82]. Caspase-10 exists as multiple isoforms (A, B, D, and G) with distinct and sometimes opposing functions [78]. Caspase-10A and -10D isoforms promote apoptosis, while caspase-10B lacks pro-apoptotic activity due to degradation via the ubiquitin-proteasome pathway [78].
Recent studies indicate that caspase-10 negatively regulates caspase-8-mediated cell death, switching the cellular response to CD95L in favor of NF-κB activation and cell survival [79]. This regulatory function highlights the complex relationship between these caspase-8 paralogs, where caspase-10 can modulate rather than mimic caspase-8 activity in specific contexts.
Functional Diversity in Cell Death Pathways
Initiator caspases coordinate multiple forms of programmed cell death, functioning as critical decision points in cellular fate determination. Beyond their traditional roles in apoptosis, these caspases participate in inflammatory cell death pathways and exhibit non-apoptotic functions.
Table 2: Functional Roles of Initiator Caspases in Cell Death Pathways
| Caspase | Primary Death Pathway | Key Functions | Regulatory Roles |
|---|---|---|---|
| Caspase-8 | Extrinsic Apoptosis | Initiator of extrinsic apoptosis; activates executioner caspases | Inhibits necroptosis; promotes NF-κB activation; component of PANoptosomes [80] [1] [81] |
| Caspase-9 | Intrinsic Apoptosis | Initiator of mitochondrial apoptosis; activates caspase-3/7 | Cleaves RIPK1 to inhibit necroptosis; regulates developmental apoptosis [77] [27] |
| Caspase-10 | Extrinsic Apoptosis | Modulates death receptor signaling | Negatively regulates caspase-8-mediated apoptosis; promotes NF-κB activation [78] [79] |
Apoptosis Regulation
Caspase-8 serves as the primary initiator of extrinsic apoptosis, directly activating executioner caspases and cleaving the BID protein to amplify death signaling through the mitochondrial pathway [1] [27]. Mice lacking caspase-8 exhibit embryonic lethality due to defects in endothelial development and blood vessel stabilization, highlighting its essential developmental role [81].
Caspase-9 is the key initiator of intrinsic apoptosis triggered by cellular stress, DNA damage, or developmental cues [77]. Caspase-9 deficiency in mice causes perinatal lethality with severe brain malformations due to suppressed apoptosis during brain development [77]. Caspase-9 null cells are resistant to diverse apoptotic stimuli, including UV irradiation and chemotherapeutic agents [77].
Caspase-10 modulates death receptor-mediated apoptosis but cannot substitute for caspase-8 in apoptosis initiation [82] [78]. The specific functions of caspase-10 vary by isoform, with caspase-10A and -10D promoting apoptosis while caspase-10B and the truncated caspase-10G isoform lack pro-apoptotic activity [78].
Cross-Pathway Regulation and PANoptosis
Recent research has revealed extensive crosstalk between cell death pathways, with initiator caspases functioning as key integration points. Caspase-8 regulates the switch between apoptosis and necroptosis by cleaving and inactivating RIPK1 and RIPK3, critical necroptosis mediators [1] [27]. When caspase-8 is inhibited, cells default to RIPK3/MLKL-dependent necroptosis [81].
Caspase-8 also participates in PANoptosis, an inflammatory cell death pathway integrating components from pyroptosis, apoptosis, and necroptosis [80]. Caspase-8 forms complexes with ASC (apoptosis-associated speck-like protein containing a CARD) in PANoptosomes, multiprotein complexes that drive inflammatory lytic cell death in response to innate immune activation [80]. Evolutionary analyses indicate that caspase-8 acquired the ability to interact with ASC's pyrin domain through specific adaptations, enabling its role in this composite cell death pathway [80].
Figure 2: Initiator Caspases in Cell Death Pathway Regulation
Non-Apoptotic Functions
Emerging evidence indicates that initiator caspases participate in processes beyond cell death. Executioner caspase activation (ECA) at sublethal levels promotes liver regeneration through JAK/STAT3 signaling rather than inducing apoptosis [30]. Similarly, caspase-8 regulates immune cell activation and differentiation independent of its cell death functions [81]. These non-apoptotic roles expand the functional repertoire of initiator caspases in physiological and pathological processes.
Experimental Methodologies and Research Reagents
Studying initiator caspases requires specialized methodologies and reagents that enable precise detection, activation, and functional characterization. This section outlines key experimental approaches and their applications in caspase research.
Complex Isolation and Analysis
Death-Inducing Signaling Complex (DISC) Immunoprecipitation: The DISC forms upon death receptor activation and serves as the platform for caspase-8 and -10 activation [82]. Standard protocol involves stimulating cells with death receptor ligands (e.g., CD95L, TRAIL) followed by cell lysis and immunoprecipitation using receptor-specific antibodies. Co-precipitated proteins including FADD, caspase-8, and caspase-10 are detected by immunoblotting [82]. This method enables analysis of caspase recruitment and activation kinetics at native DISCs.
Apoptosome Assembly Assays: Caspase-9 activation can be studied using in vitro apoptosome reconstitution systems [77]. Cytochrome c, dATP/ATP, and Apaf-1 are incubated with caspase-9 to form the functional apoptosome complex. Activity measurements using fluorogenic caspase-9 substrates (e.g., LEHD-AFC) quantify activation efficiency. This approach facilitates analysis of caspase-9 regulation by post-translational modifications and small molecule inhibitors.
Activity Monitoring and Detection
FRET-Based Caspase Biosensors: Fluorescence resonance energy transfer (FRET) biosensors enable real-time monitoring of caspase activation in single living cells [83]. These biosensors consist of fluorescent proteins linked by caspase-cleavable sequences (DEVD for executioner caspases, IETD for caspase-8). Caspase-mediated cleavage disrupts FRET, providing a sensitive readout of spatiotemporal activation dynamics [83].
Lineage Tracing of Caspase Activation: The mCasExpress system genetically labels cells that have experienced executioner caspase activation (ECA) [30]. This transgenic mouse model expresses a membrane-tethered FLP recombinase connected to a caspase-cleavable linker (DEVD). Caspase activation releases FLP, which induces permanent expression of a reporter gene (ZsGreen). This system identifies cells that survive transient caspase activation, enabling study of non-lethal caspase functions [30].
Functional Manipulation Approaches
Genetic Knockout and Knockdown Models: Caspase-8 and -9 deficient mice reveal essential developmental roles and embryonic lethality phenotypes [81] [77]. Cell lines derived from these models, or cells with siRNA/shRNA-mediated caspase knockdown, enable functional studies of specific caspases in death receptor and stress-induced apoptosis [78].
Caspase Inhibition Studies: Pharmacological inhibitors (e.g., z-VAD-FMK for pan-caspase inhibition, z-IETD-FMK for caspase-8) and endogenous inhibitors (e.g., XIAP, cFLIP) help delineate caspase-specific functions [81] [30]. These tools are particularly valuable for distinguishing between apoptosis and alternative cell death pathways.
Table 3: Essential Research Reagents for Initiator Caspase Studies
| Reagent/Category | Specific Examples | Research Applications | Key References |
|---|---|---|---|
| Pharmacological Inhibitors | z-VAD-FMK (pan-caspase), z-IETD-FMK (caspase-8), z-LEHD-FMK (caspase-9) | Distinguishing caspase-dependent and independent death pathways; studying specific caspase functions | [81] [30] |
| Genetic Models | Caspase-8 and caspase-9 knockout mice; Caspase-3/7 double knockout mice; siRNA/shRNA for caspase knockdown | Establishing essential caspase functions; creating caspase-deficient cellular models | [81] [77] [30] |
| Activity Assays | Fluorogenic substrates (IETD-AFC for caspase-8, LEHD-AFC for caspase-9); FRET-based biosensors; mCasExpress lineage tracing system | Quantifying caspase activation; monitoring spatiotemporal dynamics; tracking cells with caspase activity | [77] [30] [83] |
| Complex Isolation | DISC immunoprecipitation; apoptosome reconstitution; size exclusion chromatography | Studying caspase activation mechanisms and protein interactions | [80] [82] |
| Antibodies | Caspase-8 (recognizing p55/p59 isoforms); caspase-9; caspase-10 (specific for prodomain) | Detecting caspase expression, processing, and complex recruitment by immunoblotting | [82] [78] |
Therapeutic Implications and Future Perspectives
The central role of initiator caspases in cell death regulation makes them attractive therapeutic targets for cancer, neurodegenerative disorders, and inflammatory diseases. Understanding caspase-specific functions enables development of targeted interventions that modulate specific cell death pathways.
In cancer therapy, caspase-8 expression is frequently silenced in tumors, contributing to resistance to death receptor-mediated apoptosis [78]. Restoring caspase-8 expression or activity represents a potential strategy to sensitize tumors to chemotherapy. Conversely, caspase-9 inhibition may protect against degenerative conditions; caspase-9 polymorphisms are associated with increased cancer risk, while its overexpression correlates with degenerative disorders including discogenic low back pain and Huntington's disease [77].
The regulatory functions of caspase-8 in necroptosis inhibition have implications for inflammatory disease treatment. Enhanced necroptosis due to reduced caspase-8 activity contributes to pathogenesis in mouse models of inflammatory conditions [81]. Small molecules that selectively enhance caspase-8's anti-necroptotic activity without triggering apoptosis could provide novel anti-inflammatory therapeutics.
Future research directions include elucidating the structural basis for caspase-8's interaction with ASC in PANoptosomes [80], defining context-specific caspase-10 functions across different isoforms [78] [79], and developing isoform-specific caspase modulators for therapeutic applications. The emerging roles of sublethal caspase activation in processes like liver regeneration [30] also warrant further investigation for regenerative medicine applications.
This comparative analysis highlights the specialized functions of initiator caspases in programmed cell death pathways. While caspase-8, -9, and -10 share common features as apical proteases in apoptotic cascades, each possesses unique characteristics that determine their specific activation contexts, substrate preferences, and biological functions. Caspase-8 serves as the primary initiator of extrinsic apoptosis and a key regulator of cell fate decisions between apoptosis and necroptosis. Caspase-9 triggers mitochondrial apoptosis and is essential for developmental cell death. Caspase-10 modulates death receptor signaling with isoform-specific effects that can either promote or inhibit apoptosis.
Recent advances have expanded our understanding of initiator caspases beyond traditional apoptosis roles to include regulation of inflammatory cell death pathways and non-lethal signaling functions. The experimental methodologies and reagents detailed herein provide essential tools for continued investigation of caspase biology. Therapeutic targeting of initiator caspases holds promise for treating diverse diseases, though successful translation will require careful consideration of caspase-specific functions and pathway interactions. As research continues to unravel the complexities of caspase regulation and function, new opportunities will emerge for precisely modulating cell death pathways in human health and disease.
The study of caspases, cysteine-aspartic proteases central to programmed cell death and inflammation, has been profoundly advanced through deficiency models. Both natural human immune disorders and engineered mouse models have served as indispensable tools for unraveling the complex, non-redundant functions of these enzymes beyond their traditional roles in apoptosis. This whitepaper synthesizes current knowledge from these deficiency models, highlighting how the absence or mutation of specific caspases and their adaptor proteins disrupts immune homeostasis and provides critical insights into caspase cascade regulation. The findings underscore the therapeutic potential of targeting caspase pathways in inflammatory, infectious, and neoplastic diseases while outlining essential methodological frameworks for continued investigation.
Caspases are evolutionarily conserved cysteine-dependent aspartate-specific proteases that serve as critical mediators of programmed cell death (PCD), inflammation, and cellular homeostasis [1] [84]. These enzymes are synthesized as inactive zymogens and undergo proteolytic activation in response to specific stimuli, initiating cascades that ultimately lead to controlled cellular dismantling or inflammatory signaling [61]. The caspase family is historically categorized based on structural features and primary functions: initiator caspases (caspase-2, -8, -9, -10) containing long prodomains that facilitate activation through multiprotein complexes; executioner caspases (caspase-3, -6, -7) with shorter prodomains that are cleaved and activated by initiator caspases; and inflammatory caspases (caspase-1, -4, -5, -11, -12) primarily involved in cytokine maturation and inflammatory responses [85] [84].
Table 1: Major Caspase Classification and Primary Functions
| Category | Members | Activation Mechanism | Primary Functions |
|---|---|---|---|
| Initiator | Caspase-2, -8, -9, -10 | Induced proximity dimerization in multiprotein complexes (DISC, apoptosome) | Initiate apoptotic signaling; non-apoptotic roles in differentiation, proliferation |
| Executioner | Caspase-3, -6, -7 | Cleavage by initiator caspases | Proteolytic cleavage of cellular substrates; demolition phase of apoptosis |
| Inflammatory | Caspase-1, -4, -5, -11 | Inflammasome assembly; autocatalytic activation | Cytokine maturation (IL-1β, IL-18); pyroptosis execution |
Deficiency models—whether naturally occurring in humans or experimentally engineered in mice—have provided unparalleled insights into the non-redundant, specific functions of individual caspases within biological systems. These models have revealed that despite structural similarities and overlapping substrate preferences, caspases exhibit remarkable functional specificity in physiological and pathological contexts [84] [86]. The phenotypic consequences of caspase deficiency range from embryonic lethality and immune dysregulation to specific defects in cellular differentiation and tissue homeostasis, reflecting the diverse roles these proteases play beyond their traditional association with cell death [84] [87].
Human Caspase Deficiencies and Immune Disorders
Natural human deficiencies in caspase signaling pathways have illuminated the critical functions of these molecules in host defense and immune regulation. These disorders often present with specific infectious susceptibilities, highlighting the non-redundant roles of particular caspases in immune responses.
CARD9 Deficiency and CNS Candidiasis
Caspase Recruitment Domain-containing protein 9 (CARD9) deficiency represents a paradigm for understanding how defects in caspase-associated signaling pathways predispose to specific infectious diseases. CARD9 functions as a critical adaptor protein downstream of C-type lectin receptors that sense fungal pathogens, facilitating caspase activation and inflammatory responses [88].
Human patients with homozygous mutations in the CARD9 gene, such as the recurring p.Y91H mutation, develop chronic central nervous system (CNS) candidiasis without systemic sepsis, indicating a specific defect in localized antifungal immunity within the CNS [88]. The clinical presentation includes neurological symptoms manifesting late during infection with progressive brain fungal burden, suggesting a failure to contain fungal pathogens within neural tissue rather than a systemic immune defect.
Table 2: Human Caspase-Related Deficiency Disorders
| Deficiency | Genetic Basis | Clinical Manifestations | Immune Defect |
|---|---|---|---|
| CARD9 Deficiency | Mutations in CARD9 gene (e.g., p.Y91H) | Chronic CNS candidiasis; late-onset neurological symptoms | Defective antifungal immunity; impaired monocyte recruitment to CNS |
| Caspase-8 Deficiency | Rare mutations in CASP8 gene | Autoimmunity; immunodeficiency; lymphoproliferation | Impaired extrinsic apoptosis; defective lymphocyte homeostasis |
The immunopathogenesis of CARD9 deficiency involves defective mononuclear cell aggregation at fungal lesions in the brain, with impaired recruitment of MHCII+Ly6C+ monocytes during early infection [88]. Histopathological examination reveals cerebral multinucleated giant cells and granulomata formation, indicating attempted but ultimately ineffective containment of fungal pathogens. This human deficiency model underscores the essential role of CARD9-mediated caspase activation in orchestrating effective antifungal immunity within the central nervous system.
Mouse Models of Caspase Deficiency
Engineered mouse models with targeted caspase deletions have been instrumental in delineating the specific functions of individual caspases in development, immune function, and tissue homeostasis. These models recapitulate aspects of human disease while enabling detailed mechanistic investigation of caspase functions in a controlled genetic background.
Phenotypic Spectrum of Caspase-Deficient Mice
Mouse models with genetic ablation of specific caspases have revealed a remarkable diversity of phenotypes, from embryonic lethality to surprisingly subtle defects, highlighting both essential and context-dependent functions.
Table 3: Mouse Models of Caspase Deficiency
| Caspase | Mouse Phenotype | Primary Defects | Human Correlations |
|---|---|---|---|
| Caspase-8 | Embryonic lethality (E10.5-12.5); heart defects; impaired hematopoietic development | Defective extrinsic apoptosis; hyperactive necroptosis; impaired endothelial cell function | Rare caspase-8 deficiency with autoimmunity and lymphoproliferation |
| Caspase-9 | Embryonic/perinatal lethality; brain malformations with ectopic neuronal clusters | Defective intrinsic apoptosis; resistance to developmental neuronal death | - |
| Caspase-3 | Perinatal lethality; neurological hyperplasias; cardiac defects | Reduced apoptotic DNA fragmentation; impaired demolition phase of apoptosis | - |
| Caspase-2 | Viable with subtle defects; accelerated tumorigenesis; metabolic syndrome | Genomic instability; defective cell cycle checkpoint; oxidative stress sensitivity | Potential tumor suppressor role |
| Caspase-1 | Viable; impaired IL-1β/IL-18 processing; reduced inflammatory responses | Defective inflammasome signaling; resistance to inflammatory stimuli | - |
| Caspase-11 | Viable; impaired non-canonical pyroptosis; reduced septic shock | Defective cytosolic LPS sensing; reduced GSDMD cleavage | Orthologue of human caspase-4/5 |
The phenotypic analysis of caspase-deficient mice reveals several important patterns. First, deficiency of initiator caspases central to core apoptotic pathways (caspase-8, -9) typically results in embryonic lethality, underscoring their non-redundant roles in development [84] [86]. Second, executioner caspase deficiency (caspase-3, -7) often permits development but causes perinatal lethality with tissue-specific abnormalities, suggesting partial functional redundancy among executioners [87]. Third, inflammatory caspase deficiencies generally yield viable mice with specific immune defects rather than developmental abnormalities, reflecting their specialized roles in host defense [84].
Caspase-8: A Master Regulator of Cell Death and Immunity
Caspase-8 deficiency in mice results in embryonic lethality between E10.5 and E12.5, with characterized defects in heart development and impaired hematopoietic progenitor cell production [87] [86]. This lethal phenotype stems from caspase-8's dual role as both an initiator of extrinsic apoptosis and a critical suppressor of necroptosis. In the absence of caspase-8, death receptor signaling defaults to RIPK1/RIPK3/MLKL-dependent necroptosis, resulting in uncontrolled inflammatory cell death [1] [2].
Tissue-specific caspase-8 deletion models have revealed additional functions in immune homeostasis. Macrophage-specific caspase-8 deficiency compromises differentiation of monocytes into macrophages, highlighting a non-apoptotic role in cellular differentiation [87]. This defect involves impaired caspase-8-mediated proteolysis of RIP1, which normally downregulates NF-κB activity to favor macrophage differentiation [87]. These findings illustrate how caspase-8 functions as a molecular switch between different cell death modalities and cellular differentiation pathways.
Caspase-2: The Orphan Caspase with Tumor Suppressor Functions
Unlike other initiator caspases, caspase-2 deficiency does not cause embryonic lethality or major developmental defects in mice [86]. However, detailed analysis reveals important roles in tumor suppression, metabolism, and genomic stability. Caspase-2-deficient mice exhibit accelerated tumorigenesis in Myc-driven cancer models and are more readily transformed by Ras/E1A oncogenes, supporting a tumor suppressor function [87] [86].
Mechanistically, caspase-2 contributes to maintenance of genomic integrity through regulation of the cell cycle. Caspase-2-deficient cells show defective G2/M arrest in response to DNA damage, allowing progression through the cell cycle despite genomic lesions [87]. This function involves caspase-2 phosphorylation by DNA-PKcs in response to DNA damage, though the relevant substrates mediating this cell cycle regulation remain incompletely characterized [87].
Experimental Methodologies for Caspase Research
The study of caspase functions and deficiency models relies on sophisticated experimental approaches that enable precise manipulation and detection of caspase activity in physiological contexts.
Generation of Caspase-Deficient Mouse Models
Standardized protocols for creating and analyzing caspase-deficient mice have been essential for advancing the field.
Gene Targeting Strategies:
- Conventional knockout approaches: Homologous recombination in embryonic stem cells to replace critical exons with selection cassettes
- Conditional knockout systems: LoxP sites flanking essential exons for tissue-specific deletion using Cre recombinase
- Knock-in models: Introduction of specific point mutations (e.g., catalytic cysteine mutants) to eliminate protease activity while preserving protein expression
Phenotypic Analysis Workflow:
- Embryonic Lethality Assessment: Detailed morphological and histological examination of embryos at developmental timepoints
- Immune System Profiling: Flow cytometric analysis of hematopoietic cell populations in bone marrow, spleen, thymus, and peripheral blood
- Cell Death Assays: Exposure to apoptotic stimuli (death receptor ligands, DNA damaging agents) and measurement of viability and caspase activation
- Infection Models: Challenge with pathogens (bacterial, viral, fungal) to evaluate immune competence
- Cancer Models: Crossing with tumor-prone backgrounds (e.g., Myc transgenic, ApcMin/+) to assess tumor suppressor functions
Advanced Caspase Activity Monitoring
Traditional methods for detecting caspase activity (Western blotting, fluorogenic substrate assays) have been supplemented with sophisticated tools that enable spatial and temporal monitoring of caspase activation in live cells and animals.
Live Imaging Approaches:
- Fluorescent-Labeled Inhibitors (FLIs): Cell-permeable fluorescent molecules that covalently bind active caspases for real-time tracking
- FRET Sensors: Caspase-specific cleavage sequences between FRET pairs that report activation through changes in fluorescence resonance energy transfer
- mCasExpress System: Transgenic mouse lineage tracing system that permanently marks cells that have experienced executioner caspase activation
The mCasExpress system employs a clever genetic strategy wherein a membrane-tethered FLP recombinase is liberated by caspase-3/7-mediated cleavage at a DEVD recognition sequence, allowing translocation to the nucleus and permanent activation of a reporter gene [30]. This system enables retrospective identification of cells that have experienced caspase activation, even if they subsequently survive, making it particularly valuable for studying non-lethal caspase functions.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Caspase Studies
| Reagent Category | Specific Examples | Applications | Key Features |
|---|---|---|---|
| Caspase-Deficient Mice | Caspase-8 KO, Caspase-9 KO, Caspase-3 KO | In vivo functional studies; developmental analysis; disease modeling | Tissue-specific conditional alleles available for lethal mutations |
| Activity Probes | FLICA (Fluorochrome-Labeled Inhibitors of Caspases); ABPs (Activity-Based Probes) | Ex vivo and in vivo caspase activity detection; cell sorting based on activation status | Covalent binding to active site; compatible with flow cytometry and microscopy |
| Reporter Systems | mCasExpress; FRET-based biosensors | Lineage tracing of caspase-activated cells; real-time activity monitoring in live cells | Permanent labeling of previously active cells; non-destructive temporal tracking |
| Antibodies | Cleavage-specific antibodies (anti-cleaved caspase-3, -8, -9); PARP cleavage antibodies | Immunohistochemistry; Western blotting; assessment of apoptosis in fixed tissues | Detect active caspase fragments; well-validated for specific caspases |
| Chemical Inhibitors | zVAD-fmk (pan-caspase); DEVD-CHO (caspase-3/7); Q-VD-OPh (broad spectrum) | Functional validation; therapeutic potential assessment | Cell-permeable; reversible or irreversible inhibition |
| Mass Spectrometry | Multiplexed substrate quantification; TAILS (Terminal Amine Isotopic Labeling of Substrates) | Proteome-wide identification of caspase substrates; cleavage site mapping | Unbiased discovery of novel caspase targets and pathways |
Signaling Pathways in Caspase Deficiency
The following diagrams illustrate key signaling pathways disrupted in caspase deficiency models, generated using Graphviz DOT language with high color contrast for clarity.
CARD9 Deficiency Pathway: This diagram illustrates how mutations in CARD9 disrupt caspase activation downstream of fungal pattern recognition, leading to defective monocyte recruitment and chronic CNS candidiasis.
Caspase-8 Deficiency Consequences: This diagram shows how caspase-8 deficiency prevents extrinsic apoptosis while allowing unchecked necroptosis, resulting in embryonic lethality.
Discussion and Therapeutic Implications
The study of caspase deficiencies in both human disorders and mouse models has revealed the exquisite specificity of these proteases in physiological processes and disease pathogenesis. Several key principles have emerged from these deficiency studies.
First, caspases exhibit non-redundant functions despite overlapping substrate specificities in vitro. The distinct phenotypes of different caspase-deficient mice highlight that in vivo context, including cellular localization, expression patterns, and interacting partners, dictates functional specificity [84] [86]. Second, caspases function as critical molecular switches between different cell death modalities. Caspase-8 deficiency illustrates this principle perfectly, with loss of this protease resulting in a default to necroptotic cell death rather than simple ablation of cell death [1] [2]. Third, non-apoptotic functions of caspases play essential roles in development, immunity, and tissue homeostasis. The defects in macrophage differentiation observed with caspase-8 deficiency and the metabolic abnormalities in caspase-2 deficient mice exemplify these non-lethal functions [87] [86].
Therapeutic targeting of caspase pathways represents a promising approach for diverse diseases. In inflammatory conditions, inhibition of inflammatory caspases may mitigate excessive cytokine production and tissue damage [2]. In neurodegenerative diseases, caspase inhibitors may protect against neuronal loss, though the complex interplay between different cell death modalities requires careful modulation rather than broad suppression [1]. In cancer, strategies to reactivate apoptotic caspases or inhibit non-lethal pro-survival caspase functions could overcome therapeutic resistance [85] [87].
Future research directions should focus on understanding context-specific caspase regulation, developing more precise tools for modulating specific caspase functions in particular tissues, and elucidating the full spectrum of non-apoptotic caspase substrates. The continued refinement of deficiency models, including human organoid systems and conditional genetic approaches, will further advance our understanding of these critical proteases in health and disease.
Deficiency models have proven indispensable for unraveling the complex, multifaceted functions of caspases beyond their traditional roles in cell death. Human immune disorders such as CARD9 deficiency provide clinical relevance and identify essential non-redundant functions, while engineered mouse models enable systematic dissection of molecular mechanisms and physiological consequences. Together, these approaches have revealed caspases as critical regulators of development, immunity, and tissue homeostasis whose functions are highly context-dependent and specific. The continuing refinement of experimental approaches for monitoring and manipulating caspase activity promises to yield new insights into these essential proteases and their potential as therapeutic targets across a spectrum of human diseases.
The regulation of programmed cell death is a cornerstone of cellular homeostasis, with the caspase cascade serving as its central executioner. The efficacy and ultimate outcome of caspase activation are not determined in isolation but are profoundly influenced by a complex network of interlinked signaling pathways. Among the most critical modulators are the c-Jun N-terminal kinase (JNK), p53, and Nuclear Factor-kappa B (NF-κB) pathways. These pathways engage in extensive bidirectional crosstalk, integrating diverse cellular stress signals—including DNA damage, oxidative stress, and cytokine signaling—to collectively determine whether a cell survives, undergoes apoptosis, or triggers inflammatory cell death. This intricate communication network ensures that cell fate decisions are precisely calibrated to the specific type and intensity of stress encountered. Understanding the molecular architecture of this crosstalk is paramount for developing targeted therapeutic interventions in cancer, neurodegenerative disorders, and inflammatory diseases where these pathways are frequently dysregulated.
Pathway-Specific Molecular Mechanisms
JNK Signaling Dynamics and Substrate Regulation
The JNK pathway functions as a critical sensor of cellular stress, with the duration and oscillation of its activity encoding specific instructions for cell fate. JNK activation occurs through a three-tiered kinase module: MAP kinase kinase kinases (MAP3Ks) activate MAP kinase kinases (MKK4 and MKK7), which in turn phosphorylate and activate JNK [89]. The temporal dynamics of JNK activation—transient, sustained, or pulsed—are not arbitrary but are precisely calibrated to the nature of the stress stimulus and ultimately dictate specific transcriptional outputs [90]. Sustained JNK activation is frequently associated with pro-apoptotic outcomes, particularly in scenarios involving UV radiation or cytokine-induced stress.
JNK exerts its effects through both transcriptional and non-transcriptional mechanisms. A primary nuclear function involves the phosphorylation of the transcription factor c-Jun at serines 63 and 73, potentiating its ability to activate a repertoire of pro-apoptotic genes [89]. Beyond transcription factors, JNK directly phosphorylates cytoplasmic substrates, including members of the Bcl-2 family. It can phosphorylate and inactivate the anti-apoptotic proteins Bcl-2 and Bcl-xL, while simultaneously activating the pro-apoptotic proteins Bim and BAD, thereby shifting the balance toward mitochondrial outer membrane permeabilization (MOMP) and apoptosis initiation [89] [91]. The discovery that mRNA stability mediates distinct gene expression patterns in response to different JNK activation dynamics adds another layer of complexity to its regulatory potential [90].
p53 as the Integrative Stress Sensor
The p53 tumor suppressor protein serves as a nodal point for the integration of diverse stress signals, including DNA damage, oncogene activation, and ribosomal stress. Its function is tightly regulated by a multitude of post-translational modifications that determine its stability, DNA-binding affinity, and transcriptional specificity [92]. As a sequence-specific transcription factor, p53 binds to defined responsive elements in target genes, orchestrating a spectrum of cellular responses ranging from transient cell cycle arrest and DNA repair to senescence and apoptosis.
The pro-apoptotic function of p53 is executed through the transcriptional transactivation of genes encoding proteins involved in both the extrinsic and intrinsic apoptotic pathways. Key transcriptional targets include the death receptor FAS, the pro-apoptotic Bcl-2 family proteins Puma and Noxa, and the Apaf-1 component of the apoptosome [92]. Furthermore, p53 can directly promote MOMP through transcription-independent mechanisms by translocating to the mitochondria and engaging with anti-apoptotic Bcl-2 family members, thereby facilitating Bax/Bak activation [92]. The specific cellular response elicited by p53 is influenced by the stress context, cell type, and interactions with other signaling pathways, ensuring a response appropriately tailored to the level of damage.
The Dual Nature of NF-κB in Survival and Death
The NF-κB pathway is a quintessential mediator of inflammatory and survival signals, frequently functioning as a critical counterbalance to pro-apoptotic pathways. The canonical NF-κB pathway is typically activated by cytokines such as TNF-α and leads to the translocation of p50-RelA heterodimers into the nucleus. In contrast, the non-canonical pathway, activated by specific TNF family members, results in the processing of p100 to p52 and the nuclear translocation of p52-RelB complexes [93].
NF-κB promotes cell survival through the transcriptional induction of a formidable arsenal of anti-apoptotic proteins. These include:
- Bcl-2 homologs: Bcl-xL and A1/Bfl-1, which prevent MOMP.
- Inhibitor of Apoptosis (IAP) family members: cIAP1, cIAP2, and XIAP, which directly inhibit caspase activity.
- Caspase-8 regulator: Cellular FLIP (c-FLIP), which inhibits death receptor-mediated apoptosis [93].
The constitutive activation of NF-κB is a hallmark of numerous lymphoid malignancies, where it confers resistance to both intrinsic and extrinsic apoptosis inducers, underscoring its pivotal role in tumor cell survival [93].
Table 1: Key Anti-apoptotic Target Genes of NF-κB
| Gene Target | Protein Function | Impact on Apoptosis |
|---|---|---|
| Bcl-xL | Inhibits MOMP | Blocks intrinsic pathway |
| XIAP, cIAP1/2 | Direct caspase inhibition | Blocks executioner caspases |
| c-FLIP | Inhibits caspase-8 activation | Blocks extrinsic pathway |
Experimental Analysis of Signaling Pathways
Methodologies for JNK Dynamics and Gene Expression
The analysis of JNK signaling requires techniques capable of capturing its dynamic nature. A comprehensive experimental workflow to investigate how JNK dynamics influence gene expression involves the following key methodologies [90]:
Induction of Specific JNK Dynamics: Utilize precise dosing regimens of a JNK agonist (e.g., anisomycin at a subinhibitory concentration of 50 ng/ml to minimize translational shutoff) to generate distinct temporal profiles:
- Sustained Activation: Continuous exposure to the agonist.
- Transient Activation: Short-term exposure followed by rapid washout.
- Pulsed Activation: Multiple cycles of addition and washout.
Live-Cell Imaging of Kinase Activity: Employ fluorescent biosensors, such as the JNKKTR, to track JNK activation dynamics in real-time within single cells. This biosensor exhibits a nucleocytoplasmic shift upon JNK-mediated phosphorylation, allowing quantification of kinase activity.
Validation of Endogenous Effectors: Perform western blot analysis to confirm that the observed biosensor dynamics reflect endogenous pathway activity. Key targets include phosphorylation of the transcription factor c-Jun at Serine 73.
Transcriptomic Output Analysis: Conduct RNA-seq on samples collected at multiple time points post-stimulation to capture the global gene expression patterns resulting from different JNK dynamics.
Computational Modeling: Utilize Ordinary Differential Equation (ODE) models to explore the relationship between JNK dynamics, mRNA stability, and the resulting gene expression clusters.
Assessing NF-κB-Mediated Apoptosis Resistance
To experimentally determine the role of NF-κB in conferring resistance to apoptosis, the following protocol can be used, as derived from studies on lymphoma cell lines [93]:
Cell Model Selection: Utilize cell lines with constitutively active NF-κB (e.g., Tax-expressing or EBV-positive lymphomas) alongside control cells without constitutive activation.
Pathway Inhibition:
- Genetic Knockdown: Employ lentiviral vectors encoding shRNAs to specifically target components of the canonical (p105/NF-κB1) or non-canonical (p100/NF-κB2) pathways.
- Pharmacological Inhibition: Use inhibitors targeting IκB kinase (IKK) or proteasome function to block NF-κB activation.
Apoptosis Induction and Assessment:
- Intrinsic Pathway Inducers: Treat cells with etoposide or subject them to γ-irradiation.
- Extrinsic Pathway Inducers: Treat cells with TNF-α or TRAIL.
- Quantification of Apoptosis: Use flow cytometry with Annexin V and Propidium Iodide (PI) staining to quantify the percentage of apoptotic cells.
Downstream Analysis:
- Western Blotting: Analyze cleaved fragments of key caspases (e.g., caspase-3, -8, -9) to identify the stage of apoptotic blockade.
- Gene Expression Profiling: Evaluate changes in the expression levels of NF-κB-dependent anti-apoptotic genes (Bcl-xL, FLIP, XIAP, cIAP1/2) following pathway inhibition.
System Integration: Inter-Pathway Crosstalk
The JNK, p53, and NF-κB pathways do not operate as isolated linear tracks but form a highly interconnected network. The crosstalk between them often dictates the final cellular outcome in response to stress.
JNK and NF-κB: A Delicate Balance
The JNK and NF-κB pathways frequently exhibit antagonistic interactions, particularly in response to TNF-α stimulation. While both pathways can be activated simultaneously, NF-κB activation often serves to temper the pro-apoptotic signal of sustained JNK activation. One mechanism for this antagonism involves NF-κB-dependent transcription of genes that directly inhibit the JNK pathway [91]. Furthermore, a novel crosstalk mechanism has been identified involving the phosphorylation of the small heat shock protein HSP27. JNK-mediated phosphorylation of HSP27 can subsequently influence the NF-κB pathway, creating a bridge that impacts cell survival decisions [94]. The outcome of this interplay is context-dependent; in the absence of NF-κB activation, prolonged JNK signaling strongly promotes apoptosis, whereas effective NF-κB activation can suppress this JNK-mediated cell death [91].
p53 and NF-κB: Convergent and Antagonistic Interactions
The p53 and NF-κB pathways engage in complex cross-regulation. NF-κB can directly influence p53 activity, for instance, by modulating its acetylation status. Conversely, p53 can transcriptionally repress certain NF-κB target genes. This mutual antagonism often creates a "seesaw" effect, where the activation of one pathway suppresses the other, thereby influencing whether a cell initiates an apoptotic or a survival/inflammatory program [93]. The specific outcome is highly dependent on the cellular context and the nature of the stress signal.
p53 and JNK: Cooperative Synergy in Apoptosis
p53 and JNK signaling often converge to promote apoptosis synergistically. JNK can phosphorylate and stabilize p53, thereby enhancing its transcriptional activity and pro-apoptotic function. In turn, p53 contributes to the sustained activation of JNK, creating a positive feedback loop that amplifies the cell death signal. This cooperative interaction is critical for apoptosis induction in response to severe genotoxic stress [91].
Figure 1: Integrated Crosstalk Between JNK, p53, and NF-κB Pathways. This diagram illustrates the core components and major interactions. JNK and p53 often engage in cooperative pro-apoptotic signaling, while NF-κB typically opposes these signals through anti-apoptotic gene expression. Key points of antagonism and modulation, such as via HSP27, are shown.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents for Analyzing Pathway Crosstalk
| Reagent / Tool | Core Function | Example Application |
|---|---|---|
| JNKKTR Biosensor | Live-cell imaging of JNK activity dynamics via nucleocytoplasmic shuttling. | Tracking single-cell JNK activation patterns (sustained, transient, pulsed) in response to stress [90]. |
| shRNA/siRNA (p105/p100) | Gene-specific knockdown of canonical (p105/NF-κB1) and non-canonical (p100/NF-κB2) NF-κB pathways. | Dissecting the specific contribution of each NF-κB pathway to apoptosis resistance [93]. |
| Annexin V / PI Staining | Flow cytometry-based detection of phosphatidylserine externalization (early apoptosis) and membrane integrity (necrosis). | Quantifying the percentage of apoptotic cells after pathway inhibition or activation [93]. |
| Phospho-Specific Antibodies | Detection of activated, phosphorylated signaling components (e.g., phospho-c-Jun Ser73, phospho-JNK). | Validating pathway activation and correlating it with functional outcomes via Western Blot [90] [89]. |
| Caspase Activity Assays | Fluorometric or colorimetric measurement of executioner caspase (e.g., caspase-3/7) cleavage activity. | Assessing the final stages of apoptotic commitment downstream of pathway crosstalk [93]. |
| mCasExpress Mouse Model | Lineage tracing of cells that have experienced Executioner Caspase Activation (ECA) in vivo. | Studying non-lethal caspase functions and their role in processes like liver regeneration [30]. |
The decision between cellular survival and death is orchestrated by a sophisticated dialogue between the JNK, p53, and NF-κB signaling pathways. Rather than functioning in isolation, these pathways form an integrated network where the balance of their synergistic and antagonistic interactions determines the final cellular outcome. The JNK and p53 pathways often collaborate to amplify pro-apoptotic signals, particularly under conditions of severe stress. In stark contrast, the NF-κB pathway typically functions as a powerful survival mechanism, counteracting pro-apoptotic signals by inducing a suite of anti-apoptotic genes and directly engaging in cross-pathway inhibition. The discovery of non-apoptotic roles for executioner caspases, such as their sublethal involvement in promoting liver regeneration via the JAK/STAT3 pathway, further enriches this complex picture, demonstrating that caspase activation can signal for life as well as for death [30]. Understanding the precise molecular mechanisms of this crosstalk—including the role of pathway dynamics, spatial organization, and feedback loops—is not merely an academic pursuit. It provides the essential foundational knowledge required to rationally design novel therapeutic strategies aimed at modulating cell death in diseases such as cancer, chronic inflammation, and neurodegeneration.
Caspases, traditionally recognized as executioners of apoptosis, are now established as master regulators of diverse biological processes beyond cell death. Recent research has illuminated their critical functions in mediating pyroptosis, an inflammatory form of cell death, and in controlling cell cycle dynamics through sublethal activation mechanisms. This whitepaper synthesizes current understanding of caspase functions within these non-apoptotic contexts, detailing molecular mechanisms, experimental validation approaches, and therapeutic implications. By examining the caspase functional continuum—from homeostatic regulation to defensive responses and irreversible remodeling—we provide a framework for researchers investigating caspase cascade activation and executioner functions. The emerging paradigm positions caspases as multifunctional integrators of cellular homeostasis whose functional output is determined by dynamic activity gradients and spatiotemporal localization rather than binary death decisions.
The caspase family of cysteine proteases has undergone a profound conceptual evolution since their initial characterization as apoptotic executioners. While their canonical roles in cleaving cellular substrates to orchestrate programmed cell death remain undisputed, contemporary research reveals a functional spectrum extending far beyond apoptosis. Caspases are now understood to operate along a functional continuum where low-level, sublethal activation regulates fundamental physiological processes including cellular differentiation, immune modulation, and cell cycle progression [26]. This paradigm shift necessitates refined experimental approaches to distinguish between lethal and sublethal caspase functions across different biological contexts.
The classification of caspases has traditionally followed a tripartite division into initiator, executioner, and inflammatory caspases based on structural domains and apoptotic functions. However, a more nuanced framework organized around functional clusters—homeostatic, defensive, and remodeling—better accommodates their diverse non-apoptotic roles [26]. This revised perspective is particularly relevant for understanding how caspases mediate pyroptosis through gasdermin protein cleavage and regulate cell proliferation through sublethal activation states that avoid cell death induction. This technical review provides comprehensive validation methodologies for investigating these non-apoptotic caspase functions, with particular emphasis on their roles in pyroptotic pathways and cell cycle control mechanisms.
Molecular Mechanisms of Caspase-Mediated Pyroptosis
Pyroptosis Execution Pathways
Pyroptosis represents a lytic, proinflammatory form of programmed cell death characterized by plasma membrane pore formation, cell swelling, and release of proinflammatory cytokines and cellular contents [95] [96]. The molecular execution of pyroptosis centers on the gasdermin protein family, which contains an N-terminal cytotoxic domain capable of forming plasma membrane pores and a C-terminal autoinhibitory domain [95] [97]. Proteolytic cleavage within the flexible linker region releases the N-terminal domain, enabling it to oligomerize and insert into cellular membranes where it forms large transmembrane pores [95].
Table 1: Caspase Substrates in Pyroptosis Execution
| Caspase | Gasdermin Substrate | Cleavage Site | Functional Outcome |
|---|---|---|---|
| Caspase-1 | GSDMD | D275 (human) | Canonical inflammasome pathway; pore formation & IL-1β/IL-18 maturation [95] [1] |
| Caspase-4/5/11 | GSDMD | D275 (human) | Non-canonical pathway; direct LPS sensing & pore formation [95] [1] |
| Caspase-3 | GSDME | Multiple sites | Apoptosis-to-pyroptosis switch; chemotherapeutic agent-induced pyroptosis [1] [97] |
| Caspase-8 | GSDMC | Multiple sites | Hypoxic tumor microenvironment; TNF-α-induced pyroptosis [1] [97] |
| Caspase-3/6/7 | GSDMB | D91 | Prevents pyroptotic activation during apoptosis [1] |
| Granzyme A | GSDMB | Non-caspase | Cytotoxic lymphocyte-mediated cancer cell pyroptosis [97] |
The pyroptotic process occurs in two distinct phases: an initial subcellular permeabilization phase where gasdermin-N domains target various organelle membranes, followed by an irreversible cell lysis phase marked by plasma membrane rupture mediated by Ninjurin-1 (NINJ1) [97]. Importantly, gasdermin pore formation can release specific cytokines like IL-1β without immediately inducing cell lysis, demonstrating that pore formation and cell death are separable events [97].
Comparative Pathway Architecture
Caspase Signaling Pathways in Apoptosis vs. Pyroptosis
The diagram illustrates the distinct caspase signaling cascades in apoptosis versus pyroptosis. While apoptotic pathways maintain membrane integrity and avoid inflammation, pyroptotic pathways deliberately induce membrane disruption and proinflammatory mediator release through gasdermin pore formation [95] [98].
Sublethal Caspase Activation in Cell Cycle Control
The Caspase Functional Continuum
Beyond their roles in cell death execution, caspases function as regulatory proteases in living cells through sublethal activation states that cleave specific substrates without triggering apoptosis [26]. This functional continuum model posits that caspase activity exists along a gradient where low-level activation supports homeostatic functions, moderate activation enables defensive responses, and high-level activation initiates cell death programs [26]. The critical determinants of functional outcome include:
- Activity intensity: Concentration and catalytic efficiency of active caspases
- Spatiotemporal localization: Subcellular compartmentalization and substrate accessibility
- Microenvironmental context: pH, redox status, and cofactor availability
- Temporal dynamics: Duration and oscillation frequency of activation
In the context of cell cycle regulation, sublethal caspase activation has been demonstrated to promote hepatocyte proliferation during liver regeneration through the JAK/STAT3 pathway [30]. Transgenic lineage tracing revealed that hepatocytes with executioner caspase activation (ECA) not only survived but proliferated extensively during regeneration, with inhibition of ECA resulting in impaired liver regeneration [30].
Experimental Validation of Sublethal Functions
Caspase Activity Gradient Determining Functional Outcomes
The functional continuum model illustrates how caspase output ranges from physiological regulation to pathological cell death based on activity levels and contextual factors [26]. This model explains how the same caspases can execute diametrically opposed functions in different contexts.
Experimental Methodologies for Caspase Function Validation
Lineage Tracing for Sublethal Caspase Activation
The mCasExpress transgenic mouse system provides a sophisticated methodology for tracking cells that have experienced executioner caspase activation (ECA) without undergoing apoptosis [30]. This lineage tracing approach enables researchers to distinguish between lethal and sublethal caspase functions in complex physiological contexts.
Table 2: mCasExpress System Components and Functions
| Component | Genetic Element | Function |
|---|---|---|
| Inducible Reporter | LSL-rtTA; TRE-Lyn11-NES-DEVD-FLP; FSF-ZsGreen | Doxycycline-dependent expression of caspase-sensitive FLP recombinase [30] |
| Caspase Sensor | Lyn11-NES-DEVD-FLP fusion protein | Membrane-tethered FLP cleaved by active caspase-3/7, releasing nuclear FLP [30] |
| Lineage Marker | CAG-FRT-STOP-FRT-ZsGreen | Permanent ZsGreen expression after FLP-mediated STOP cassette excision [30] |
| Validation Controls | Caspase-3/7 DKO; XIAP/p35 overexpression | Confirms caspase-specific signaling [30] |
Experimental Workflow:
- System Activation: Administer doxycycline (5 mg/kg) via tail vein injection to induce LN-DEVD-FLP expression
- Caspase Activation Window: Allow 3-7 days for caspase activation and ZsGreen expression accumulation
- Lineage Tracing: Track ZsGreen+ cells over time to determine proliferation and fate
- Functional Validation: Modulate caspase activity genetically (XIAP/p35 overexpression) or pharmacologically
In liver regeneration studies, this system demonstrated that approximately 10.7% of hepatocytes experienced ECA by day 7 after partial hepatectomy, with the majority surviving and proliferating rather than undergoing apoptosis [30].
Pyroptosis Induction and Assessment Protocols
Validating caspase roles in pyroptosis requires distinct methodological approaches focused on gasdermin cleavage and pore formation assessment:
Gasdermin Cleavage Detection:
- Western Blot Analysis: Use specific antibodies targeting full-length and cleaved gasdermins (e.g., GSDMD, GSDME)
- Plasma Membrane Binding Assays: Isolate membrane fractions to detect N-terminal gasdermin translocation
- Liposome Permeabilization: Reconstitute gasdermin pores in synthetic membranes with fluorescent dye release readouts
Functional Pyroptosis Assays:
- Lactate Dehydrogenase (LDH) Release: Quantify plasma membrane integrity disruption
- Propidium Iodide Uptake: Measure pore-mediated influx of small molecules
- IL-1β/IL-18 Secretion: ELISA-based quantification of inflammasome-dependent cytokine release
- Electron Microscopy: Visualize membrane pores and cellular ultrastructural changes
Chemical Inducers and Inhibitors:
- Nigericin: K+ ionophore for NLRP3 inflammasome activation
- LPS transfection: Non-canonical inflammasome activation via caspase-4/5/11
- Chemotherapeutic agents (e.g., lobaplatin): Caspase-3-mediated GSDME cleavage
- Disulfiram: Direct GSDMD inhibitor blocking pore formation
Research Reagent Solutions
Table 3: Essential Research Reagents for Caspase Function Studies
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| Caspase Activity Probes | FLICA reagents, DEVD-AMC | Live-cell caspase activity quantification [30] |
| Transgenic Model Systems | mCasExpress mice, Caspase KO mice | Lineage tracing of caspase activation in vivo [30] |
| Gasdermin Antibodies | Anti-GSDMD, Anti-GSDME, Anti-GSDMC | Cleavage detection and cellular localization [95] [97] |
| Inflammasome Activators | Nigericin, Poly(dA:dT), ATP, LPS | Pathway-specific pyroptosis induction [95] [97] |
| Caspase Inhibitors | Z-VAD-FMK (pan-caspase), Ac-DEVD-CHO (caspase-3) | Activity validation and functional blocking [30] |
| Cytokine Detection | IL-1β ELISA, IL-18 bioassays | Inflammasome activity and pyroptosis readouts [95] [97] |
Therapeutic Implications and Research Perspectives
The expanding understanding of non-apoptotic caspase functions opens new therapeutic avenues across multiple disease contexts. In oncology, inducing pyroptosis in cancer cells represents a promising strategy to overcome apoptosis resistance and stimulate antitumor immunity [97]. Therapeutically, caspase-mediated pyroptosis can transform "cold" tumors into "hot" tumors by releasing DAMPs that activate dendritic cells and enhance cytotoxic lymphocyte infiltration [97]. Clinical evidence shows that elevated expression of pyroptosis-related molecules correlates with more immunogenic tumor microenvironments and improved chemotherapeutic responses in cancer patients [97].
Beyond oncology, modulating the caspase functional continuum offers potential for treating neurodegenerative disorders, inflammatory conditions, and metabolic diseases. The development of activity gradient-based therapeutics represents a frontier in precision medicine, where interventions aim to tune caspase activity to optimal levels rather than complete inhibition or activation [26]. Conformation-specific inhibitors that selectively block pathological caspase functions while preserving physiological roles exemplify this approach [26].
Future research directions should focus on:
- Developing advanced biosensors for real-time monitoring of caspase activity gradients in living cells and organisms
- Elucidating the molecular mechanisms governing caspase substrate selectivity at different activity thresholds
- Exploring tissue-specific and context-dependent regulation of caspase functions
- Designing therapeutic strategies that precisely modulate caspase activity within the functional continuum
The traditional paradigm of caspases as mere executioners of apoptosis has been fundamentally transformed by contemporary research demonstrating their multifunctional roles in pyroptosis and cell cycle regulation. The validation approaches outlined in this technical review provide researchers with comprehensive methodologies for investigating these diverse caspase functions within the framework of the caspase functional continuum. As our understanding of caspase biology continues to evolve, the strategic manipulation of their activity gradients and spatiotemporal localization offers promising therapeutic potential for cancer, inflammatory diseases, and regenerative medicine. The ongoing challenge for researchers remains the development of increasingly precise tools to dissect and modulate the complex caspase networks that integrate cellular homeostasis, defense mechanisms, and programmed remodeling.
Conclusion
The caspase cascade represents a sophisticated and tightly regulated system central to cellular homeostasis, with its executioner functions serving as the final, irreversible step in apoptotic demise. Research has firmly established that while core activation mechanisms are conserved, significant complexity arises from functional redundancies, non-apoptotic functions, and intricate cross-talk with other vital signaling networks. The paradoxical role of caspases, where their activation can sometimes lead to unintended pro-survival outcomes as seen in radiotherapy, underscores the necessity for a nuanced understanding in therapeutic development. Future research must focus on delineating the precise substrate profiles of individual caspases, developing highly specific pharmacological modulators, and exploiting the differential regulation of caspase activity in diseased versus healthy tissues. The continued integration of foundational knowledge with advanced methodological and comparative analyses will be paramount in successfully translating caspase biology into next-generation therapies for cancer, neurodegenerative diseases, and autoimmune disorders.
References
- 1. Caspases as master regulators of programmed cell death [https://pmc.ncbi.nlm.nih.gov/articles/PMC12229594/]
- 2. structural and molecular mechanisms and functions in cell ... [https://www.nature.com/articles/s41421-025-00791-3]
- 3. Caspase Functions in Cell Death and Disease - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3683896/]
- 4. - Wikipedia Caspase [https://en.wikipedia.org/wiki/Caspase]
- 5. Death and survival from executioner caspase activation [https://www.sciencedirect.com/science/article/abs/pii/S108495212300143X]
- 6. in cell Caspases , death and disease - PMC inflammation [https://pmc.ncbi.nlm.nih.gov/articles/PMC6611727/]
- 7. A long way to go: caspase inhibitors in clinical use [https://www.nature.com/articles/s41419-021-04240-3]
- 8. Ventus Therapeutics Announces Nature Reviews ... [https://www.businesswire.com/news/home/20250305537053/en/Ventus-Therapeutics-Announces-Nature-Reviews-Immunology-Publication-Demonstrating-the-Promise-of-Caspase-45-as-Therapeutic-Targets]
- 9. Converging roles of caspases in inflammasome activation, cell death ... [https://www.nature.com/articles/nri.2015.7?error=cookies_not_supported&code=342f56d4-1c8c-483f-aeb3-548d1502af6b]
- 10. 10 things you wish you knew about inflammatory caspases [https://pmc.ncbi.nlm.nih.gov/articles/PMC12550167/]
- 11. Crystal Structure of Procaspase-1 Zymogen Domain Reveals ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2649088/]
- 12. Caspases: structural and molecular mechanisms and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12052993/]
- 13. Crystal structure of procaspase-1 zymogen domain reveals ... [https://pubmed.ncbi.nlm.nih.gov/19117953/]
- 14. Executioner caspase is proximal to Fasciclin 3 which ... [https://elifesciences.org/articles/99650]
- 15. Structure and function of the human apoptotic scramblase ... [https://www.nature.com/articles/s41467-025-62739-1]
- 16. Mechanisms of caspase activation [https://www.sciencedirect.com/science/article/abs/pii/S0955067403001364]
- 17. Caspase Activation and Inhibition - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC9341465/]
- 18. Caspase 3-specific cleavage of ubiquitin ... [https://pubmed.ncbi.nlm.nih.gov/39878157/]
- 19. Caspase 3-specific cleavage of ubiquitin- ... [https://mdanderson.elsevierpure.com/en/publications/caspase-3-specific-cleavage-of-ubiquitin-specific-peptidase-48-en/]
- 20. Apoptosis [https://en.wikipedia.org/wiki/Apoptosis]
- 21. Caspases: the executioners of apoptosis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1218630/]
- 22. Quantitative analysis of pathways controlling extrinsic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2858979/]
- 23. From computational modelling of the intrinsic apoptosis ... [https://www.nature.com/articles/cddis201436]
- 24. Apoptosis Assay Market Size Report, 2025 – 2034 [https://www.gminsights.com/industry-analysis/apoptosis-assay-market]
- 25. Targeting apoptotic pathways for cancer therapy [https://www.jci.org/articles/view/179570]
- 26. The multifunctionality of the caspase family of proteases [https://www.sciencedirect.com/science/article/abs/pii/S0098299725000755]
- 27. Caspases as master regulators of programmed cell death [https://www.nature.com/articles/s12276-025-01470-9]
- 28. SPR imaging-based monitoring of caspase-3 activation [https://www.sciencedirect.com/science/article/abs/pii/S0006291X08001964]
- 29. Beclin 1 cleavage by caspase-3 inactivates autophagy and ... [https://pubmed.ncbi.nlm.nih.gov/21203962/]
- 30. Sublethal executioner caspase activation in hepatocytes ... [https://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.3003357]
- 31. Efficient apoptosis requires feedback amplification of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6669006/]
- 32. Caspase-2 Deficiency Enhances Aging-Related Traits in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1828128/]
- 33. Caspase-8 deficiency in mouse embryos triggers chronic ... [https://www.nature.com/articles/s41418-018-0104-9]
- 34. Caspase-8 deficiency induces a switch from TLR3 ... [https://www.nature.com/articles/s41598-021-89793-1]
- 35. A Comprehensive Exploration of Caspase Detection Methods [https://www.mdpi.com/1422-0067/25/10/5460]
- 36. Protocol for measuring the caspase-8 activity at the DED ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12539301/]
- 37. A Guide to Modern Quantitative Fluorescent Western ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4354265/]
- 38. Integrated real-time imaging of executioner caspase ... [https://www.nature.com/articles/s41420-025-02662-y]
- 39. Current applications of antibody microarrays - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5830343/]
- 40. Apoptosis Protein Arrays [https://www.raybiotech.com/applications/cardiovascular-disease/apoptosis]
- 41. Proteome analysis of apoptotic cells [https://pubmed.ncbi.nlm.nih.gov/15264233/]
- 42. Quantification of relevant metabolites in apoptotic bodies ... [https://www.sciencedirect.com/science/article/pii/S0003267024009917]
- 43. Apoptotic proteome profiling [https://bio-protocol.org/exchange/minidetail?id=7943401&type=30]
- 44. Reactivating apoptotic pathways in cancer: A review of ... [https://www.sciencedirect.com/science/article/abs/pii/S0014299925007198]
- 45. Anti-apoptotic PROTACs in Cancer Therapy: A Review [https://esmed.org/anti-apoptotic-protacs-in-cancer-therapy-a-review/]
- 46. Isoginkgetin Induces Caspase Cascade Activation and ... [https://www.jcancer.org/v16p4415.htm]
- 47. Isoginkgetin, a Natural Biflavonoid Proteasome Inhibitor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6497994/]
- 48. Ginkgetin from Ginkgo biloba: mechanistic insights into ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12325161/]
- 49. Isoginkgetin exerts apoptotic effects on A375 melanoma cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC11461025/]
- 50. RAD51 modulates in nasopharyngeal carcinoma cells by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12255641/]
- 51. Mechanisms of radioresistance and radiosensitization ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11964565/]
- 52. Molecular mechanisms of tumor resistance to radiotherapy [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-023-01801-2]
- 53. Caspase-12 exhibits non-redundant functions in response ... [https://www.sciencedirect.com/science/article/pii/S193152442500026X]
- 54. The role of BCL-2 family proteins in regulating apoptosis and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9597512/]
- 55. The BCL2 family: from apoptosis mechanisms to new ... [https://www.nature.com/articles/s41392-025-02176-0]
- 56. The Immuno-Modulatory Effects of Inhibitor of Apoptosis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7017284/]
- 57. The interplay between the Bcl-2 family and death receptor- ... [https://www.sciencedirect.com/science/article/pii/S0167488903001794]
- 58. The Bcl-2-regulated apoptosis switch: mechanism and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2754308/]
- 59. Targeting the inhibitors of apoptosis proteins (IAPs) to ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1562167/full]
- 60. Paradoxical roles of caspase-3 in regulating cell survival ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9106709/]
- 61. Cellular Mechanisms Controlling Caspase Activation and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3660825/]
- 62. Caspase Cascade pathway [https://www.abeomics.com/caspase-cascade]
- 63. Caspase-7: a protease involved in apoptosis and inflammation [https://pmc.ncbi.nlm.nih.gov/articles/PMC2787741/]
- 64. Caspase-3 Is Required for DNA Fragmentation and ... [https://www.sciencedirect.com/science/article/pii/S002192581846139X]
- 65. The proteolytic landscape of cells exposed to non-lethal ... [https://www.nature.com/articles/s41420-021-00539-4]
- 66. The concealed side of caspases: beyond a killer of cells [https://link.springer.com/article/10.1007/s00018-024-05495-7]
- 67. Physiological functions of non-apoptotic caspase activity in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5988915/]
- 68. Non-Canonical Roles of Apoptotic Caspases in the ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2022.840023/full]
- 69. Multiple entanglements of different cell death pathways, in ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1667611/full]
- 70. Caspases and therapeutic potential of caspase inhibitors in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8222863/]
- 71. structural and molecular mechanisms and functions in cell ... [https://pubmed.ncbi.nlm.nih.gov/40325022/]
- 72. Caspase-8 in inflammatory diseases: a potential therapeutic ... [https://cmbl.biomedcentral.com/articles/10.1186/s11658-024-00646-x]
- 73. Caspases and Their Substrates - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8886984/]
- 74. Executioner caspase-3 and caspase-7 are functionally distinct ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2529079/]
- 75. Caspases and their substrates | Cell Death & Differentiation [https://www.nature.com/articles/cdd201744]
- 76. Executioner caspases degrade essential mediators of ... [https://pubmed.ncbi.nlm.nih.gov/39885151]
- 77. Caspase-9: structure, mechanisms and clinical application [https://pmc.ncbi.nlm.nih.gov/articles/PMC5410359/]
- 78. Individual caspase-10 isoforms play distinct and opposing ... [https://www.nature.com/articles/cddis20118]
- 79. Caspase-10 Negatively Regulates Caspase-8-Mediated ... [https://www.sciencedirect.com/science/article/pii/S2211124717304850]
- 80. Evolutionary and Functional Analysis of Caspase-8 and ASC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12066828/]
- 81. Functions of Caspase 8: the Identified and the Mysterious [https://pmc.ncbi.nlm.nih.gov/articles/PMC4099255/]
- 82. Caspase-10 is recruited to and activated at the native ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC126181/]
- 83. The molecular mechanism of apoptosis upon caspase-8 ... [https://www.sciencedirect.com/science/article/pii/S0167488912001991]
- 84. Exploring caspase functions in mouse models - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11263464/]
- 85. A Comprehensive Exploration of Caspase Detection Methods [https://pmc.ncbi.nlm.nih.gov/articles/PMC11121653/]
- 86. Exploring caspase functions in mouse models | Apoptosis [https://link.springer.com/article/10.1007/s10495-024-01976-z]
- 87. Caspase activation pathways: some recent progress [https://www.nature.com/articles/cdd200959]
- 88. A CARD9 deficiency mouse model recapitulates human ... [https://pubmed.ncbi.nlm.nih.gov/40424070/]
- 89. JNK Signaling in Apoptosis - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC3063296/]
- 90. JNK activation dynamics drive distinct gene expression ... [https://www.nature.com/articles/s41540-025-00590-2]
- 91. Role of JNK activation in apoptosis: A double-edged sword [https://www.nature.com/articles/7290262]
- 92. Tumor Suppressor p53: Biology, Signaling Pathways, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8730328/]
- 93. The role of NF-κB-1 and NF-κB-2-mediated resistance to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1482593/]
- 94. Crosstalk between JNK and NF-κB signaling pathways via ... [https://www.sciencedirect.com/science/article/abs/pii/S0006291X14020579]
- 95. Pyroptosis: molecular mechanisms and roles in disease [https://www.nature.com/articles/s41422-025-01107-6]
- 96. role of pyroptosis in revolutionizing thyroid cancer care - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12501357/]
- 97. Manipulation of cancer cell pyroptosis for therapeutic ... [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-025-00771-5]
- 98. What is the difference between pyroptosis and apoptosis? [https://www.ptglab.com/news/blog/what-is-the-difference-between-pyroptosis-and-apoptosis/?srsltid=AfmBOopMFL67qEHJ6XXV-bJjuMLPaNcpIghViu_JAKf0nP1q68oE6Lyh]